Chronic GVHD is the leading cause of late nonrelapse morbidity and mortality. It is thus crucial for patient management and counseling to identify patients with low or high chronic GVHD-associated nonrelapse mortality risk.
Chronic graft-versus-host disease (GVHD) is a frequent but highly polymorphic complication of allogeneic stem cell transplantation. Its clinical presentation varies from few lichenoid skin lesions to a highly aggressive disease with multiple organ involvement mimicking autoimmune diseases such as scleroderma. Since its first clinical description in 1980,1 clinicians have tried to characterize the disease severity to adapt treatments and predict outcomes. Several risk factors predicting survival in patients with chronic GVHD have been reported (reviewed in Lee et al2 ) but none of them really reached applicability in clinical practice. However, some presenting features have been repeatedly associated with poor outcomes. In particular, thrombocytopenia3 (< 100 × 109/L) first described by Sullivan in the late 1980s and progressive onset4 (ie, chronic GVHD developing without discontinuity from acute GVHD) have been associated with poor outcomes.
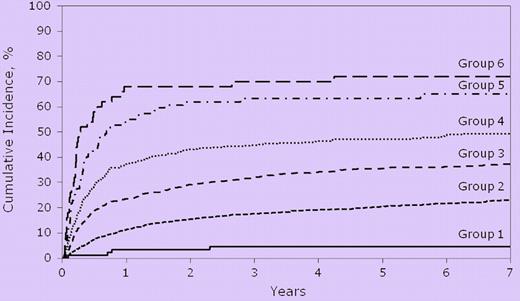
In this issue of Blood, Arora et al on behalf of the Center for International Blood and Marrow Transplant Registry (CIBMTR) revisited the risk factors associated with nonrelapse mortality (NRM) and survival in the setting of chronic GVHD.5 The authors have to be congratulated for the huge effort and high-level statistical analyses they performed. They evaluated patient, transplantation, and chronic GVHD characteristics at disease onset in a large cohort of nearly 5400 patients. They identified 10 variables associated with high NRM and lower probability of overall survival: older age, prior acute GVHD, shorter time from transplantation to chronic GVHD, mismatched related or mismatched unrelated donors, advanced or intermediate disease status at transplantation, GVHD prophylaxis other than cyclosporine plus methotrexate, gender mismatch, increased serum bilirubin, poor Karnofsky score, and platelet count < 100 × 109/L. Arora and colleagues then computed risk scores by assigning variables specific risk scores for each of the variables selected. Six risk groups were identified associated with different NRM risk and probability of survival (see figure).
Risk groups associated with different incidences of nonrelapse mortality according to Arora et al.5
Risk groups associated with different incidences of nonrelapse mortality according to Arora et al.5
Although risk groups 5 and 6 (see figure) could probably be collapsed into a single “very high” risk group, it represented (fortunately enough) a minority of patients (137 of 5343) but with a dismal prognosis (nearly 70% 5-year cumulative incidence of NRM). Otherwise, risk scores seemed to distribute risks fairly cleanly from around 5% to 40% 5-year cumulative incidence of NRM for risk groups 1 to 4. The risk factors included in the model are easily amenable to construct prospective validation studies. Thus, at a first glance this new risk score seems to be a promising useful clinical tool in chronic GVHD. There is 1 factor included in the model that deserves further comment: the time from transplantation to chronic GVHD.
In their analysis Arora et al report that a significant proportion of the patients (2301, 43%) had progressive GVHD. As patients with progressive onset of chronic GVHD had an earlier time to onset (median 3.6 months) as compared with de novo (median 5.2 months) and quiescent chronic GVHD (median 5.5 months), interaction between time to onset and type of onset was evaluated and the authors found it to be not significant. Arora and colleagues also recognize that persistent acute GVHD has many features similar to progressive-onset chronic GVHD, and thus repeated the analysis after excluding patients with early progressive onset chronic GVHD (progressive onset, < 130 days from transplantation). They report that the risk score remained similarly applicable for both overall survival and NRM in this population.
Why is it so important to look carefully at these patients with progressive chronic GVHD? It has been known for many years that although the disease usually manifests itself > 100 days after transplantation, earlier disease onset could occur. More importantly, clinical syndromes with features of typical acute GVHD are increasingly recognized beyond 100 days after hematopoietic stem cell transplantation, especially in recent years with the development of the reduced-intensity conditioning regimen. In addition, patients with acute GVHD may progress to developing chronic GVHD with symptoms of both acute GVHD and chronic GVHD. Recognizing these limitations, a group of experts under the auspices of the National Institutes of Health (NIH) met in 2004 for a consensus conference on chronic GVHD. All participants agreed that it was urgently necessary to get rid of the formal definition of chronic GVHD (any GVHD beyond day 100). The diagnosis and staging working group of the NIH Consensus Development Project on chronic GVHD thus proposed standard criteria for diagnosis, organ scoring, and global assessment of disease severity.6 Thus even Arora et al tried to take into account through a search for interactions between time to onset and type of onset or in excluding patients with early, progressive-onset chronic GVHD that it is highly likely a significant proportion of the patients included as progressive chronic GVHD would be considered to have persistent or recurrent acute GVHD according to the NIH criteria. For example, our group at Hospital Saint Louis analyzed patients who underwent transplantation for hematologic malignancies after reduced intensity conditioning regimen.7 The cumulative incidence of chronic GVHD at 36 months was 74% when using classic criteria compared with 54% with NIH consensus. In a Cox model, NRM was significantly higher in patients with late-onset, persistent, and recurrent acute GVHD. Thus not only using the NIH criteria cumulative incidence of chronic GVHD dropped by nearly 20% but NRM was mostly because of acute features of GVHD.
Nevertheless, Arora et al's study by the numbers of patients and quality of analyses remains highly valuable. The score, if validated using NIH definitions of chronic GVHD, will prove a practical tool to help identify high-risk patients for further therapy and enrollment in clinical trials.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal