Abstract
Abstract 393
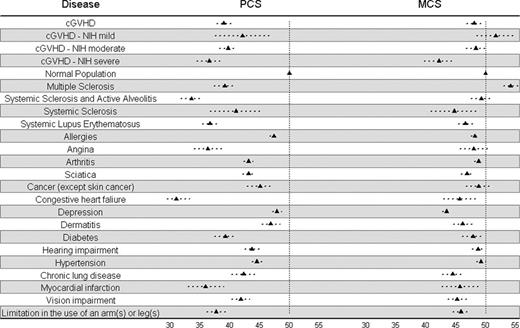
Chronic graft-versus-host disease (cGVHD) can negatively impact quality of life (QOL) following allogeneic hematopoietic cell transplantation (HCT). Whether the new NIH cGVHD global severity grading correlates with patient reported QOL is not known. In a prospectively assembled multi-center observational cohort study of adult HCT recipients with cGVHD, we examined the relationship between cGVHD severity according to NIH criteria and patient-reported QOL. Major objectives of this analysis were: (1) Describe the relationship between cGVHD severity and patient reported QOL; (2) compare QOL in HCT recipients with cGVHD to US population normative data; (3) compare QOL in HCT recipients with cGVHD to patients with other chronic health conditions; and (4) investigate the ability of SF-36 and FACT-BMT QOL instruments to discriminate cGVHD severity. This analysis included 298 patients with cGVHD who were enrolled at a median of 12.3 months from HCT. Overall, 54% patients were diagnosed < 3 months before enrollment. 56% had classic and 44% had overlap cGVHD. Organs most commonly involved included skin (63%), mouth (61%), eye (50%), and liver (50%). 31 (10%) had mild, 175 (59%) had moderate and 92 (31%) had severe cGVHD. Univariable modeling confirmed the relationship between cGVHD severity and QOL outcomes (SF-36 and FACT-BMT composite scores and subscales). Among other considered disease-, transplantation-, and socio-demographic variables, only age was significantly correlated with QOL (physical functioning and the physical component score (PCS) of the SF-36 instrument). Multivariable linear regression analysis adjusting for age at enrollment showed QOL measures, especially involving physical functioning, to differ according to cGVHD severity. For example, controlling for age, the average physical component score (PCS) of the SF-36 was 5.6 points higher for mild cGVHD compared to severe cGVHD (p < 0.01) and 3.2 points higher for moderate cGVHD compared to severe cGVHD (p = 0.02). In comparison to age- and gender-matched US population normative data for SF-36, mean scores for cGVHD cohort members were significantly lower for physical functioning, role-physical, bodily pain, general health, vitality, social functioning, and PCS. There were no significant differences observed in the domains of role-emotional, mental health, or MCS. We also compared the mean SF-36 scores (PCS and MCS) of cGVHD patients with those reported for other chronic health conditions: Patients with moderate and severe cGVHD had PCS scores comparable to scores reported for systemic sclerosis, systemic lupus erythematosis, and multiple sclerosis, and greater impairment compared to common conditions such as diabetes, hypertension, and chronic lung disease (see figure). MCS scores of those with severe cGVHD rivaled MCS scores reported with clinical depression, while mild and moderate cGVHD MCS scores were comparable to that of the general population. Discriminative accuracy of the QOL instruments (SF-36 and FACT-BMT) was assessed utilizing an extension of the concordance index to an ordinal gold standard (cGVHD severity). The concordance index was modest (∼0.60) for all QOL scales examined, with no significant differences between the QOL instruments' discriminative ability. We conclude that, while physical components of self-reported quality of life are lower on average for patients with more severe cGVHD, the extent of impairment and symptom burden represented by cGVHD severity are not solely captured by differences in quality of life. Future analyses will evaluate sensitivity to change and may help identify the better instrument to use in this population. In summary, NIH consensus criteria global cGVHD severity is independently associated with patient reported QOL, with worsening QOL for increasing severity of cGVHD. Patients with moderate to severe cGVHD have poor QOL, comparable to patients with other with immune mediated disorders, and much worse than general population norms. We hypothesize that better prevention and control of cGVHD has the potential to not only decrease morbidity and mortality but also to significantly improve QOL.
Comparison of SF-36 PCS and MCS mean scores (with 95% confidence interval) from chronic GVHD cohort members according to NIH severity and chronic health conditions
Comparison of SF-36 PCS and MCS mean scores (with 95% confidence interval) from chronic GVHD cohort members according to NIH severity and chronic health conditions
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal