Abstract
Abstract 3466
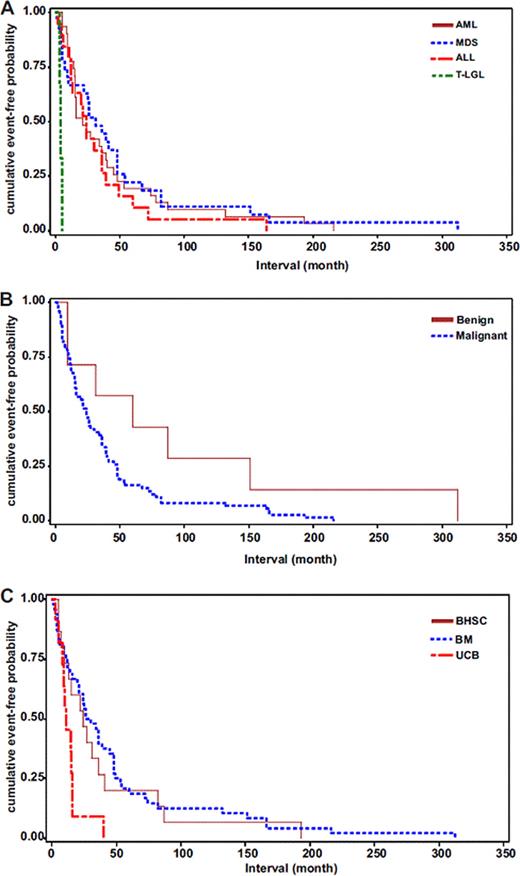
Donor cell leukemia (DCL) in the setting of bone marrow/hematopoietic stem cell transplant (HCT) has not been well characterized. We analyzed 9 cases of DCL and performed a literature review (table). The indications for transplant and subtypes of DCL are shown (table). The 6 myelodysplastic syndrome (MDS) cases included 1 case of refractory cytopenia with multilineage dysplasia (RCMD), 2 cases of refractory anemia and 3 cases which were unclassifiable. Conventional cytogenetic analysis was performed on all 9 cases of DCL (table). All 9 cases had engraftment studies performed either by short tandem repeat analysis (3) or FISH analysis for donor gonosomal complement (6) when DCL was diagnosed. Seven cases had either engraftment studies or cytogenetic analysis performed periodically after HCT to test the donor cell engraftment and engraftment was confirmed in all. FISH analysis for monosomy 7, del(7q) and del(5q) was retrospectively performed on preserved donor cells in 4 cases after DCL was diagnosed. A low level of abnormalities was observed in preserved donor cells for the cases with del(7q) (2.9%) and del(5q) (8.2%). The 2 cases of AML received chemotherapy. Of the MDS cases, 2 received donor cell infusion, 1 received 6 cycles of revlimid, and 3, along with the case of CLL, received either supportive therapy or were simply observed. Six cases have clinical follow up ≥ 5 months and of these, 1 died of disease (AML) while the other 5 are alive, including 4 MDS and the 1 CLL. The disproportionate detection of DCL in sex mismatched HCT suggests a probable under-detection in the sex-matched population. In our analysis, the interval between HCT and diagnosis of DCL (table) falls within the range of currently reported cases. When stratified by type of DCL, the T-LGL group demonstrates presentation significantly earlier than other groups (Fig. A), indicating pathogenesis of T-LGL may involve a distinct pathway. When stratified by types of primary disease, the interval of the neoplastic group is shorter than that of benign group (Fig. B), implying that pre-HCT treatment may play a role in the pathogenesis of DCL. When stratified by stem cell sources, UCB group shows shorter latency than the other sources (Fig. C), suggesting a higher risk of DCL in this cell source. The low level cytogenetic abnormalities of preserved donor cells in our series and the longer latency of the benign group suggest that donor cells with an intrinsic defect may be predisposed to evolve into DCL.
| . | Total cases (%) . | Reported cases (%) . | Current cases (%) . |
|---|---|---|---|
| Number of cases | 83 | 74 | 9 |
| Age (years) | |||
| Median/range | 37.0/3~70 | 36.0/4~62 | 53.0/3~70 |
| Gender | |||
| Male | 43 (52.4) | 38 (52.0) | 5 (55.6) |
| Female | 39 (47.6) | 35 (48.0) | 4 (44.4) |
| Primary disease | |||
| Neoplasms | 76 (91.6) | 67 (90.5) | 9 (100) |
| Non-neoplasms | 7 (8.4) | 7 (9.5) | 0 (0.0) |
| Donor | |||
| Related | 59 (72.0) | 54 (74.0) | 5 (55.6) |
| Unrelated | 23 (28.0) | 19 (26.0) | 4 (44.4) |
| Sex-matched | 28 (34.6) | 27 (37.5) | 1 (11.1) |
| Sex-mismatched | 53 (65.4) | 45 (62.5) | 8 (88.9) |
| Donor cell source | |||
| BM | 48 (63.2) | 44 (65.7) | 4 (44.4) |
| BHSC | 16 (21.0) | 13 (19.4) | 3 (33.3) |
| UCB | 12 (15.8) | 10 (14.9) | 2 (22.2) |
| 2nd neoplasm (DCL) | |||
| AML | 31 (37.4) | 29 (39.2) | 2 (22.2) |
| MDS/MPN* | 27 (32.5) | 21 (28.4) | 6 (66.7) |
| ALL | 20 (24.1) | 20 (27.0) | 0 (0.0) |
| T-LGL | 4 (4.8) | 4 (5.4) | 0 (0.0) |
| CLL | 1 (1.2) | 0 (0.0) | 1 (11.1) |
| Interval (months) | |||
| Median/range | 24.0/1~312 | 24.0/2~312 | 26.0/1~193 |
| Cytogenetics | |||
| Normal | 21 (28.0) | 20 (30.3) | 1 (11.1) |
| Abnormal | 54 (72.0) | 46 (69.7) | 8 (88.9) |
| -7 or del(7q)** | 15 (27.8) | 10 (21.7) | 5 (62.5) |
| +8** | 2 (3.7) | 2 (4.4) | 0 (0.0) |
| Del(20)** | 4 (7.4) | 2 (4.4) | 2 (25.0) |
| Del(5q)** | 2 (3.7) | 1 (2.2) | 1 (12.5) |
| 11q23** | 3 (5.6) | 3 (6.5) | 0 (0.0) |
| Other abnormalities** | 28 (51.9) | 28 (60.9) | 0 (0.0) |
| Follow up (months) | |||
| Median/range | 8.5/1~108 | 9.0/1~108 | 6.0/1~68 |
| Died of disease | 28 (46.7) | 27 (52.9) | 1 (11.1) |
| . | Total cases (%) . | Reported cases (%) . | Current cases (%) . |
|---|---|---|---|
| Number of cases | 83 | 74 | 9 |
| Age (years) | |||
| Median/range | 37.0/3~70 | 36.0/4~62 | 53.0/3~70 |
| Gender | |||
| Male | 43 (52.4) | 38 (52.0) | 5 (55.6) |
| Female | 39 (47.6) | 35 (48.0) | 4 (44.4) |
| Primary disease | |||
| Neoplasms | 76 (91.6) | 67 (90.5) | 9 (100) |
| Non-neoplasms | 7 (8.4) | 7 (9.5) | 0 (0.0) |
| Donor | |||
| Related | 59 (72.0) | 54 (74.0) | 5 (55.6) |
| Unrelated | 23 (28.0) | 19 (26.0) | 4 (44.4) |
| Sex-matched | 28 (34.6) | 27 (37.5) | 1 (11.1) |
| Sex-mismatched | 53 (65.4) | 45 (62.5) | 8 (88.9) |
| Donor cell source | |||
| BM | 48 (63.2) | 44 (65.7) | 4 (44.4) |
| BHSC | 16 (21.0) | 13 (19.4) | 3 (33.3) |
| UCB | 12 (15.8) | 10 (14.9) | 2 (22.2) |
| 2nd neoplasm (DCL) | |||
| AML | 31 (37.4) | 29 (39.2) | 2 (22.2) |
| MDS/MPN* | 27 (32.5) | 21 (28.4) | 6 (66.7) |
| ALL | 20 (24.1) | 20 (27.0) | 0 (0.0) |
| T-LGL | 4 (4.8) | 4 (5.4) | 0 (0.0) |
| CLL | 1 (1.2) | 0 (0.0) | 1 (11.1) |
| Interval (months) | |||
| Median/range | 24.0/1~312 | 24.0/2~312 | 26.0/1~193 |
| Cytogenetics | |||
| Normal | 21 (28.0) | 20 (30.3) | 1 (11.1) |
| Abnormal | 54 (72.0) | 46 (69.7) | 8 (88.9) |
| -7 or del(7q)** | 15 (27.8) | 10 (21.7) | 5 (62.5) |
| +8** | 2 (3.7) | 2 (4.4) | 0 (0.0) |
| Del(20)** | 4 (7.4) | 2 (4.4) | 2 (25.0) |
| Del(5q)** | 2 (3.7) | 1 (2.2) | 1 (12.5) |
| 11q23** | 3 (5.6) | 3 (6.5) | 0 (0.0) |
| Other abnormalities** | 28 (51.9) | 28 (60.9) | 0 (0.0) |
| Follow up (months) | |||
| Median/range | 8.5/1~108 | 9.0/1~108 | 6.0/1~68 |
| Died of disease | 28 (46.7) | 27 (52.9) | 1 (11.1) |
DCL, donor cell leukemia; BM, bone marrow; BHSC, blood hematopoietic stem cells; UCB, umbilical cord blood; AML, acute myeloid leukemia; MDS, myelodysplastic syndrome; ALL, acute lymphoblastic leukemia (including B-cell and T-cell ALL); T-LGL, T-cell large granular lymphocyte leukemia; CLL, chronic lymphocytic leukemia. All the numbers represent the cases with data available.
One case of myeloproliferative neoplasm is included in this category.
The percentage is calculated using number of total cytogenetic abnormalities in each column as denominator.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal