Abstract
Abstract 1228
Thiazolidinediones (TZDs) are agonists of PPARγ which favorably modify metabolic parameters and markers of atherosclerosis among type 2 diabetics. Enucleate platelets express PPARγ protein, and PPARγ agonists blunt release of CD40L and thromboxane B2 (TXB2) from thrombin-activated platelets. (Abbiyik, F et al, Human bone marrow megakaryocytes and platelets express PPARγ and PPARγ agonists blunt platelet release of CD40 ligand and thromboxanes. Blood, 2004 104(5):p.1361–8.) Diabetic subjects disproportionately experience arterial thromboses despite aspirin therapy. We assessed platelet function after pioglitazone in two risk groups in the presence and absence of aspirin to characterize its range of antiplatelet effect.
20 diabetic and 20 non-diabetic subjects were enrolled in a prospective study. Exclusion criteria among all subjects included current use of antiplatelet, anticoagulants, or pioglitazone, bleeding disorder, renal or liver disease, congestive heart failure, pregnancy or hypersensitivity to aspirin or pioglitazone. Non-diabetic subjects were excluded for BMI > 30 kg/m2, cardiovascular disease or risk factors. All subjects previously on aspirin underwent a 7 day minimum “wash-out” period.
Four separate blood samples from each subject were collected on 2 separate days separated by a 7 day interval. On day 1, a baseline blood sample was obtained followed by a second blood sample 3 hours after ingestion of 30 mg pioglitazone. Subjects returned 1 week later after having taken a single 81 mg aspirin 2–3 hours before arrival. Samples 3 and 4 were collected in the same manner as during week 1. Platelet rich plasma (PRP) was immediately prepared and platelet aggregation performed by the turbidometric method of Born with simultaneous measurement of ATP release. ADP (5M and 10M), arachidonic acid (0.5mM) and collagen (2g/mL) were used as agonists. PRP was activated with 0.8 unit/ mL thrombin for subsequent ELISA assays of TXB2 (Thromboxane B2), TGF-β (Transforming Growth Factor-Beta) and CD40L (CD 40 Ligand).
By Diabetic Status: a.) Baseline platelet aggregations, ATP release and ELISAs were similar between diabetic and non-diabetic subjects, with the exception of platelet aggregation using 5 uM and 10uM as agonist. b.) Mean maximum platelet aggregation after aspirin alone was 20% higher among diabetic subjects.
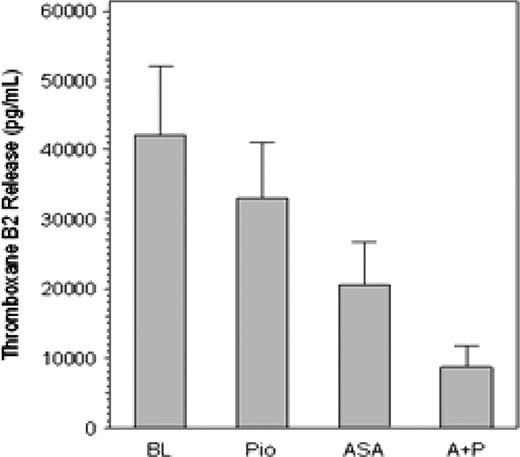
lp;&0.5qAmong all Subjects: a.) Mean TXB2 release among all subjects was reduced from a baseline of 42,075 ± 4,479 pg/ml to 32,719 ± 3,589pg/ml after pioglitazone alone (p = 0.0004).
b.) Mean TXB2 release after aspirin alone was 20,829 ± 2,753 pg/ml which was reduced to 9,569 ± 1,653 pg/ml after the addition of pioglitazone (p = 0.0001). (Figure 1)
Thromboxane B2 release. Data are mean ± SEM (pg/ml) for all patients at baseline (BL), after pioglitazone alone (Pio), after aspirin alone (ASA) and after both aspirin and pioglitazone (A+P). Release with Pio alone was significantly less than at BL (p =.0004), and release with A + P was significantly less than with ASA alone (p <.0001).
Thromboxane B2 release. Data are mean ± SEM (pg/ml) for all patients at baseline (BL), after pioglitazone alone (Pio), after aspirin alone (ASA) and after both aspirin and pioglitazone (A+P). Release with Pio alone was significantly less than at BL (p =.0004), and release with A + P was significantly less than with ASA alone (p <.0001).
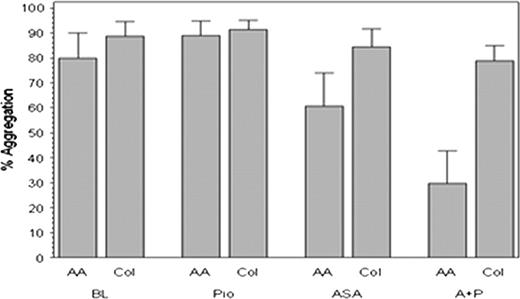
c.) Twenty-five of 40 subjects (63%) had aggregation of greater than 20% using arachidonic acid as agonist despite ingestion of 81 mg aspirin. This decreased to 11 /40 (28%) after the administration of 30 mg of pioglitazone (p < 0.0001). (Figure 2)
Platelet aggregation with arachidonic acid and collagen. At each time point the results are shown for maximum % aggregation (mean ± SEM) with arachidonic acid (AA) and collagen (Col). Baseline (BL), after pioglitazone alone (Pio), after aspirin alone (ASA), and after both aspirin and pioglitazone (A+P). The numbers at the top of each bar represent the mean value.
Platelet aggregation with arachidonic acid and collagen. At each time point the results are shown for maximum % aggregation (mean ± SEM) with arachidonic acid (AA) and collagen (Col). Baseline (BL), after pioglitazone alone (Pio), after aspirin alone (ASA), and after both aspirin and pioglitazone (A+P). The numbers at the top of each bar represent the mean value.
No significant effects were observed on release of CD40L or TGFβ.
Pioglitazone has a direct platelet stabilizing effect and potentiates the effect of aspirin irrespective of underlying cardiovascular risk.
Francis:Takeda Pharmaceuticals North America, Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal