Abstract
Abstract 3536
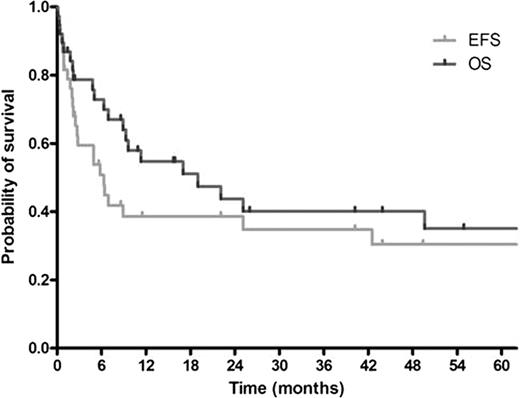
Prognosis of patients with NHL who underwent relapse or progression after autoSCT is generally dismal and treatment option is limited. AlloSCT has been performed to overcome this problem and long term survivors have been reported. However, substantial transplant-related mortality (TRM) is a significant problem. We report clinical outcomes of alloSCT in these patients and DLI after failure of alloSCT along with analysis of risk factors for treatment results and adverse events. This retrospective study was performed in 7 hospitals in Korea. Candidate risk factors were age, sex, histology, Ann Arbor stage at diagnosis, number of prior treatments, time to progression (TTP) after autoSCT, bone marrow involvement, Eastern Cooperative Oncology Group (ECOG) performance status (PS), donor type, stem cell source, conditioning regimens of alloSCT, serum lactate dehydrogenase (above 250 IU/L), serum albumin (above 3.0 g/dL), and acute graft-versus-host disease (aGvHD). Between August 1998 and March 2009, 38 patients received alloSCT. Median age was 37 (range, 17–54) years. Male to female ratio was 26:12. Eighteen patients (47.4%) had B-cell lymphoma and 20 patients (52.6%), T/NK-cell lymphoma. Before alloSCT, patients had received median 4 (range, 2–7) prior treatments including autoSCT. Median TTP after autoSCT was 5.9 (range, 0.8–35.8) months. Twenty four patients (63.2%) received stem cells from related donors and 14 patients (36.8%) from unrelated donors. Median number of CD34+ cells infused was 5.41 × 106 (range, 0.86 × 106-16.60 × 106) /kg. Eighteen patients (47.4%) underwent a myeloablative conditioning and 20 patients (52.6%), a reduced intensity conditioning. During a median follow-up of 45.2 (range, 1.3–137.1) months, 24 patients (63.2%) experienced treatment failure and 22 patients (57.9%) died. Median event-free survival (EFS) was 6.3 (95% confidence interval (CI), 4.3–8.4) months. Median overall survival (OS) was 19.0 (95% CI, 3.8–34.2) months. Estimated 5-year survival rate was 35.0% (Figure). Treatment response was evaluable in 30 patients. Response rate was 73.3%; complete remission (CR) was achieved in 20 patients (66.7%) and partial response in 2 patients (6.7%). Grade 3 or 4 renal toxicity developed in 6 patients (15.8%), grade 3 or 4 hepatic toxicity in 15 patients (39.5%) including veno-occlusive disease (VOD) in 6 patients (15.8%), aGvHD in 13 patients (34.2%), and neutropenic fever in 34 patients (89.5%) including documented sepsis in 11 patients (28.9%). TRM was reported in 8 patients (21.1%). Causes of TRM were infection in 7 patients and VOD in 1 patient. In univariate analysis, no significant association was found with treatment response. By contrast, EFS was related to stage (p=0.039), TTP after autoSCT (p=0.033), and PS (p<0.001). OS was associated with stage (p=0.037), number of prior treatments (p=0.049), TTP after autoSCT (p=0.032), PS (p<0.001), and serum albumin (p=0.016). On the other hand, aGvHD was not associated with EFS (p=0.545) and OS (p=0.476). Multivariate analysis demonstrated that stage IV (hazard ratio (HR) 2.85 (95% CI, 1.13–7.22); p=0.027) and ECOG PS 2 (HR 3.94 (95% CI, 2.08–7.47); p<0.001) were significant factors for EFS and that stage IV (HR 3.28 (95% CI, 1.19–9.04); p=0.022), ECOG PS 2 (HR 5.26 (95% CI, 2.22–12.48); p<0.001), and serum albumin above 3.0 g/dL (HR 0.15 (95% CI, 0.03–0.63); p=0.010) were significant factors for OS. TRM was associated with PS (p=0.010) and serum albumin (p=0.040) by univariate analysis. Multivariate analysis showed that ECOG PS 2 was the only significant factor for TRM (relative risk (RR) 11.77 (95% CI, 1.43–97.01); p=0.022). ECOG PS 2 was also a significant factor for documented sepsis (RR 7.14 (95% CI, 1.08–47.42); p=0.042). DLI was performed in 8 patients who failed alloSCT. After median 1.5 (range, 1–6) cycles of DLI, 2 patients achieved CR. Grade III or IV aGvHD developed in these patients. By contrast, among 6 patients who failed to achieve CR, aGvHD developed in 2 patients. In conclusion, alloSCT is a viable option for patients with NHL who failed autoSCT despite high TRM. Stage and PS were significant factors for EFS and OS. Serum albumin was a significant factor for OS. In patients with ECOG PS 2, alloSCT should be avoided and novel treatment approaches should be offered due to high risk of TRM. DLI after failure of alloSCT showed promising results, which supports the presence of graft-versus-lymphoma effect.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal