Abstract
Abstract 4610
Infections are a major cause of morbidity and mortality in patients with chronic lymphocytic leukemia (CLL). Up to 50% of patients with CLL will develop infectious complications during the course of their disease, and 30–50% of all deaths from CLL are attributed to infections and infectious complications. The risk of infection in CLL is related to immune deficiencies associated with the primary disease process, as well as immunosuppression secondary to treatment.
Available research on infectious complications of CLL has focused on patients in clinical trials receiving chemotherapy. Little is known about the natural history of infection in community dwelling patients with newly diagnosed CLL.
To explore the natural history of infection in a local, community dwelling cohort of patients diagnosed with CLL, we used the Mayo Clinic CLL database to identify all patients with newly diagnosed CLL seen in the Mayo Clinic Division of Hematology after January 1, 1999 and who resided within 50 mi of Mayo Clinic (Rochester, MN). All patient hospitalizations were reviewed to document infection including cross-referencing with the electronic Mayo Clinic infection database which includes all culture and serology results obtained from hospitalized Mayo Clinic patients. Patients who had positive blood, sputum, cerebrospinal fluid, pleural fluid, or paracentesis fluid culture results were identified. Patients whose cultures were negative were considered to have culture negative infection. Serologies and viral assays (e.g. CMV viral load) were also reviewed to identify infections.
In May 2010, there were 2022 patients in the Mayo Clinic CLL Database with the diagnosis of CLL/SLL made between Jan 1999 – Dec 2009. Of these, 336 (17%) patients resided within a 50 mi radius of Mayo Clinic and were considered non-referred, community-based CLL patients.
Median age at diagnosis for these 336 patients was 69 yrs (range 27–97) and most had early stage CLL (57% stage 0; 34% stage I-II). With respect to prognostic markers, 206 (70%) patients were CD38 negative, 125 (64%) ZAP-70 negative, 85 (53%) IgVH mutated, and 101 (63%) had either no abnormality or 13q14- as a sole abnormality on FISH analysis. Consistent with being a community dwelling cohort, ~90% (152/165) of patients had co-morbid health problems and ~50% (86/165) had a major comorbidity (e.g. coronary artery disease, cerebral vascular disease, CHF, diabetes, COPD, other malignancy). Although ~17% (43/249) of patients had gamma-globulin levels below the reference range at diagnosis, only 2% (6/249) had an IgG level <500 mg/dL.
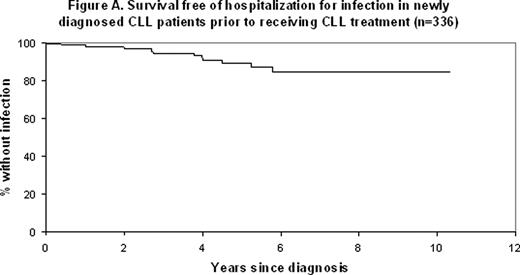
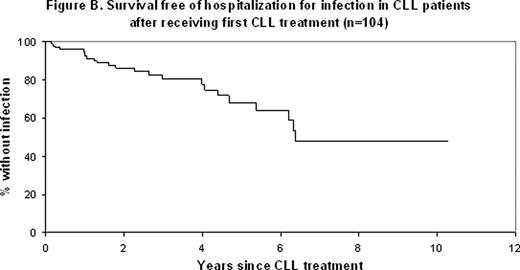
Median follow-up for all patients was 49 months (range 0–121) and 104 (31%) patients progressed to require treatment for CLL. Although 222 (66%) patients required hospitalization during follow-up, only 38 (11.3%) were hospitalized with infection. Collectively, these 38 patients were hospitalized for infection 139 times (median 2 hospitalizations for infection per patient). Among these 38 patients, 13 had no organism identified on cultures (culture negative infection) while the remaining 25 (66%) had an organism identified during at least hospitalization for infection. Of the 38 patients hospitalized with infection, 18/38 (47%) had a gram positive organism (8 strep pneumonia, 11 staphylococcus Aureus, 2 nocardia), 11/38 (29%) had a gram negative organism (3 E.Coli, 4 Pseudomonas, 4 Hemophilus influenzae), 5/38 (13%) a mycobacterial infection (4 MAC, 1 M. gordonae), 15/38 (40%) a cytomegalovirus infection, 19/38 (50%), cryptococcus and/or cryptosporidium (18 cryptococcus AG, 4 cryptosporidium), and 12/38 (32%) a filamentous fungi infections (12 aspergillous). In aggregate, hospitalization for an opportunistic infection (e.g. cytomegalovirus, cryptococcus, filamentous fungi, myocobacteria, pneumocystis) occurred in 26/336 (8%) CLL patients during follow-up.
Being male (OR 2.7; p=0.02), ZAP-70+ (OR 3.9; p=0.004), IGHV unmutated (OR 5.5; p=0.002), and receiving treatment (OR 4.7, p<0.001; Figure) were associated with increased risk of hospitalization for infection.
Approximately 8% of newly diagnosed, community dwelling CLL patients will require hospitalization for opportunistic infection at some point during the course of their disease. Gender, disease factors (e.g. ZAP-70, IGHV status), and treatment characteristics are associated with infection risk.
Zent:Genzyme: Research Funding; Genentech: Research Funding; Novartis: Research Funding; G.S.K.: Research Funding. Shanafelt:Celgene: Research Funding; Hospira: Research Funding; Genentech: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal