Abstract
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare and aggressive malignancy derived from precursors of plasmacytoid dendritic cells. We analyzed 21 cases with array-based comparative genomic hybridization (aCGH). Complete or partial chromosomal losses largely outnumbered the gains, with common deleted regions involving 9p21.3 (CDKN2A/CDKN2B), 13q13.1-q14.3 (RB1), 12p13.2-p13.1 (CDKN1B), 13q11-q12 (LATS2), and 7p12.2 (IKZF1) regions. CDKN2A/CDKN2B deletion was confirmed by FISH. This scenario argues for disruption of cell cycle at G1/S transition, representing a genetic landmark of BPDCN, and possibly contributing to its pathogenesis. Statistical analysis of overall survival in our series highlighted an association of poor outcome with biallelic loss of locus 9p21.3. We suggest that, in the absence of reliable parameters for predicting prognosis in BPDCN other than age, tumor stage, and/or clinical presentation, simple methods, such as FISH for CDKN2A/CDKN2B, could help to identify the most aggressive cases.
Introduction
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare hematologic disease, often presenting in the skin.1-3 Its clinical course is aggressive in adults and apparently milder in children.4 Chemotherapy is the preferred treatment, along with allogeneic stem cell transplantation.5 Histologically, tumor cells may be either blastoid or pleomorphic6 and express several markers of plasmacytoid dendritic cells, such as CD123, TCL1, BDCA2, and CD2AP.7
Cytogenetic investigations have shown the predominance of genomic losses, affecting 5q21 or 5q34 (72%), 12p13 (64%), 13q13-q21 (64%), 6q23-qter (50%), 15q (43%), and the entire chromosome 9 (28%).8 More recently, array-based comparative genomic hybridization (aCGH) and gene expression profiling have highlighted peculiar chromosomal losses. In particular, Dijkman et al documented a decrease in RB1 and LATS2 oncosuppressor genes.9 Jardin et al showed loss of CDKN1B, CDKN2A, and TP53,10 and Wiesner et al confirmed deletions in several cell-cycle genes.11 Our study focused on 21 cases of BPDCN, combining clinicopathologic findings and genetic data to establish correlations with disease outcome.
Methods
Twenty-one cases of BPDCN were investigated, based on the availability of frozen material. Clinical characteristics are summarized in Table 1 and supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). This study was conducted in accordance with the Declaration of Helsinki, abiding by the rules of the research ethics committees of both participating institutions and was exclusively based on archival material.
Clinical picture, therapy, and follow-up for each patient
| Case no. . | Age (median 64 y)/sex ratio (5:2 male/female) . | Sites of involvement at diagnosis . | Initial treatment . | Response . | Relapse, months . | Sites of relapse . | Therapy at relapse . | Follow-up, months . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Skin (n = 21) . | BM (n =10) . | Peripheral blood (n =9) . | Lymph node (n =5) . | Other (n =2) . | ||||||||
| 1 | 64/M | Mu | + | + | − | − | ALL-type* | CR | 11 | S/BM/B | CHT | DOD 23 |
| 2 | 83/M | D | + | + | + | − | None | — | — | — | — | DOD 3 |
| 3 | 38/M | Mu | + | − | − | − | SCT | CR | 17 | S/BM/B/Ly | CHT | DOD 20 |
| 4 | 67/F | D | − | − | − | − | ALL-type* | PR | 5 | S | CHT | AWD 11 |
| 5 | 84/F | D | − | − | − | − | mCHT† | PR | 4 | B | — | DOD 6 |
| 6 | 64/M | D | + | + | − | − | ALL-type‡ | CR | 10 | S/BM/B | CHT | DOD 26 |
| 7 | 19/M | Mu | − | − | − | − | NHL-type§ | CR | 36 | S | SCT | AWD 72 |
| 8 | 62/M | Mu | + | + | + | − | ALL-type* | CR | — | — | — | ADF 13 |
| 9 | 61/M | Mu | − | − | − | − | NHL-type§ | CR | 30 | S/BM/B/Ly | CHT | DOD 35 |
| 10 | 83/M | D | + | + | − | MALT | NHL-type§ | PR | 8 | S/BM/B/O | CHT | DOD 10 |
| 11 | 40/M | L | − | − | − | − | mCHT† + RT | PR | 20 | BM/B | CHT | DOD 30 |
| 12 | 60/M | D | − | − | + | − | SCT | CR | — | — | — | DTR 60 |
| 13 | 76/M | L | − | − | − | − | RT | CR | 8 | BM | CHT | AWD 13 |
| 14 | 9/F | D | + | + | − | − | ALL-type* | CR | — | — | — | ADF 12 |
| 15 | 58/M | D | − | − | − | − | ALL-type* | CR | — | — | — | ADF 28 |
| 16 | 79/M | L | − | − | − | − | RT | CR | — | — | — | ADF 14 |
| 17 | 75/F | D | − | − | − | − | ALL-type* | CR | — | — | — | ADF 8 |
| 18 | 39/F | L | − | − | − | − | ALL-type*‖ | CR | — | — | — | DTR 12 |
| 19 | 66/F | Mu | + | + | − | − | NHL-type§ | PR | 5 | S/BM/B/O | CHT | DOD 20 |
| 20 | 64/M | D | + | + | + | MALT | ALL-type* | PR | 4 | S/B | SCT | DOD 12 |
| 21 | 83/M | L | + | + | + | − | None | — | — | — | — | DOD 1 |
| Case no. . | Age (median 64 y)/sex ratio (5:2 male/female) . | Sites of involvement at diagnosis . | Initial treatment . | Response . | Relapse, months . | Sites of relapse . | Therapy at relapse . | Follow-up, months . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Skin (n = 21) . | BM (n =10) . | Peripheral blood (n =9) . | Lymph node (n =5) . | Other (n =2) . | ||||||||
| 1 | 64/M | Mu | + | + | − | − | ALL-type* | CR | 11 | S/BM/B | CHT | DOD 23 |
| 2 | 83/M | D | + | + | + | − | None | — | — | — | — | DOD 3 |
| 3 | 38/M | Mu | + | − | − | − | SCT | CR | 17 | S/BM/B/Ly | CHT | DOD 20 |
| 4 | 67/F | D | − | − | − | − | ALL-type* | PR | 5 | S | CHT | AWD 11 |
| 5 | 84/F | D | − | − | − | − | mCHT† | PR | 4 | B | — | DOD 6 |
| 6 | 64/M | D | + | + | − | − | ALL-type‡ | CR | 10 | S/BM/B | CHT | DOD 26 |
| 7 | 19/M | Mu | − | − | − | − | NHL-type§ | CR | 36 | S | SCT | AWD 72 |
| 8 | 62/M | Mu | + | + | + | − | ALL-type* | CR | — | — | — | ADF 13 |
| 9 | 61/M | Mu | − | − | − | − | NHL-type§ | CR | 30 | S/BM/B/Ly | CHT | DOD 35 |
| 10 | 83/M | D | + | + | − | MALT | NHL-type§ | PR | 8 | S/BM/B/O | CHT | DOD 10 |
| 11 | 40/M | L | − | − | − | − | mCHT† + RT | PR | 20 | BM/B | CHT | DOD 30 |
| 12 | 60/M | D | − | − | + | − | SCT | CR | — | — | — | DTR 60 |
| 13 | 76/M | L | − | − | − | − | RT | CR | 8 | BM | CHT | AWD 13 |
| 14 | 9/F | D | + | + | − | − | ALL-type* | CR | — | — | — | ADF 12 |
| 15 | 58/M | D | − | − | − | − | ALL-type* | CR | — | — | — | ADF 28 |
| 16 | 79/M | L | − | − | − | − | RT | CR | — | — | — | ADF 14 |
| 17 | 75/F | D | − | − | − | − | ALL-type* | CR | — | — | — | ADF 8 |
| 18 | 39/F | L | − | − | − | − | ALL-type*‖ | CR | — | — | — | DTR 12 |
| 19 | 66/F | Mu | + | + | − | − | NHL-type§ | PR | 5 | S/BM/B/O | CHT | DOD 20 |
| 20 | 64/M | D | + | + | + | MALT | ALL-type* | PR | 4 | S/B | SCT | DOD 12 |
| 21 | 83/M | L | + | + | + | − | None | — | — | — | — | DOD 1 |
BM indicates bone marrow; Mu, multiple noncontiguous skin lesions; D, diffuse skin involvement; L, localized skin disease; Ly, lymph node; MALT, mucosa-associated lymphoid tissue; O, other; B, peripheral blood; ALL, acute lymphoblastic leukemia; SCT, allogeneic stem cell transplantation; mCHT, monochemotherapy; NHL, non-Hodgkin lymphoma; RT, radiotherapy; CR, complete remission; —, not available; PR, partial remission; S, skin; CHT, chemotherapy; DOD, dead of disease; AWD, alive with disease; ADF, alive disease-free; and DTR, death therapy-related.
Hyper-CVAD regimen (hyperfractionated cyclophosphamide, vincristine, doxorubicin, dexamethasone, alternating with high-dose methotrexate and cytarabine).
Hydroxyurea.
IVA regimen (ifosfamide, vincristine, actinomycin-D).
CHOP regimen (cyclophosphamide, doxorubicin, vincristine, prednisolone).
This patient had skin-limited disease at diagnosis, but she refused treatment until 8 months later when bone marrow involvement developed.
Immunohistochemistry (Dako Denmark) used the following antibodies: CD2, CD8, CD20, CD30, CD34, CD43, CD45RA, CD45RO, CD68, CD79a, CD117/c-kit, Bcl-2, granzyme B, Ki-67, LCA, LMP1, lysozyme, myeloperoxidase, perforin, S100, and TIA-1 (Dako Denmark); CD3, CD4, CD5, CD10, CD56, p16, and TdT (Novocastra); CD33 (Abcam); CD123 (BD Biosciences PharMingen); CD303/BDCA-2 (Dendritics); Tcl-1 (Cell Marque); and β-F1 and TCR-δ1 (Thermo Scientific).
DNA was extracted with QIAamp DNA Mini Kit (QIAGEN). Genome-wide aCGH used Human Genome CGH Microarray Kit, 44K (Agilent Technologies). Cases carrying locus 9p21.3 deletion were tested by dual-color FISH,12 with 9p21 (SpectrumOrange) probes (Abbott Molecular). PCR for IGHV and TCRγ-chain genes was performed as previously described.13 In situ hybridization for EBV used probes for EBV-encoded early RNAs (Dako Denmark).
Statistical analysis was performed with Kaplan-Meier survival and Cox multivariate analyses, and the log-rank test, using MedCalc Version 11.4 software.
Results and discussion
Median survival was 13 months. At onset, all patients had cutaneous involvement, with diffuse lesions in 10 cases (47.6%), and multiple noncontiguous or localized tumors in the remainder (supplemental Figure 1). The rate of bone marrow involvement was higher in cases with multiple noncontiguous or diffuse skin lesions (62.5%) compared with localized (20.0%; P = .91). The 11 patients with extracutaneous disease at diagnosis (52.4%) had a median survival of 13 months, compared with 28 months for skin-restricted forms. Specific therapy was administered in 19 cases. Twelve patients relapsed (57.1%; median time to relapse, 10 months), with negative correlation between age and time to relapse (P = .0053). At last follow-up, 11 patients (52.4%) had died of disease.
Ten cutaneous biopsies showed pleomorphic histology, although in the absence of correlation with overall survival or aberrant immunophenotype. The latter was typical in all but 3 cases (14.3%), which were negative for CD4, CD56, or both. In addition, CD2 and/or CD7 were aberrantly expressed in 9 biopsies (42.8%) (supplemental Table 2; supplemental Figure 2), with CD2+ cases experiencing a median survival of 35 months. All 3 patients with TdT+ tumors had bone marrow involvement at diagnosis. Bone marrow findings are illustrated in supplemental Figure 3.
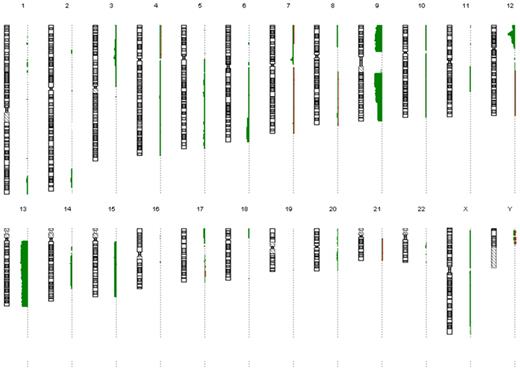
There was a mean of 7 copy number alterations per case (always detected in cellular mosaic), with prevalence of losses over gains (141 vs 18), and of large interstitial/telomeric imbalances over losses/gains of entire chromosomes (127 vs 32; Figure 1; supplemental Table 3). Most affected were chromosomes 9 (71%), 13 (61%), 12 (57%), 5 (19%), 7 (19%), 14 (19%), and 15 (14%), with common deleted regions (CDRs). Deletion of 9p21.3 locus was identified in 14 patients (66.6%, 5 homozygous, 9 hemizygous), ranging from 21.003 Mb to 21.980 Mb and containing CDKN2A (cyclin-dependent kinase inhibitor 2A, p16INK4a), CDKN2B, and MTAP (5′-methylthioadenosine phosphorylase). These deletions were also confirmed by FISH (hemizygous, 9 cases; homozygous, 3 cases; chromosome 9 monosomy, 2 cases; supplemental Figure 4). In addition, immunohistochemistry for p16INK4a was negative on all biopsies. Chromosome 13 monosomy was found in 52.4% of samples: a CDR on 13q13.1-q14.3 involved RB1 (retinoblastoma 1), CCNA1 (cyclin A1), and KPNAP3 (karyopherin α 3), hsa-mir-320d-1, hsa-mir-621, hsa-mir-16–1, and hsa-mir-15a. Another CDR on 13q11-q12 encompassed LATS2 (52.4%). A minimal CDR occurred on 12p13.2-p13.1 (57.1%), from 12.247 Mb to 14.491 Mb, including CDKN1B (cyclin-dependent kinase inhibitor 1B). 7p12.2 was the target of a CDR encompassing IKZF1 (IKAROS family zinc finger 1, 19.0%). The deletion of Ikaros protein has been associated with poor outcome in BCR-ABL1+ acute lymphoblastic leukemias.14,15 In our series, 2 patients bearing this anomaly had leukemic spread at diagnosis, with accelerated fatal course.
Copy number alterations detected by aCGH. Summary of the chromosomal losses and gains detected by aCGH in our patients (chromosomes are shown as ideograms). The positions of oligomers refer to Human Genome March 2006 assembly (hg18). In each experiment, log2 ratios estimated the percentage of anomalous cells for each copy number alteration. Green bars on the left side of each chromosome represent chromosomal losses; and red bars, chromosomal gains. The width of the bars is proportional to the occurrence of a given anomaly in the 21 analyzed samples.
Copy number alterations detected by aCGH. Summary of the chromosomal losses and gains detected by aCGH in our patients (chromosomes are shown as ideograms). The positions of oligomers refer to Human Genome March 2006 assembly (hg18). In each experiment, log2 ratios estimated the percentage of anomalous cells for each copy number alteration. Green bars on the left side of each chromosome represent chromosomal losses; and red bars, chromosomal gains. The width of the bars is proportional to the occurrence of a given anomaly in the 21 analyzed samples.
The 4 most frequent CDR (9p21.3, 13q13.1-q14.3, 12p13.2-p13.1, and 13q11-q12) contain several genes controlling G1/S transition of cell cycle, including, respectively, CDKN2A/CDKN2B, RB1, CDKN1B, and LATS2.16-18 Biallelic loss and/or multiple heterozygous deletions of these genes were detected in > 90% of cases. Being infrequent in tumors both of lymphoid or myeloid derivation,19,20 the aforementioned genetic anomalies might delineate a specific oncogenic pathway for BPDCN. Only 2 cases (patients 20 and 21) lacked these anomalies, in the absence of distinctive clinical features. We cannot exclude epigenetic silencing or mutations in these few instances. In addition, patients 16 and 18 were father and daughter, suggesting that germline variations may have a role as well.
The largest series of BPDCN have suggested that survival may be related to age, tumor stage, and clinical presentation.21 In one series, patients presenting with solely cutaneous lesions survived longer,22 and this was also the case for our patients. Our cases were diagnosed at different points in time and received heterogeneous treatments. Those undergoing allogeneic stem cell transplantation, either at diagnosis or at relapse, had the highest benefit (median survival, 60 months).
The deletion of 9p21.3 locus was the most recurrent event. Although seen in many cancers, this loss has been associated with poor prognosis in systemic diffuse large B-cell lymphomas,23 primary cutaneous diffuse large B-cell lymphoma leg-type,24 and mycosis fungoides/Sézary syndrome.12 In our series, median overall survival was 11 months for cases with homozygous loss, compared with 26 months for hemizygous loss. Even if we cannot rule out functional inactivation of the remaining allele in the latter group,25 univariate analysis for overall survival with the Kaplan-Meier method revealed reduced survival probability among patients with biallelic loss (hazard ratio = 11.98; CI, 1.21-118.96; log-rank test, P = .0349; supplemental Figure 5). All 5 cases with homozygous loss had multiple noncontiguous or diffuse skin lesions, whereas 2 patients in the hemizygous group had localized skin disease (P = .64). Patients with multiple noncontiguous or diffuse skin lesions had 2-fold higher 9p21.3 locus losses (81.2%) compared with those with localized disease (40.0%; P = .22). Multivariate analysis, using the Cox proportional hazards model (covariates: locus 9p21.3 loss; distribution of skin lesions; treatment modality), defined homozygous loss of locus 9p21.3 as a basically independent adverse prognostic factor (P = .06).
In conclusion, beyond representing a potential oncogenetic event in BPDCN, the deletion of p16INK4a also affects prognosis. In the effort to identify patients at higher clinical risk, simple assays, such as PCR or FISH for 9p21.3 locus, might improve current diagnostic standards. Other studies should verify our observations, possibly combining multiple ligation-dependent probe amplification, mutational analysis, and methylation assay for CDKN2A/CDKN2B genes.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Alessandra Viglio (Anatomic Pathology Section, Fondazione IRCCS Policlinico San Matteo, Italy) for her outstanding assistance in manuscript revision.
M.A. and E.D. are recipients of a fellowship from Anatomic Pathology Section, IRCCS Fondazione Policlinico “San Matteo,” Pavia, Italy.
Authorship
Contribution: M.P., M.L., and E. Berti designed the study and wrote the paper; M.L., F.N., G.F., R.R., D.F., M.A., E.D., E.T., and O.Z. performed the research and analyzed the data; L.A., F.O., P.V., and E. Berti collected the clinical data; E. Boveri, L.V., and M.N. provided important suggestions both during the study and in writing; and all authors checked the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marco Lucioni, Anatomic Pathology Section, Foundation IRCCS Policlinico San Matteo, Via Forlanini 14, 27100 Pavia, Italy; e-mail: m.lucioni@smatteo.pv.it.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal