Abstract
Abstract 1040
Secondary acute myeloid leukemia (sAML) is a heterogeneous disease classification comprising patients (pts) with a history of myelodysplastic syndromes (MDS) or myeloproliferative neoplasms (MPN) and pts with prior exposure to chemotherapy or radiation. Though sAML pts typically have lower complete remission (CR) and worse overall survival (OS) rates with induction chemotherapy, it is unknown whether pts with antecedent CBC abnormalities but without formal hematologic diagnoses prior to AML display similar poor outcomes.
We retrospectively evaluated all pts with newly diagnosed, pathologically-confirmed AML treated with cytarabine-based induction chemotherapy at a single institution between 1997 and 2008 to identify both those with known antecedent hematologic disorders and those with antecedent CBC abnormalities irrespective of preceding myeloid diagnosis. sAML was classified as AML from MDS, AML from MPN, and therapy-related AML (t-AML); these groups were compared to pts classified as de novo AML with antecedent CBC abnormalities using univariate and multivariate regression analyses and recursive partitioning to determine cut-points. A CBC abnormality was defined as persistent white blood cell count (WBC) <3.5 or >12 k/uL, hemoglobin <10 or >16 g/dL, or platelet count <100 or >500 k/uL.
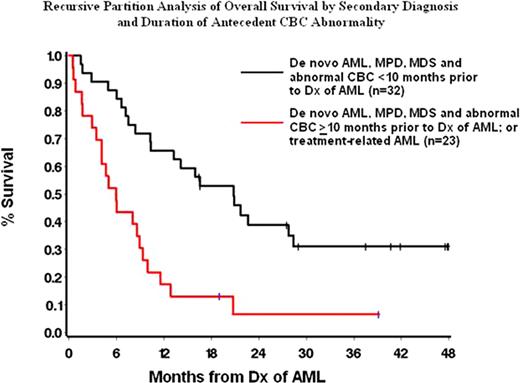
Of 413 AML pts who received induction chemotherapy, 140 were identified with sAML or antecedent CBC abnormalities; 46 (33%) had t-AML, 41 (29%) had AML from MDS, 23 (16%) had AML from MPN, and 30 (21%) had de novo AML with an antecedent CBC abnormality. The median age at AML diagnosis was 62 years (range 24–77) and differed among groups (MDS 67 years, MPN 61, t-AML 80, and de novo 62, p=.003); 49% were male. Overall, the median time from identification of a CBC abnormality to AML diagnosis was 5 months (range 2–83). The time from preceding event to sAML differed among groups (MDS 7 months, MPN 50, t-AML 53, p<.001). Unfavorable risk cytogenetics were more frequent in MDS (44%) and MPN (42%) than in t-AML (26%) or de novo (27%, p=.008). Median presenting WBC differed among groups (MDS 4.0 k/uL, MPN 9.9, t-AML 6.9, de novo with antecedent CNC abnormalities 2.7, p=.02). Among pts with de novo AML with antecedent CBC abnormalities, 18 (60%) had abnormal WBCs, 13 (43%) had anemia, and 8 (27%) had thrombocytopenia; 7 (23%) had multilineage cytopenias. Univariable analysis of CR rates among sAML pts without an antecedent CBC abnormality identified age <60 (71% vs 50% in age ≥ 60, p=.02), unfavorable cytogenetics (28% vs 75% in intermediate or favorable, p<.0001), and AML precursor (34% in MDS, 61% in MPS, and 65% in t-AML, p=.002) as significant factors. t-AML also exhibited better OS compared to prior MDS (hazard ratio [HR] 2.40, 95% confidence interval [CI] 1.38–4.19, p=.002) or MPN (HR 1.84, 95% CI 0.95–3.56, p=.07). In multivariable analysis, unfavorable cytogenetics (p=.0001) and prior MDS or MPN (vs t-AML) (HR 1.83, 95% CI 1.04–4.05), p=.04) were prognostic for worse OS. However, when an antecedent CBC abnormality was identified (n=55), t-AML exhibited poorer OS compared to prior MDS (p=.04) and de novo AML with a CBC abnormality (HR 4.79, 95% CI 1.95–11.77, p=.001). Pts whose CBC abnormality was present for ≥10 months prior to AML diagnosis had poorer OS than those for whom it was present <10 months (HR 2.06, 95% CI 1.08–3.93, p=.03), controlling for factors such as age and cytogenetics. By recursive partition analysis, pts with prior MDS, prior MPN, or de novo AML with CBC abnormality of fewer than 10 months had significantly longer median OS (20.8 months) than those with a CBC abnormality of greater than 10 months or with t-AML regardless of duration of CBC abnormality (5.9 months, HR 3.27, 95% CI 1.73–6.20, p=.0003) (Figure 1), and also exhibited higher CR rate to induction chemotherapy (78% vs 39%, p=.005).
The presence of an antecedent CBC abnormality of greater than 10 months in both de novo and sAML patients negatively impacts CR and OS following induction chemotherapy. These pts should be considered for alternative therapeutic approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal