Abstract
Abstract  2121
2121
Pulmonary hypertension is associated with increased mortality in patients with sickle cell disease (SCD). Although recent studies suggest that echocardiography-assessed elevation in the tricuspid regurgitant (TR) jet velocity may over-estimate the prevalence of PHT, elevated TR jet velocity is recognized as an independent predictor of mortality in this patient population. Because of this association with mortality, many experts recommend routine screening of SCD patients with Doppler echocardiography. However, the rate of progression of the TR jet velocity and the predictive markers of such progression are unknown in this patient population.
We evaluated echocardiography-derived TR jet velocities obtained from patients participating in an ongoing study of pulmonary hypertension at the University of North Carolina, Chapel Hill. Patients with more than one measurable TR jet velocity were evaluated for progression. The data were dichotomized to evaluate for associations between increased TR jet velocity vs. no increase in TR jet velocity (decreased or no change). We also evaluated for any associations between increased TR jet velocity and clinical and laboratory covariates using individual logistic regression models for each variable, comparing the values of variables in the subjects with increased TR jet velocity to those with no increase in TR jet velocity. For continuous variables, a Wilcoxon rank sum test was performed. For dichotomous variables, Fishers Exact test was performed. Due to the exploratory nature of this study, reported p-values were not adjusted for multiple comparisons.
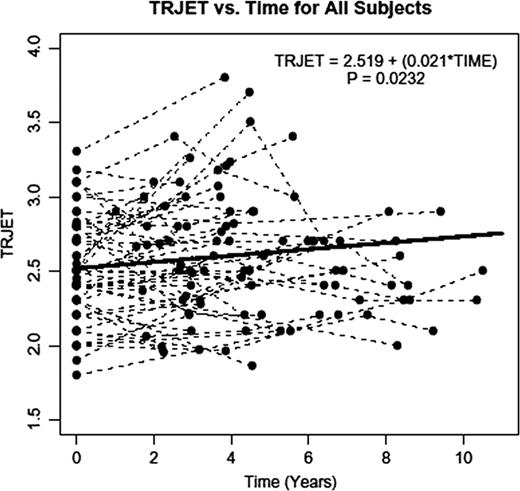
Fifty five patients (30 female and 25 male), with a median age of 38.0 years (range: 20 – 65 years) had at least 2 measurable TR jet velocities and were followed for a median of 4.52 years (range 1.02–10.5 years). Thirty one patients (56%) showed an increase in TR jet velocity while 24 patients (44%) showed no change or decrease in TR jet velocity. The model predicted an initial TR jet velocity of 2.52 m/s and a rate of increase in TR jet velocity of 0.021 m/s per year (p = 0.023) for all the patients. For those patients with an increase in TR jet velocity, the model predicted a rate of increase of 0.071 m/s per year. The level of placental growth factor may be lower in subjects with increased TR jet velocity compared to those with no increase in TR jet velocity (4.48 pg/mL vs. 9.85 pg/mL, p = 0.071), although this result was based only on eight patients with multiple measurements. No associations were observed between increase in TR jet velocity and age, weight, systolic blood pressure, WBC count, hemoglobin, platelet count, reticulocyte count, fetal hemoglobin, lactate dehydrogenase, total bilirubin, or history of acute chest syndrome. For subjects not receiving any therapeutic interventions for SCD-related complications (hydroxyurea or ACE inhibitors/ARBs), the model predicted an initial TR jet velocity of 2.61 m/s, and an increase in TR jet velocity over time of 0.019 m/s per year (p=0.16). Patients on hydroxyurea at the onset (N=26) were predicted to have an initial TR jet velocity that was 0.202 m/s lower than subjects not on hydroxyurea (p = 0.036). Patients on hydroxyurea were also predicted to have a slower increase in the TR jet velocity of 0.015 m/s per year, although this was not statistically different from those not on any interventions (p = 0.83). Patients on ACE inhibitors/ARBs were predicted to have an initial TR jet velocity that was 0.029 m/s higher than subjects not on such interventions (p=0.85). Furthermore, they were predicted to have an increase in their TR jet velocity of 0.058 m/s per year, although this was not statistically different from patients not on any therapeutic interventions (p=0.20).
TR jet velocity appears to increase over time in patients with SCD. Patients on treatment with hydroxyurea have lower baseline TR jet velocities compared to those who are not on such therapy. Furthermore, hydroxyurea may decrease the progression of TR jet velocity. With the association of increased TR jet velocity with mortality, periodic echocardiography to assess TR jet velocity is warranted in patients with SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal