Abstract
Abstract 3783
Dengue fever is the most prevalent mosquito-borne viral disease, and its clinical signs and symptoms can vary widely. Since hemorrhagic manifestations are common, hematologists are often included in the care of these patients, and face a difficult challenge trying to discriminate dengue fever from other more common viral infections. Laboratory tests used in this context are less than optimal. The expected findings of leukopenia and thrombocytopenia are absent in many cases, thus delaying the suspicion for dengue and the ordering of confirmatory serological tests.
Leukocyte morphology changes in numerous medical conditions, including infections. The VCS technology available in the LH and DxH hematology analyzers is capable of automatically quantifying leukocyte morphologic characteristics: cell volume by voltage impedance (V); cytoplasmic and nuclear density by radio frequency conductivity (C); and cytoplasmic granularity and nuclear complexity by laser light scatter (S). The mean and standard deviation of each parameter is calculated. This data is collected for neutrophils, lymphocytes, monocytes and eosinophils separately.
Previous studies have demonstrated the significant value of these VCS parameters in improving the laboratory diagnosis of malaria and septicemia, both in adults and neonates. The objective of this study was to compare the performance of the VCS parameters with that of traditional hematological tests used in the diagnosis of dengue fever.
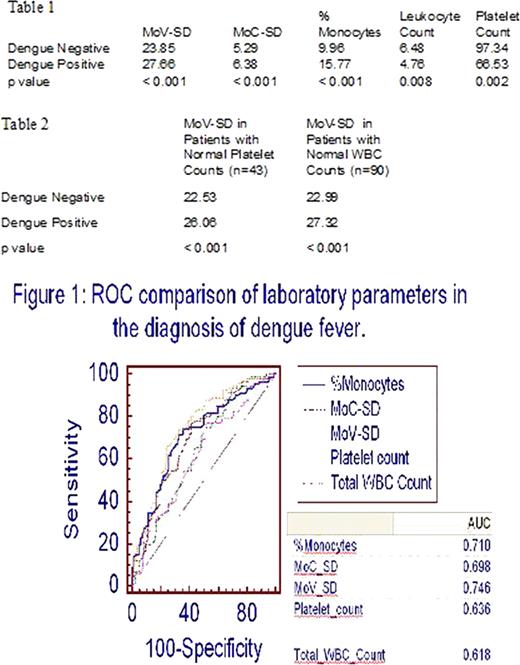
We included in this study 174 patients who were clinically suspected to have dengue fever, as indicated by the clinicians ordering serological testing. Of these, 92 patients were positive and 82 negative by serology. Using the Mann-Whitney U test, we compared the mean VCS values, as well as total leukocyte counts, leukocyte differential counts and platelet counts, between both groups. For those tests that showed a statistically significant difference between dengue positive and dengue negative patients, their diagnostic performance was compared by ROC curve. Finally, we separated patients with normal platelet and WBC counts, likely to be misdiagnosed based on these traditional laboratory tests, and evaluated the diagnostic performance of the VCS parameters in this subgroup.
Tests that showed a statistically significant difference (p<0.05) between dengue positive and dengue negative groups are listed in Table 1. There was marked anisocytosis of the monocytes in dengue positive patients, as demonstrated by the increased Monocyte Volume Standard Deviation (MoV-SD). ROC curves comparing the diagnostic performance of these tests are shown in Figure 1. The MoV-SD showed the best performance with an AUC of 0.74. Additionally, the MoV-SD was increased even in patients with unremarkable platelet and WBC counts (Table 2).
The MoV-SD was significantly increased in dengue positive patients. We speculate that the strong immune stimulation caused by the virus leads to this monocyte anisocytosis. These findings are analogous to those seen in bacterial sepsis, which causes neutrophil anisocytosis.
Since dengue fever is much less common than other viral diseases with similar symptoms, clinicians often rely on features such as thrombocytopenia and leukopenia as indicators of dengue. If these traditional findings are absent, serological testing and the correct diagnosis may be significantly delayed.
In this study, we have also demonstrated that the MoV-SD is increased even in those dengue infected patients with unremarkable hematological profiles, for whom the correct diagnosis could easily be overlooked. Since the MoV-SD is obtained automatically as part of any CBC with differential performed using VCS technology, it can greatly improve the detection of dengue fever in a timely and cost effective manner.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal