Abstract
Abstract 872
All-trans retinoic acid (ATRA) with contemporary therapeutic strategies for the treatment of patients with newly diagnosed acute promyelocytic leukemia (APL) have dramatically improved outcome. Currently, the major cause for treatment failure is death during induction mostly due to hemorrhage, infection and differentiation syndrome. Since there is virtually no primary resistance to induction and the relapse rate once in complete remission (CR) is very low, reducing the early death rate would be critical to further improve the cure rate. The true rate of early death in the United States (US) is not yet clear. Cooperative group multicenter studies report early death rates of 5–10% within 1 month of starting therapy which is likely an underestimation, in part, due to failure to account for those who die prior to registration on study or possibly other selection biases for enrollment.
We performed an epidemiologic study of the true rate of early death and overall survival (OS) using US population-based datasets of all newly diagnosed patients with APL. The datasets from SEER Program 13 (includes 5 states: Connecticut, Hawaii, Iowa, New Mexico and Utah; 8 metropolitan areas including Detroit, Atlanta, San Francisco-Oakland, Seattle-Puget Sound, Los Angeles, San Jose-Monterey, Alaska Native Registry and rural Georgia) and the New York (NY) State Cancer Registry were used to identify patients with APL registered in the US and NY state from January 1, 1992 to December 31, 2007. Patterns of APL incidence, early death rate, long-term OS over time, and differences in OS by region (urban vs. rural) were analyzed in pre-set time periods of 1992–1996, 1997–2001, and 2002–2007.
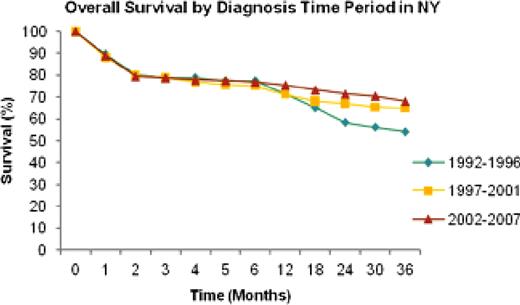
A total of 1,400 and 721 patients with APL were identified in the SEER program and the NY registry, respectively. The number of registered APL patients was similar between men and women in both datasets, and has steadily increased from 1992–1996 (295 cases in SEER and 143 in NY) to 2002–2007 (681 cases in SEER and 371 in NY). Early death rate, defined as death reported within the first month of diagnosis, was 22.7% in the years 1992–1996, 15.6% in 1997–2001, and 18.1% in 2002–2007 in the SEER program, and 10.9%, 11.9% and 11.2% in the NY registry. No significant differences in the early death rate were observed between urban and rural areas in either datasets. OS at 1 year improved from 59.8% in 1992–1996 to 69.6% in 1997–2001; at 2 years from 53.7% to 65.3%; and at 3 years from 50.2% to 63.7% in the datasets from the SEER program. There were no significant changes in OS from 1997–2001 to 2002–2007, and similar trends in OS were observed in the NY datasets (Figure). Interestingly, when the survival data were analyzed by the urban/rural regions in the SEER program, the greatest improvement was observed in patients treated in the urban counties with absolute increases in 2- and 3-year OS of 15.3% (from 53.1 in 1992–1996 to 68.4% in 2002–2007) and 17.6% (from 49.8 to 67.4%), respectively. In contrast, in patients treated in rural counties, increases in 0.4% (from 62.5 in 1992–1996 to 62.9% in 2002–2007) and 7.3% (from 55.6 to 62.9%) were observed in 2- and 3-year OS, respectively. However, the latter statement should be interpreted with caution since the rural OS estimates are imprecise due to small numbers.
The large number of newly diagnosed APL patients and the long follow-up reported here confirm improvement in OS over time in a US population-based study. Disappointingly, the early death rate has changed only modestly since 1992 (22.7% in 1992–1996, and 18.1% in 2002–2007), and appears significantly higher than what is reported in contemporary clinical trials. Furthermore, the long-term OS, though improved over time, appears lower than that reported in clinical trials. In fact, more than 25% of patients are not cured of their disease. OS in patients treated in rural areas appears worse, possibly related, in part, to less access to specialized centers, although the analysis is limited due to small numbers. Strategies to reduce the early death rate in APL and improve OS should include very early introduction of ATRA, arsenic trioxide or both and aggressive blood product support at the very first suspicion of the diagnosis well before genetic confirmation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal