Abstract
Abstract 4750
In Chronic myeloid leukemia (CML), that have an insidious onset, some patients are diagnosed in the asymptomatic phase by high white blood cells count (WBC) with immature granulocytes, when submitted to routine periodic exams (preventive medicine). In developing countries, preventive medicine is almost non-existent and most patients are diagnosed when look for medical attention because of signs and symptoms such as fatigue, weight loss, anemia, night sweats and splenomegaly. In modern treatment of CML, the kinase inhibitors are employed and the most common of these is imatinib mesylate, which specifically inhibits the BCR-ABL chimeric protein very efficiently. Despite the excellent results obtained by Druker et al. (N Engl Med J 355:2408-2417, 2006), with 98% progression free survival for five years, studies conducted in developing countries like India, China and Brazil showed high frequency of suboptimal response (Rajappa et al. Leuk Lymphoma 49:554-558, 2008; Zhao et al. Int J Hematol 89:445-451, 2009; Scerni et al. Clinics 64:731-734, 2009), attributed by authors to delayed treatment. Several factors such as mutation and no compliance may also explain this fact, however, the diagnosis of the disease in late chronic phase combined with the delayed treatment may be an important factor because only a small proportion of patients (less than 20%) is diagnosed randomly in asymptomatic chronic phase or in periodic examinations. Thus, it appears clear that a good response to treatment depends largely on the early diagnosis and immediate treatment, factors that were decisive for the indicators of survival from controlled studies in Europe and USA, which have been better than the ones in developing countries.
To evaluate the influence of late diagnosis and delayed treatment on long term sustained optimal response to imatinib therapy.
We analyzed, in an observational study, 71 patients with CP CML, with a median age of 39 years old, treated with imatinib (400mg) at Ophir Loyola Hospital (Belém-PA-Brazil). Molecular response was evaluated using quantitative real time PCR every 3 months. We consider the response to imatinib therapy as optimal or suboptimal according to criteria of the European LeukemiaNet (Baccarani et al. Blood 108:1809-1820, 2006) and survival time was considered from the start of treatment until the last visit to the doctor. To estimate the time course of the disease at diagnosis, we have used the method of Kamada and Uchino (Blood 51:843-850, 1978) in which the time between the normal maximum WBC count, (10 × 109/L) and onset of symptoms (15.5 months) occurs at about 70 ×109 WBC/L, which can be calculated by the formula logY=0.053X+10.023 (R2=0.79), where Y=WBC and X=months.
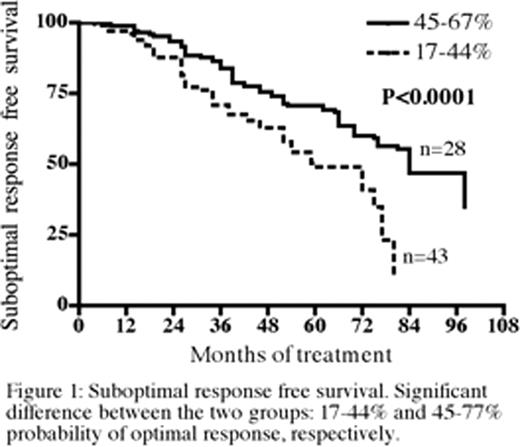
We have analyzed the interdependence of response to imatinib therapy to the variables ‘time course of the disease at diagnosis, mean=20.2 months’ and ‘time between diagnosis and initiation of treatment, mean=18.6 months’ by multiple logistic regression, which revealed high significance of these variables in the response to imatinib therapy (p=0.007). From this analysis, the following formula Logit Pi=-1.0804+[0.0458(X1)]+[0.01659(X2)] was generated, which allowed the calculation of the probability of achieving the optimal response. We have identified two groups, one which had probability to achieve optimal response between 17 and 44% and the other between 45 and 67%, which after the Kaplan Meier analysis and Log Rank Test, had a median survival of 60 and 84 months, respectively (p<0.0001) (Figure 1).
The results show that this method may be useful to estimate the long term sustained response based on the WBC count at diagnosis, and thus we could classify patients with a probability greater than 44% with good chance of sustained response after 5 years of treatment. Late diagnosis combined with delayed treatment is a factor that undermines the good response to imatinib therapy and this can be an important issue for the treatment of CML in developing countries. Thus, early detection of CML in the group with most affected age could be a good way to circumvent this problem, since the long-term suboptimal response will certainly lead the patient to treatment failure.
Lemos:Novartis, Brazil: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal