Abstract
Abstract 3906
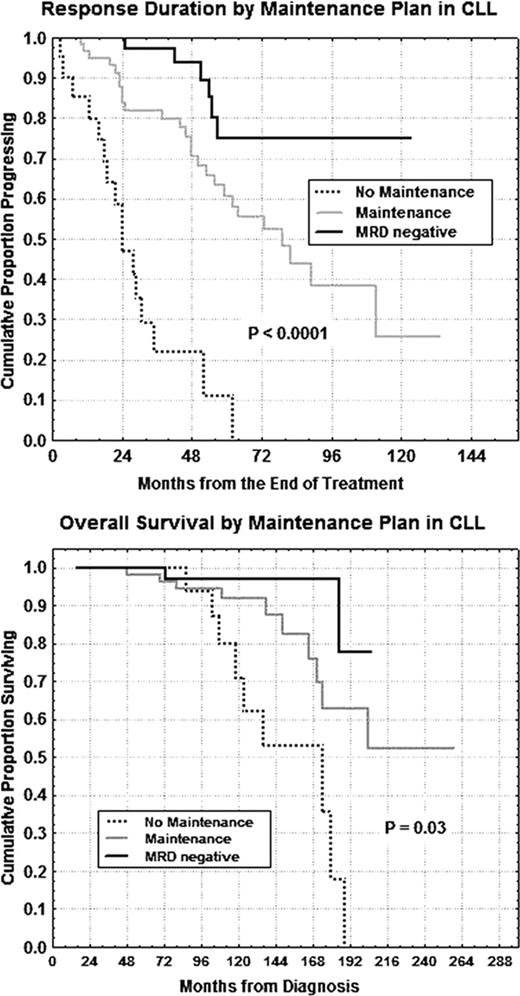
Today the treatment target of CLL is the attainment of an optimal disease control combining chemotherapy with monoclonal antibodies (MoAbs). This approach produces more complete molecular remissions and longer response duration (RD), remaining often a minimal residual disease (MRD) detectable by flow cytometry. In addition, consolidation and maintenance therapy with MoAbs might provide a further RD and overall survival (OS) benefit in CLL, as it has been already clearly demonstrated in indolent non-Hodgkin lymphomas. We treated in first line 145 CLL symptomatic patients (pts), median age 63 years (37–80), with six monthly courses of intravenous (25 mg/m2) or oral fludarabine (30–40 mg/m2) and then, after a median time of 30 days, with four weekly doses (375 mg/m2) of rituximab (rtx). Before treatment, 15 pts had a modified low Rai stage, 127 an intermediate stage and only 3 a high stage. We defined as high risk pts having at least two of these markers: unmutated IgVH, CD38>30%, ZAP-70>20%, intermediate/poor cytogenetics (trisomy 12 or del11q or del17p). Sixty-three pts (43.5%) belonged to the high risk subset. For MRD flow cytometric study, the threshold was set at >1% CD19+CD5+CD79b+/− bone marrow (BM) CLL cells. Based on NCI criteria (Cheson, 1996), 111/145 (76%) pts achieved a complete remission (CR), 27/145 (19%) a partial remission (PR) and 7/145 (5%) no response or progression. Phenotypic CR (CD19+CD5+CD79b- BM cells <1%) was achieved in 85/145 (59%) CLL pts. Interestingly, MRD+ pts showed a significant shorter overall survival (OS) in comparison with MRD- pts (25% vs 73% at 16 years, P=0.00096). During the induction and consolidation/maintenance time, 13 pts underwent grade 2–3 (sec.WHO) infective lung toxicity and 2 pts progressed towards Richter's syndrome. Hematologic toxicity was mild including mainly neutropenia (grade 3 and/or 4 in 60 pts) and thrombocytopenia (grade 3 and/or 4 in 9 pts). Fifty-nine pts (43%) either in CR with B-CLL BM cells >1% (MRD+, n=16 pts) or in CR MRD negative, but developing MRD positivity within 2 years after induction (n=25 pts) or in PR (n=18 pts), underwent consolidation and maintenance therapy with four monthly cycles of rtx at 375 mg/m2 followed by twelve monthly doses of rtx at 150 mg/m2. The median follow-up duration was 63 months. Noteworthy, both persistently MRD negative pts (n=56) and pts undergoing consolidation/maintenance therapy (n=59) showed a longer RD vs MRD+ not consolidated pts (n=23) [75% vs 58% vs 0% at 5 years; P<0.0001, Figure]. Equally, OS was shorter in MRD+ not consolidated pts in comparison with the other two subsets (0% vs 63% vs 78% at 16 years; P=0.03, Figure). Moreover, ZAP-70+ or unmutated IgVH pts revealed shorter RD (17% vs 53% at 16 years, P=0.001; 16% vs 53% at 6.5 years, P<0.0001). Noteworthy, within the high risk subset (n=63), pts in persistent phenotypic CR (n=18) and consolidated pts (n=23) showed a longer RD (90% vs 66% vs 8% at 2.7 years, P=0.00024) vs MRD+ not consolidated pts (n=15). In multivariate analysis, only consolidation/maintenance (P<0.0001) and biologic risk classes (P=0.001 and P<0.0001) were confirmed as independent prognosticators with regard to RD and OS. Therefore rituximab consolidation/maintenance therapy improve RD and OS in CLL, also within the high risk subset, taking into account that historical biological markers (ZAP-70 and IgVH mutational status) retain their prognostic impact with our chemoimmunotherapeutic strategy.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal