In this issue of Blood, Lacy et al report that pomalidomide overcomes refractoriness to prior therapy with lenalidomide and bortezomib, thus representing a new and valuable treatment option for patients who have exhausted major novel agent–based strategies for the management of multiple myeloma.1
Over the past decade, increasing use of the immunomodulatory derivatives (IMiDs) thalidomide and lenalidomide and the first-in-class proteasome inhibitor bortezomib has dramatically changed the natural history of multiple myeloma (MM).2 Novel agents, initially approved for the treatment of relapsed or refractory (rel/refr) MM, are actually used up-front as part of induction therapy for both transplant- and nontransplant-eligible patients, and studies are under way to evaluate their role in additional therapeutic phases, such as consolidation and maintenance.3,4 However, almost all patients treated with these new classes of agents inevitably develop drug resistance over time, and ultimately relapse. Mechanisms leading to resistance are largely unknown. Overexpression and mutation of β5-proteasome activity, and activation of Wnt/β-catenin signaling5 have recently been proposed as possibly related to refractoriness to bortezomib and lenalidomide, respectively. Patients failing bortezomib and lenalidomide have a very dismal clinical outlook, and represent an unmet medical need.
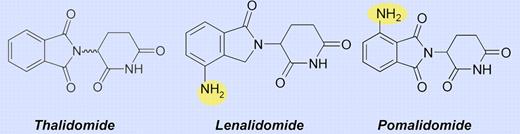
Pomalidomide (CC-4047) is a new IMiD (see figure) with increased activity in vitro compared with thalidomide and lenalidomide, which exerts anti-MM effects through multiple mechanisms, including induction of apoptosis via caspase-8, reduction of proliferation, inhibition of NF-κ B activation, reduction of stromal cell stimulatory cytokine secretion, and angiogenesis inhibition.
The safety and toxicity profile of pomalidomide as a single agent in patients with rel/refr MM was initially explored in two pilot phase 1 studies that established the maximum tolerated dose as 2 mg daily on days 1 through 28 of 28-day cycles and 5 mg on alternate days.6,7 In two subsequent studies enrolling patients with rel/refr MM after 1 to 4 prior lines of treatment, including refractoriness to lenalidomide, salvage therapy with pomalidomide at 2 mg/day was given continuously in 28-day cycles combined with low-dose dexamethasone.8,9 In one study, the overall rate of at least partial response (PR) was 63%, including 33% complete response or very good partial response (VGPR), and median progression-free survival (PFS) was 11.6 months.8 Among patients refractory to prior lenalidomide, PR or better was seen in the 32% to 40% range, suggesting a lack of cross-resistance between lenalidomide and pomalidomide.9
These promising results provided the basis of the study designed by Lacy et al to evaluate the efficacy of two different doses of pomalidomide in patients with dual refractoriness (defined as progression on therapy or within 2 months of stopping treatment) to lenalidomide and bortezomib.1 For this purpose, 70 patients who had received a median of 6 prior therapies (range, 2-11) were enrolled in two sequential phase 2 trials of pomalidomide given continuously at a daily dose of either 4 or 2 mg of 28-day cycles along with 40 mg of dexamethasone on days 1, 8, 15, and 22. The rates of at least minimal response in the 4-mg and 2-mg cohorts were 49% and 43%, respectively, including VGPR and PR rates of 28.5% and 26%, respectively. These values of PR or better appear slightly lower than those observed in previously reported series of lenalidomide-refractory patients,8,9 a finding that reflects the more heavily pretreated population of patients enrolled in the current trial and, importantly, their dual refractoriness to both lenalidomide and bortezomib. Consistent with this interpretation, similar rates of at least PR were seen in the phase 1 and 2 portions (the latter using daily pomalidomide at 4 mg on days 1-21 of 28-day cycles) of MM-002 study that included patients who had been previously treated with bortezomib and lenalidomide and were refractory to their most recent regimen.10
In Lacy et al's trial, responses to 2-mg and 4-mg doses of pomalidomide combined with dexamethasone were fast, from 1 to 2 months, and durable. With a median follow-up of 14 months, the median duration of response was not reached in the 2-mg cohort. Although a longer follow-up is required, the 6-month overall survival rates of 78% and 67% reported in the 2-mg and 4-mg cohorts are promising in a challenging population of patients for whom limited treatment options are available outside clinical trials.
As in other pomalidomide trials, toxicity consisted primarily of myelosuppression, although it was more pronounced than what was previously reported with this agent.8,9 Reduced hematopoiesis related to both advanced refractory disease and extensive prior treatments justifies the higher rates of grade 3-4 neutropenia (66% and 51% in the 4- and 2-mg cohorts, respectively) and thrombocytopenia (30.5% in both cohorts) observed in the current study compared with others. Nevertheless, the overall frequency of febrile neutropenia was low (0% and 11% in the 2- and 4-mg cohorts, respectively). The most common nonhematologic toxicity was fatigue. With adequate thromboprophylaxis and use of reduced-dose dexamethasone, thrombotic complications were observed in 4% of all patients. Grade 2 peripheral neuropathy (PN) possibly related to pomalidomide therapy was 11% in both cohorts, while grade 3 PN was 3% in the 4-mg cohort. However, it is worthy of note that the majority of these patients had baseline PN that worsened during pomalidomide treatment.
The lack of superiority with the higher over the lower pomalidomide dose reported by Lacy et al might suggest that for this drug there is no dose-response effect. However, before concluding that higher pomalidomide doses are useless, it should be noted that the shorter exposure to the study drug in the 4-mg compared with the 2-mg cohort (median number of 28-day cycles administered per patient: 3 vs 6, respectively) and comparable total doses of pomalidomide actually delivered in the 2 subgroups (median dose per patient: 12 mg in both cohorts) might have ultimately affected similar rates of response. This issue was not addressed by Lacy and colleagues, who continue to investigate the optimal dosing schedule of pomalidomide. In this context, a regimen of 4 mg on days 1 through 21 of each 28-day cycle compared with 2 mg continuously for 28 days is actually under investigation.
Pomalidomide represents a leap forward in myeloma care and serves as an important platform on which to build future rationally based combination strategies. In addition to pomalidomide, carfilzomib (PR-171), a novel generation proteasome inhibitor of the epoxyketone class, has shown remarkable single-agent activity and holds great promise in the setting of advanced rel/refr MM. Complementary to the development of newer immunomodulators and proteasome inhibitors, including salinosporamide (NPI-0052) and the novel orally bioavailable inhibitor MLN9708, a great number of investigational agents targeting novel pathways (such as histone deacetylase inhibitors, AKT/P13K/mTOR inhibitors, heat-shock-protein inhibitors, and monoclonal antibodies) have entered clinical testing. The armamentarium of available treatment options for MM continues to expand and it is likely that patient outcomes will continue to progressively improve in the coming years.
Conflict-of-interest disclosure: The author received honoraria from and is on the advisory boards for Janssen, Celgene, and Millennium. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal