Abstract
Abstract 2300
Imatinib mesylate (Gleevec) treatment for Chronic Myelogenous Leukemia (CML) was first introduced in Brazil in 2003, initially used as second line therapy for patients resistant or intolerant to interferon. In 2004 imatinib was adopted as front-line therapy for chronic phase (CP) and clinical experience improving since then. Close monitoring of responses achievement at scheduled time has proven to provide good predictive value for progression and event-free survival. Failure and sub-optimal responses correspond to indications for dose change or therapy switching and the identification of patients at greater risk for such events has a vital role. The aim of this study is to evaluate the impact of temporary imatinib therapy discontinuation on achievement of Major Cytogenetic Response (MCyR) and event-free survival (EFS).
During the period of 1990 to 2010 a total of 185 patients from 7 CML treatment centers from Rio Grande do Sul, south Brazil, with a confirmed diagnosis of CML (Philadelphia chromosome positive [Ph+]) at CP under imatinib treatment were retrospectively analyzed. A major cytogenetic response was considered complete plus partial cytogenetic responses (Ph+ less than 35%). At least 20 metaphases were analyzed for a cytogenetic response to be evaluable. Temporary treatment discontinuation (TTD) corresponds to 20 days or more off-medication for any reason during the follow-up. Were included patients in imatinib second-line and first-line therapy. Early-imatinib treatment was considered when imatinib started before 12 months from diagnosis and late-imatinib treatment when more then 12 months lapse. EFS was measured from the start of imatinib to the date of any the following events while on therapy: death of any cause, therapy failure, any response loss, disease progression, definitive treatment discontinuation or therapy change. Descriptive statistics and Kaplan-Meier analysis (to estimate event-free survival [EFS]) were performed using SPSS software.
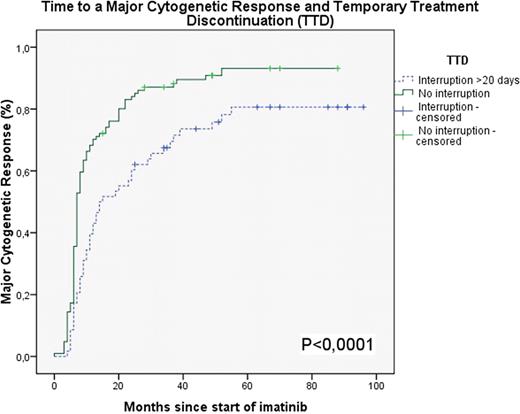
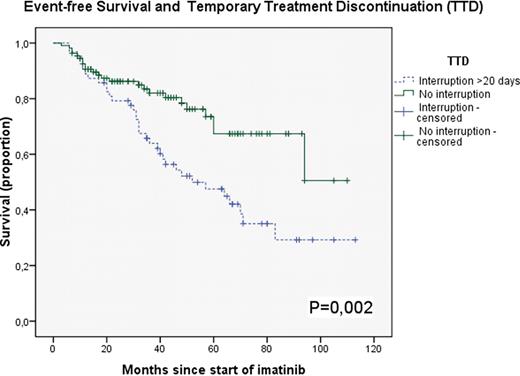
The median age at diagnosis was 48 years (range, 4–85 years) median of follow-up was 47 months (range, 7–113 months) and 55% of male sex. Preferential previous treatment was interferon in 70% of the patients and 71% were early-imatinib treatment. TTD was observed in 63/185 patients (34%) and was related to toxicities in 35/63 patients (55%), including hematological and non-hematological. Nonadherence was attributed to the remaining TTD, 28/63 patients (44%). Late-imatinib patients had significant more TTD (62%) than early-imatinib patients (26,2% [p<0,001]). Subgroup analyzes showed that was a significant TTD rate due to toxicity in the late-imatinib patients (p=0,03), but not significant due to nonadherence (p=0,37). Patients who experienced TTD had lower proportion of MCyR at 12 months: only 43% compared to 70% of patients who did not had TTD (p<0,001 [Figure 1]). Finally the TTD had a relevant negative impact on EFS in 5 years. In the group who had TTD EFS was 47,5%, compared with 73% in the group without TTD (p=0,002 Figure 2).
In our cohort, patients with TTD were associated with lower rate of MCyR and it may be a risk factor for failure or sub-optimal responses to imatinib therapy. TTD also has a negative effect in terms of EFS in patients under imatinib treatment, possibly related to worsen cytogenetic disease control. The late onset of imatinib therapy correlates with more toxicity leading to treatment interruptions and front-line imatinib therapy should be started as soon as possible. Special attention should be given to patients who presents with side effects of any nature that could preclude the correct use of the medication. Close monitoring and early management of such adverse reactions, frequent assessment of compliance should be warrant as effort to guarantee the best chance for therapy success.
Major Cytogenetic Response according to Temporary Treatment Interruption
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal