Abstract
The baseline characteristics and therapeutic management of sickle cell disease (SCD) can be quite variable depending on disease severity. This report describes baseline assessments and therapies of 420 patients in an ongoing registry designed to study current treatment patterns, natural history, and outcomes in patients with SCD.
This registry trial involving 57 US hematology centers had a sequential recruitment target of 600 patients with SCD subdivided into 3 age groups (2-<12 yr, 12-<18 yr, ≥18 yr). Patients '2 years of age with HbSS, HbS/β-thalassemia, or HbSC were eligible. Follow-up visits were every 6 months for a maximum of 5 years. Assessments included demographics, SCD history, Karnofsky Performance Status, medical history, types of crises, frequency of crises and hospitalization, treatment history, transfusion practices and use of iron chelation. Differences between pediatric (<18 yrs) and adult (≥18 yrs) patients were examined. (ClinicalTrials.gov identifier, NCT01220115).
Enrollment: 420 patients (254 <18 yrs, 166 ≥18 yrs) completed the initial baseline visit. Baseline characteristics and medical history are shown in the Table and Figure.
Baseline characteristics of patients enrolled in registry trial
| . | <18yrs (N=254) n (%)* . | ≥18yrs (N=166) n (%)* . |
|---|---|---|
| Age, yrs – mean±SD | 8.9 ± 4.5 | 35.5 ± 12.4 |
| Sex, M:F – % | 58:43:00 | 48:52:00 |
| Karnofsky Performance Status | 98 (38.6) | 23 (13.9) |
| 100% | 69 (27.2) | 50 (30.1) |
| 90% | 23 (9.1) | 56 (33.7) |
| ≤80% | ||
| Type of SCD | 193 (76.0) | 117 (70.5) |
| HbSS | 27 (10.6) | 16 (9.6) |
| HbS/β-thalassemia | 32 (12.6) | 33 (19.9) |
| HbSC | ||
| Transfusions | 54 (21.3) | 29 (17.5) |
| Regular (≥6/yr) | 58 (22.8) | 49 (29.5) |
| Intermittent (<6/yr) | 134 (52.8) | 73 (44.0) |
| No transfusions in last 12 months | ||
| Serum ferritin, ng/ml – Median (range) | 435 (15–10054) | 702.5 (6–19362) |
| Liver iron concentration: biopsy, mg/g – Median (range) | 7.068 (1.070–27.115) | – |
| Chelation, patients receiving in their lifetime | 56 (22.0) | 52 (31.3) |
| Hospitalizations | 0.80 (0.2–4.4) | 0.60 (0.2–5.2) |
| Number/yr/patient – median (range) | 218 (85.8) | 122 (73.5) |
| Patients hospitalized in last 5 years | ||
| Concomitant medical history | 27 (10.6) | 15 (9.0) |
| Aplastic episode | 77 (30.3) | 23 (13.9) |
| Asthma/reactive airway disease | 7 (2.8) | 48 (28.9) |
| Avascular necrosis, hip(s)/shoulder(s) | 20 (7.9) | 5 (3.0) |
| CNS disease, abnormal TCD | 14 (5.5) | 11 (6.6) |
| CNS disease, seizure | 19 (7.5) | 9 (5.4) |
| CNS disease, silent infarct | 8 (3.1) | 9 (5.4) |
| CNS disease, TIA | 60 (23.6) | 12 (7.2) |
| Dactylitis (hand food syndrome) | 35 (13.8) | 71 (42.8) |
| Gall bladder disease | 0 (0.0) | 15 (9.0) |
| Leg ulcer | 2 (0.8) | 13 (7.8) |
| Lung disease, pulmonary hypertension | 57 (22.4) | 14 (8.4) |
| Splenic sequestration | ||
| Hydroxyurea use | 101 (39.8) | 64 (38.6) |
| . | <18yrs (N=254) n (%)* . | ≥18yrs (N=166) n (%)* . |
|---|---|---|
| Age, yrs – mean±SD | 8.9 ± 4.5 | 35.5 ± 12.4 |
| Sex, M:F – % | 58:43:00 | 48:52:00 |
| Karnofsky Performance Status | 98 (38.6) | 23 (13.9) |
| 100% | 69 (27.2) | 50 (30.1) |
| 90% | 23 (9.1) | 56 (33.7) |
| ≤80% | ||
| Type of SCD | 193 (76.0) | 117 (70.5) |
| HbSS | 27 (10.6) | 16 (9.6) |
| HbS/β-thalassemia | 32 (12.6) | 33 (19.9) |
| HbSC | ||
| Transfusions | 54 (21.3) | 29 (17.5) |
| Regular (≥6/yr) | 58 (22.8) | 49 (29.5) |
| Intermittent (<6/yr) | 134 (52.8) | 73 (44.0) |
| No transfusions in last 12 months | ||
| Serum ferritin, ng/ml – Median (range) | 435 (15–10054) | 702.5 (6–19362) |
| Liver iron concentration: biopsy, mg/g – Median (range) | 7.068 (1.070–27.115) | – |
| Chelation, patients receiving in their lifetime | 56 (22.0) | 52 (31.3) |
| Hospitalizations | 0.80 (0.2–4.4) | 0.60 (0.2–5.2) |
| Number/yr/patient – median (range) | 218 (85.8) | 122 (73.5) |
| Patients hospitalized in last 5 years | ||
| Concomitant medical history | 27 (10.6) | 15 (9.0) |
| Aplastic episode | 77 (30.3) | 23 (13.9) |
| Asthma/reactive airway disease | 7 (2.8) | 48 (28.9) |
| Avascular necrosis, hip(s)/shoulder(s) | 20 (7.9) | 5 (3.0) |
| CNS disease, abnormal TCD | 14 (5.5) | 11 (6.6) |
| CNS disease, seizure | 19 (7.5) | 9 (5.4) |
| CNS disease, silent infarct | 8 (3.1) | 9 (5.4) |
| CNS disease, TIA | 60 (23.6) | 12 (7.2) |
| Dactylitis (hand food syndrome) | 35 (13.8) | 71 (42.8) |
| Gall bladder disease | 0 (0.0) | 15 (9.0) |
| Leg ulcer | 2 (0.8) | 13 (7.8) |
| Lung disease, pulmonary hypertension | 57 (22.4) | 14 (8.4) |
| Splenic sequestration | ||
| Hydroxyurea use | 101 (39.8) | 64 (38.6) |
n (%) unless otherwise indicated.
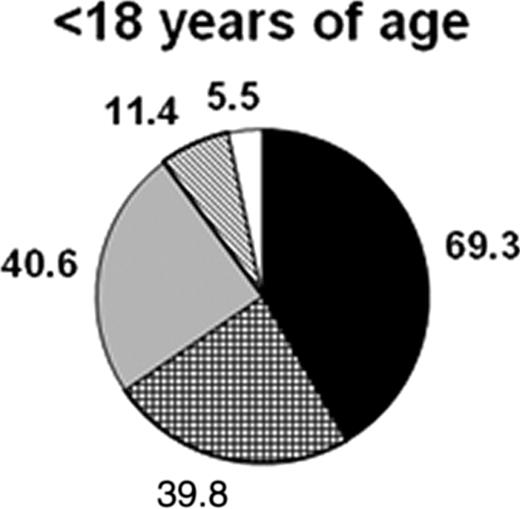
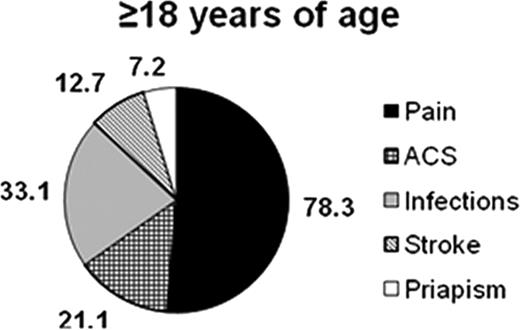
Types of crises experienced (percentage of patients). Incidence over the past 5 years is shown for all except stroke, which is shown as lifetime incidence.
Types of crises experienced (percentage of patients). Incidence over the past 5 years is shown for all except stroke, which is shown as lifetime incidence.
These data indicate differences in baseline characteristics and treatment patterns between adult and pediatric patients with SCD in this registry. Karnofsky performance status was worse, and serum ferritin levels were higher in adult versus pediatric patients. The percentage of patients having regular transfusions was higher in pediatric patients, while adult patients had higher rates of intermittent transfusions. As expected, the lifetime chelation exposure was more frequent in adult patients. Hospitalizations and use of hydroxyurea were also greater in pediatric patients. In terms of medical history related to SCDs, pediatric patients had higher frequencies of asthma, abnormal TCDs, dactylitis and splenic sequestration, while adults had more frequent evidence of avascular necrosis, gall bladder disease, leg ulcers and pulmonary hypertension. Pain was the most common crisis type in both cohorts, although this accounted for a greater relative proportion of crises in the adult cohort. The relative proportion of ACS events was lower in the adult versus pediatric patients; all other crisis types occurred in similar relative proportions in both cohorts. This ongoing registry will provide information about disease patterns, current treatment practices, and outcomes, thus contributing to a better understanding of the appropriate therapeutic management of patients with SCD.
Heeney:Novartis: Consultancy, Research Funding. Baltz:Novartis: Research Funding. Paley:Novartis: Employment. Esposito:Novartis: Employment. Sharma:Novartis: Employment. Vichinsky:Novartis, Apotex, Ferrokin: Research Funding.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal