Abstract
Abstract 4126
The immunohistochemical (IHC) profile as described by Hans and colleagues has emerged as a potential prognostic and predictive factor in patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) treated with chemotherapy. However, its role has not been completely elucidated. The main objective of this patient-level meta-analysis was to evaluate the IHC profile as a prognostic and predictive indicator in newly diagnosed DLBCL patients treated with R-CHOP. Secondary objectives were to identify potential novel prognostic factors in these patients.
Patient-level clinical data was requested from 13 research groups that published studies on the role of the IHC profile in prognosis for DLBCL patients treated exclusively with R-CHOP. Six groups (46%) submitted their data, accounting for a total of 701 patients. The requested clinical data included age, sex, performance status, LDH levels, number of extranodal sites, clinical stage, expression of CD10, BCL-6 and MUM1, IHC profile, type of response, outcome and overall survival (OS). Logistical regression analyses were used to identify independent variables associated with overall and complete response rates. Univariate survival curves were estimated using the Kaplan-Meier method and compared using the log-rank test. Multivariate analysis was performed using the Cox proportional-hazard regression test. P-values of <0.05 were considered statistically significant.
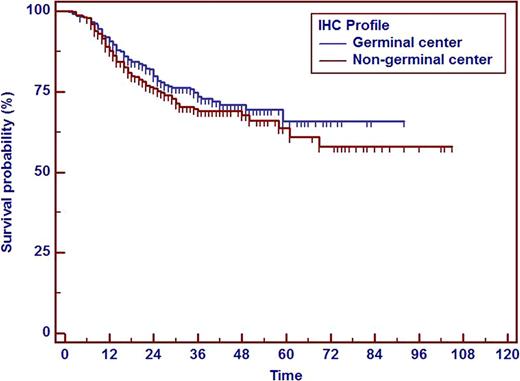
The median age was 63 years (range 16–90 years), 54% were men, 59% were 60 years or older, 24% had an ECOG ≥2, 55% had elevated LDH levels, 15% had ≥2 extranodal sites involved, 52% had stage III/IV and 48% had a non-germinal center (NGC) IHC profile. The overall response rate was 92% with complete responses seen in 78% and partial responses in 14%. The median follow-up was 34 months. In the logistical regression analysis, age ≥70, high LDH, ECOG ≥2, stage III/IV and a NGC profile were associated with improved overall response, and MUM1 expression, ECOG ≥2 and stage III/IV were associated with improved complete response. In the survival analysis, the estimated 5-year OS was 66% and the median OS was not reached. Age ≥60 years, elevated LDH levels and NGC IHC profile (Figure) were not associated with worse OS. In the multivariate analysis, age ≥70 years, male sex, ECOG ≥2 and clinical stage III/IV were independent prognostic factors for OS. A prognostic score was formulated using these 4 prognostic factors and then compared against the IPI and R-IPI scores. This novel score and the IPI score were the only independent factors for OS with HR 1.4 (95% CI 1.19–1.64) and 1.38 (95% CI 1.15–1.67) with p<0.0001 and p=0.0006, respectively.
The IHC profile is not a prognostic indicator for OS, and it is predictive of overall response but not complete response in newly diagnosed patients with DLBCL treated with R-CHOP. Age ≥70, male sex, ECOG ≥2 and stage III/IV were independent prognostic factors for OS. A score consisting of these 4 factors showed a significant prognostic value in DLBCL patients treated with R-CHOP.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal