Abstract
Abstract 3493
An increased risk for GvHD, infections and liver toxicity after transplant has been attributed to iron overload (defined by serum ferritin) of MDS and AML patients prior to allogeneic hematopoietic stem cell transplantation (allo-HSCT). Nevertheless, the reason for this observation is not very well defined. Consequently, there is a debate whether to use iron chelators in these patients prior to allo-HSCT. In fact, serum ferritin levels and transfusion history are commonly used to guide iron depletion strategies. Both parameters may inadequately reflect body iron stores in MDS and AML patients prior to allo-HSCT. Recently, quantitative magnetic resonance imaging (MRI) was introduced as a tool for direct measurement of liver iron. We therefore aimed at evaluating the accurateness of different strategies for determining iron overload in MDS and AML patients prior to allo-HSCT.
Serologic parameters of iron overload (ferritin, iron, transferrin, transferrin saturation, soluble transferrin receptor) and transfusion history were obtained prospectively in MDS or AML patients prior to allo-SCT. In parallel, liver iron content was measured by MRI according to the method described by Gandon (Lancet 2004) and Rose (Eur J Haematol 2006), respectively.
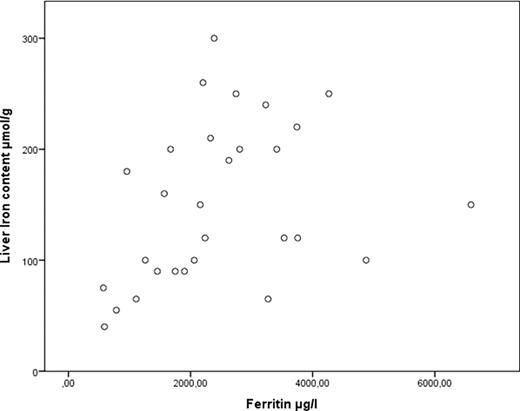
A total of 20 AML and 9 MDS patients (median age 59 years, range: 23–74 years) undergoing allo-HSCT have been evaluated so far. The median ferritin concentration was 2237 μg/l (range 572–6594 μg/l) and patients had received a median of 20 transfusions (range 6–127) before transplantation. Serum ferritin was not significantly correlated with transfusion burden (t = 0.207, p = 0.119) but as expected with the concentration of C-reactive protein (t = 0.385, p = 0.003). Median liver iron concentration measured by MRI was 150 μmol/g (range 40–300 μmol/g, normal: < 36 μmol/g). A weak but significant correlation was found between liver iron concentration and ferritin (t = 0.354; p = 0.008). The strength of the correlation was diminished by the influence of 5 outliers with high ferritin concentrations but rather low liver iron content (Figure 1). The same applied to transfusion history which was also only weakly associated with liver iron content (t = 0.365; p = 0.007). Levels of transferrin, transferrin saturation, total iron and soluble transferrin receptor did not predict for liver iron concentration.
Our data suggest that serum ferritin or transfusion history cannot be regarded as robust surrogates for the actual iron overload in MDS or AML patients. Therefore we advocate caution when using one of these parameters as the only trigger for chelation therapy or as a risk-factor to predict outcome after allo-HSCT.
Correlation of Liver iron content with Ferritin.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal