Abstract
Abstract 902
HCT is a curative option for patients with hematologic malignancies. However, the procedure carries a high risk of death in the immediate post-HCT period in part due to disease recurrence (relapse-related mortality [RM]), but also due to treatment-related mortality (TRM) resulting from the following: i) toxicity due to high intensity treatment; ii) graft vs. host disease (GvHD) and its management; and iii) infections. Previous studies utilizing data from HCTs performed in 1980s and 1990s indicate that the 1-yr cumulative incidence of TRM exceeds 20% for related donor and 30% for unrelated donor HCTs. However, gaps in knowledge remain related to the cause-specific cumulative incidence of TRM and RM after autologous and allogeneic HCT performed in the more recent eras.
Between 2005 and 2008, a total of 1,673 consecutive patients received HCT at City of Hope at a median age of 50 years for AML (n=433), NHL (n=428), MM (n=369), ALL (n=176), and HL (n=154); 913 patients received autologous HCT; 382 allogeneic related donor; and 378 unrelated donor HCT. Reduced intensity conditioning was used for 268 patients. Early mortality was defined as death in the first year after HCT due to disease (RM) or treatment (TRM). Information regarding vital status and cause of death were obtained from medical records, supplemented with Social Security Death Index. Overall survival (OS) and cumulative incidence of TRM and RM were calculated for 30 d, 6 mo and 1 yr after HCT for i) the entire cohort, and by ii) diagnosis and iii) type of HCT. Multivariable models identified predictors of TRM and RM.
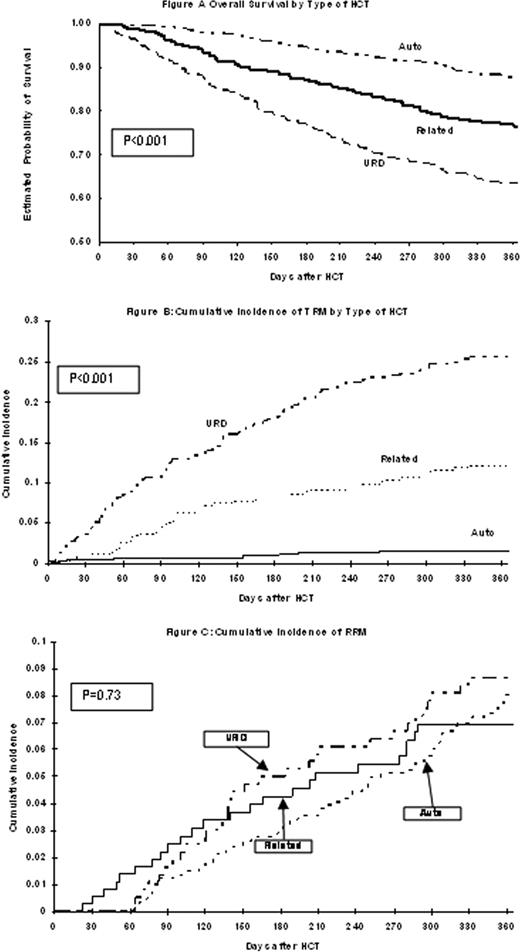
A total of 323 deaths (19.3% of the entire cohort) were observed within the first year after HCT; 55.5% attributed to TRM and 44.5% to RM. Among deaths due to TRM, 59% were attributed to infections, 12.9% to acute or chronic GvHD, and 9.5% to organ toxicity. Among autologous, related and unrelated donor HCT recipients, overall survival (OS) was 87.2%, 76.6% and 63.5% at 1 yr (p<0.001) (Figure 1A). Among autologous, related donor, and unrelated donor HCT recipients, 1-yr cumulative incidence of TRM was 1.6%, 12.1%, and 25.6% respectively (p<0.001) (Figure 1B), and cumulative incidence of RM was 8.2%, 6.9%, and 8.7% respectively (p=0.73) (Figure 1C). OS and cumulative incidence of TRM and RM by disease and type of HCT are summarized in Table . Predictors of increased RM included age at HCT 40–60 yr (HR: 1.6, p=0.04; referent group: <40 yr), and diagnosis of NHL (HR=2.0, p=0.008; referent group: AML); receipt of HCT in the later years was associated with decreased RM (2007: HR=0.5, p=0.02; 2008: HR=0.5, p=0.04; referent group: HCT in 2005). Of note, RM for NHL and AML did not differ by type of HCT (p=0.94). Predictors of TRM included allogeneic HCT (related: HR=4.3, p=0.0003; unrelated: HR=10.2, p<0.0001; referent group: autologous HCT). Among related and unrelated HCT recipients, use of reduced intensity conditioning did not have a significant impact on TRM (HR=1.2, p=0.6) or RM (HR=1.2, p=0.7).
For patients with NHL and AML, cumulative incidence of RM does not differ by HCT type. Unrelated donor HCT continues to be associated with the highest risk of TRM. Infection is the most frequent cause of TRM, accounting for 62% of deaths due to TRM in unrelated donor, 52% in related donor, and 46% in autologous HCT recipients – reinforcing the need for aggressive measures for prevention and treatment of infections in this immune compromised population.
| . | Overall survival . | Cum incidence: TRM . | Cum incidence RRM . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 30 d | 6 mo | 1 yr | 30 d | 6 mo | 1 yr | 30 d | 6 mo | 1 yr | |
| Entire cohort (n=1673) | 98.7% | 88.8% | 79.1% | 1.2% | 6.7% | 9.7% | 0.1% | 3.7% | 8% |
| Autologous HCT (n=913) | 99.6% | 94.8% | 87.2% | 0.5% | 1.1% | 1.6% | 0 | 2.9% | 8.2% |
| Allogeneic HCT (n=382) | 98.7% | 87% | 76.6% | 0.8% | 8.2% | 12.1% | 0.6% | 4.3% | 6.9% |
| URD HCT (n=378) | 96.6% | 77% | 63.5% | 3.6% | 17.9% | 25.6% | 0% | 5% | 8.7% |
| Autologous (AML: n=67) | 98.5% | 95.2% | 85.3% | 1.5% | 4.8% | 6.4% | 0% | 0% | 8.2% |
| Related donor (AML: n=175) | 98.9% | 85.3% | 72.4% | 0.6% | 10.1% | 14% | 0.6% | 4.4% | 8.3% |
| URD HCT (AML: 191) | 97.4% | 75% | 62.9% | 2.7% | 19.3% | 25.1% | 0 | 5% | 9.1% |
| Related donor (ALL: n=89) | 97.8% | 89.7% | 80.3% | 2.4% | 8.5% | 13.6% | 0% | 0% | 0% |
| URD HCT (ALL: n=87) | 93.3% | 72.8% | 57.8% | 6.7% | 21.5% | 33.1% | 0 | 5.7% | 9.2% |
| Autologous (NHL: n=313) | 100% | 91.2% | 82% | 0% | 0% | 0.4% | 0% | 6.6% | 13.7% |
| Related donor (NHL: n=63) | 98.4% | 81.6% | 68.9% | 0% | 8.5% | 14.2% | 0% | 10.5% | 14.3% |
| URD HCT (NHL: n=52) | 98.1% | 82.4% | 70.7% | 1.9% | 9.9% | 16.5% | 0% | 7.9% | 11.9% |
| Autologous (HL: n=147) | 99.3% | 94.2% | 87.2% | 0.7% | 2.2% | 2.2% | 0% | 2.2% | 7% |
| Autologous (MM: n=358) | 99.7% | 98.4% | 92.6% | 0.3% | 0.6% | 1.3% | 0% | 0.7% | 3.9% |
| . | Overall survival . | Cum incidence: TRM . | Cum incidence RRM . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 30 d | 6 mo | 1 yr | 30 d | 6 mo | 1 yr | 30 d | 6 mo | 1 yr | |
| Entire cohort (n=1673) | 98.7% | 88.8% | 79.1% | 1.2% | 6.7% | 9.7% | 0.1% | 3.7% | 8% |
| Autologous HCT (n=913) | 99.6% | 94.8% | 87.2% | 0.5% | 1.1% | 1.6% | 0 | 2.9% | 8.2% |
| Allogeneic HCT (n=382) | 98.7% | 87% | 76.6% | 0.8% | 8.2% | 12.1% | 0.6% | 4.3% | 6.9% |
| URD HCT (n=378) | 96.6% | 77% | 63.5% | 3.6% | 17.9% | 25.6% | 0% | 5% | 8.7% |
| Autologous (AML: n=67) | 98.5% | 95.2% | 85.3% | 1.5% | 4.8% | 6.4% | 0% | 0% | 8.2% |
| Related donor (AML: n=175) | 98.9% | 85.3% | 72.4% | 0.6% | 10.1% | 14% | 0.6% | 4.4% | 8.3% |
| URD HCT (AML: 191) | 97.4% | 75% | 62.9% | 2.7% | 19.3% | 25.1% | 0 | 5% | 9.1% |
| Related donor (ALL: n=89) | 97.8% | 89.7% | 80.3% | 2.4% | 8.5% | 13.6% | 0% | 0% | 0% |
| URD HCT (ALL: n=87) | 93.3% | 72.8% | 57.8% | 6.7% | 21.5% | 33.1% | 0 | 5.7% | 9.2% |
| Autologous (NHL: n=313) | 100% | 91.2% | 82% | 0% | 0% | 0.4% | 0% | 6.6% | 13.7% |
| Related donor (NHL: n=63) | 98.4% | 81.6% | 68.9% | 0% | 8.5% | 14.2% | 0% | 10.5% | 14.3% |
| URD HCT (NHL: n=52) | 98.1% | 82.4% | 70.7% | 1.9% | 9.9% | 16.5% | 0% | 7.9% | 11.9% |
| Autologous (HL: n=147) | 99.3% | 94.2% | 87.2% | 0.7% | 2.2% | 2.2% | 0% | 2.2% | 7% |
| Autologous (MM: n=358) | 99.7% | 98.4% | 92.6% | 0.3% | 0.6% | 1.3% | 0% | 0.7% | 3.9% |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal