To the editor:
Kantarjian and coworkers have recently stated that intensive chemotherapy does not benefit most older patients with acute myeloid leukemia (AML),1 in contrast to the Swedish published experience.2 Their view was based on 446 patients 70 years or older who were referred to their institution 1990-2008 and treated with cytarabine-based intensive chemotherapy. The Swedish Acute Leukemia Registry is now updated (diagnosis 1997-2006; 3318 patients, median age 71 years; 998 patients were 70-79 years of age). Furthermore, our registry now also contains 1057 AML patients diagnosed since 2007 (median age 71 years), and thus this latter cohort can serve as validation.
Our study is not only larger and more recent but, more importantly, the patient cohort was unselected and includes all AML patients, including those who are judged to be unfit for treatment and referrals. Still, 55% of all patients 70-79 years of age had intensive treatment (64% in ages 70-74, and 44% in ages 75-79 years). The Swedish AML Guidelines from 2006 prescribe cytarabine 1 g/m2 twice daily for 5 days, with daunorubicin 60 mg/m2 for 3 days, with dose reductions if urgently needed. Intermediate-dose cytarabine is feasible for remission induction also in older AML patients according to our previous experience.3 Half of those treated achieved complete remission.
We previously identified that the decision to treat is not based merely on clinical features, but also on the doctor's perception of age and attitude toward remission induction. Thus, in ages 70-79 years, 75% of patients with AML, except acute promyelocytic leukemia (APL), received intensive treatment in some parts of Sweden compared with 41% in others.2 Still, the complete remission (CR) and early death rates among the treated were similar if many or few were treated, whereas the long-term survival of all was clearly superior when more patients were treated.
It is easy to identify risk factors in these patients, however, they apply whether or not patients receive intensive treatment, and patients with poor risk factors have very poor outcome when given palliation only. In fact, all patient subsets have better survival with intensive treatment than without.
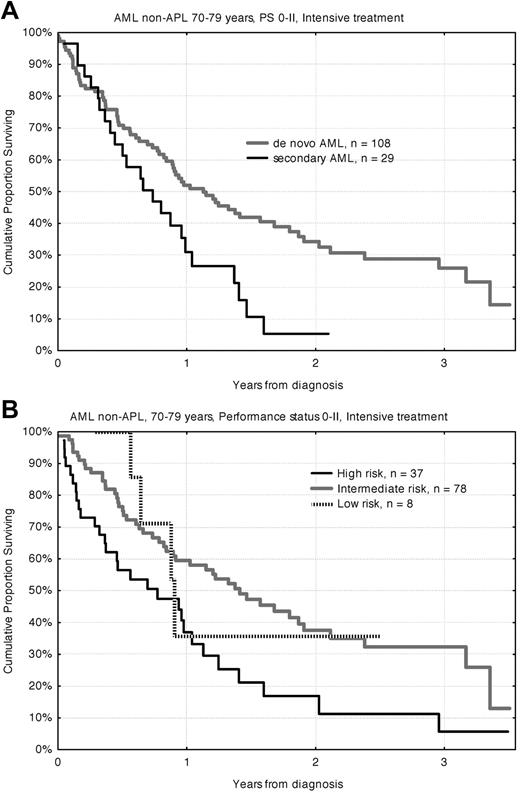
Among our recent AML non-APL patients 70-79 years, 40% had secondary disease (ie, previous hematologic disease and/or cytotoxic treatment), half had comorbidity, and 20% had a WHO/ECOG performance status (PS) of III-IV. Genetic risk classification4 identified high risk (including normal karyotype with FLT3-ITD) in 30% of de novo and 40% in secondary AML. NPM1+/FLT3-ITD− normal karyotype was regarded as low-risk. In PS III-IV this aged population had 76% 8-week mortality with palliation alone, but 50% with intensive treatment, an improvement that might not justify treatment toxicity and prolonged hospitalization. However, for patients with PS 0-II the 8-week mortality with intensive treatment for AML with intermediate-risk genetics was 8%, and 22% with high risk, but with palliative treatment the 8-week mortality was 23% and 47%, respectively. The overall survival of patients 70-79 years with PS 0-II given intensive treatment is shown in Figure 1.
Overall survival for AML non-APL patients aged 70-79 years diagnosed in Sweden 2007-2010 with performance status 0-II and receiving intensive treatment. Survival according to (A) de novo versus secondary disease and (B) genetic risk.
Overall survival for AML non-APL patients aged 70-79 years diagnosed in Sweden 2007-2010 with performance status 0-II and receiving intensive treatment. Survival according to (A) de novo versus secondary disease and (B) genetic risk.
The outcome for older patients with AML is highly unsatisfactory, but, although the development of new therapies is a high priority, it is not acceptable to withdraw patients from established useful treatment only because of age when our data show clearly that most patients 70-79 years of age not only tolerate but also benefit from intensive treatment.
Authorship
Contribution: G.J. wrote the letter.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Dr Gunnar Juliusson, Department of Hematology, Skåne University Hospital, Lund University BMC B10, Lund, 22184 Sweden; e-mail: Gunnar.Juliusson@med.lu.se.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal