Abstract
Abstract 4876
Pneumocystis jirovecii is an opportunistic pathogen responsible for severe pneumonia in immunocompromised patients. Management of this pneumonia remains a major challenge for all physicians caring for immunosuppressed patients. The prognosis of Pneumocystis jirovecii pneumonia (PCP) with acute respiratory failure is traditionally known to be poor.
We report a case of PCP in a child with recently diagnosed childhood Precursor B cell Acute Lymphoblastic Leukemia (ALL). Course was complicated with acute respiratory failure showing hypoxemia, respiratory failure requiring intubation and reduced compliance resembling ARDS.
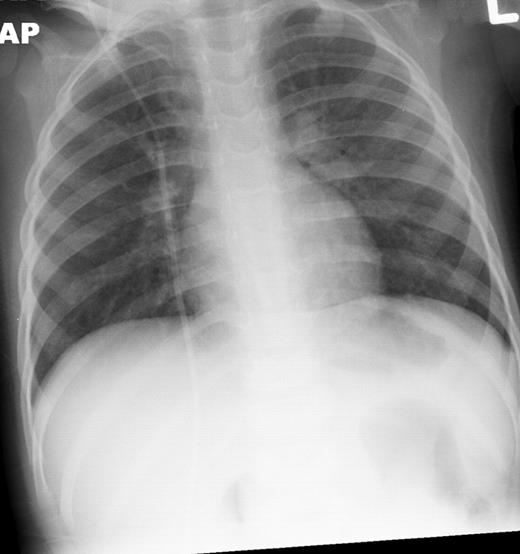
Our Patient, 8 weeks into chemotherapy for newly diagnosed ALL, presented with high grade fevers and poor activity. Patient was admitted 3 weeks prior for Bacillus cereus bacteremia. Additionally the patient had been on broad spectrum antibiotics on 2 occasions for febrile neutropenia episodes within the past 2 weeks. Patient had minimal respiratory symptoms at this presentation and recovered from pancytopenia at the time of this presentation. CT scans and chest x-ray (Figures 1 and 2) showed diffuse marked ground glass opacities with dependent consolidation in the lungs. On day 3 of admission, bronchoalveolar lavage (BAL) was preformed and empiric trimethoprim-sulfamethoxazole was initiated in addition to broad spectrum antibacterial, antifungal and antiviral medications.
Within 24 hours, patient rapidly deteriorated with significant respiratory distress and hypoxemia requiring intubation. Clinical and radiologic findings were suggestive of ARDS. Patient required significant ventilatory support, fluid restriction, diuretics, and steroids. PCR testing of BAL fluid was reported as positive for Pneumocystis jirovecii. By hospital day 6 the patient was still requiring a fair amount of respiratory support. Corticosteroids had been added but concern amongst some members of the team surrounded possible lack of efficacy of trimethoprim-sulfamethoxazole. Review of published case reports suggested that addition of caspofungin provided salvage therapy in cases where trimethoprim-sulfamethoxazole was believed to be suboptimal. Caspofungin was added to this patient's treatment. However, liver trans-aminases experienced a 2–3 fold increase within 72 hours after initiating caspofungin. Caspofungin was withdrawn but the patient's condition gradually improved and was extubated 7 days later. Also of note, there have been wide spread regional and national shortages of intravenous trimethoprim-sulfamethoxazole preparations. We were forced to convert to oral therapy several days after extubation. The patient continued to improve and had no signs of complications or increased morbidity from this conversion; however, this was a continued concern during his treatment.
Ground Glass Opacities on CT Chest
Chest x-ray infiltrates
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal