Abstract
Abstract 4426
We present a case with disseminated intravascular coagulation (DIC) successfully treated with low dose Fondaparinux.
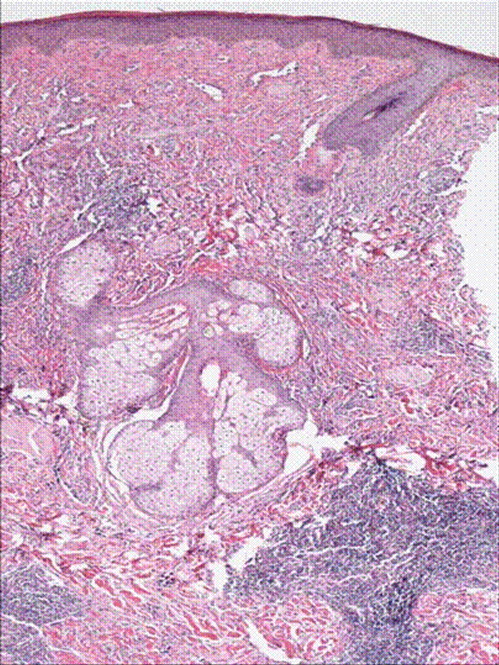
A 50 year old male with past medical history of diabetes, hypertension was diagnosed with angiosarcoma localized to the face (Figure 1 & Figure 2). The patient had baseline mild coagulopathy before start of chemotherapy most likely from the angiosarcoma. He received the first cycle of paclitaxel and bevacizumab but required hospitalization four days later for chest pain and acute coronary syndrome was ruled out. He then developed febrile neutropenia with an ANC of 0.0 and progressive pancytopenia. On day 9 of chemotherapy, the patient had a platelet count of 12 K/μ L with hemoglobin of 6.1gm/dl, hematocrit of 18% and WBC count of 3 k/μ l. The peripheral smear revealed many schistocytes, in addition elevated LDH 1112U/L, with an indirect bilirubin of 2.62 mg/dl, total bilirubin of 3.80mg/dl, and a haptoglobin of less than 10. His coagulopathy progressed with a PT of 17.3, PTT 65.3, fibrinogen degradation products (FDP) which were less than 10 on day 6 post chemo, were more than 40 on day 8 and his D-Dimers were 13.5 mg/l(Figure 5). ADAMTS13 level was drawn and though his creatinine and mental status remained normal, plasmapharesis was initiated with the presumptive diagnosis of thrombotic thrombocytopenic purpura (TTP).
The patient developed a mild to moderate pericardial effusion without evidence of tamponade and was monitored in the critical care unit. Echocardiogram also revealed an elevated pulmonary artery pressure of 60 mmHg. He was treated with broad spectrum antibiotics, daily plasmapharesis and blood products as needed. Initial platelet count responded to plasmapharesis going up to 50 by day 22. His ADAMTS 13 level on day 9 and 12 were 392ng/ml (ref > 590ng/ml) and 297ng/ml respectively.
After 38 days of plasmapharesis platelet count stayed in the range of 10–20 and pericardial effusion was stable. We decided to consider the alternative diagnosis of acute on chronic DIC. Patient was started on Fondaparinux at a dose of 2.5mg initially for 3 days and then increased to 5mg SQ. On day 7 of Fondaparinux the platelet count was 137 from 20, PTT 35.5 (baseline 40), D-Dimers 0.74 and FDP were less than 10. (Figure 3,Figure 4 and Figure 5)
Microangiopathic hemolytic anemia (MAHA) can be is seen in tumors of vascular origin and could be caused due to TTP or DIC. These tumors can present as Kasabach Merritt phenomenon which is characterized by severe thrombocytopenia and or coagulopathy due to platelet trapping in the vascular tumor. This phenomenon usually responds to chemotherapy (1). In our case initially anticoagulation I was a difficult choice because of acute pericardial effusion. The rationale for using Fondaparinux were two; one a theoretical benefit of anticoagulation in DIC(2), second patient also was developing pulmonary hypertension observed on serial ECHO's done for pericardial effusion indicating an ongoing chronic thrombo-embolic process. We decided to avoid heparin because it can itself cause thrombocytopenia and may confound with our clinical condition. Patient responded well and has been stable on low dose Fondaparinux.
1.Kasabach-Merritt syndrome associated with angiosarcoma of the scalp sucessfully treated with chemoradiotherapy. mafuku S, Hosokawa C, Moroi Y, Furue M. cta Derm enereol. 2008;88(2):193-4.
2.Angiosarcoma variant of Kasabach-Merritt syndrome. Alliot C, Tribout B, Barrios M, Gontier MF. Eur J gastroentrol Hepatol. 2001 Jun;13(6):731-4
H& E stain of punch biopsy of the lesion from the cheek showing infilterating vascular tumor.
H& E stain of punch biopsy of the lesion from the cheek showing infilterating vascular tumor.
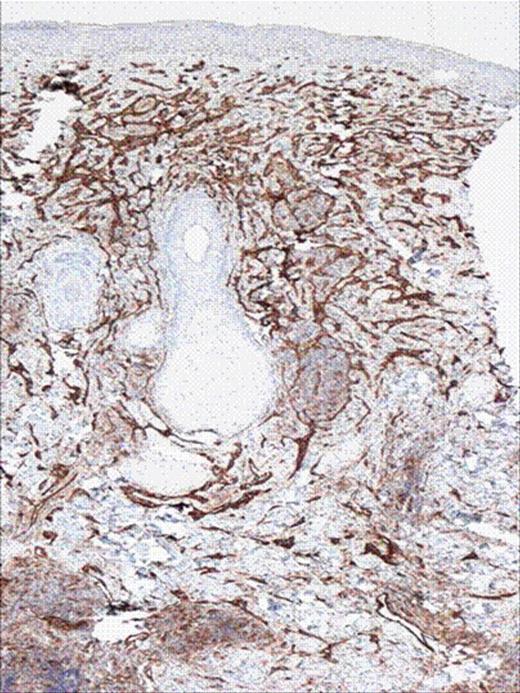
CD 31 stains of the skin biopsy showing vascular tumor.
Off Label Use: Fondaprinux is a direct thrombin inhibitor used for anticoagulation for venous thromboembolism. It is only technical off label because it is not mentioned in the label of the drug.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal