Abstract
Abstract 4077
The reported incidence of chronic graft-versus-host disease (cGVHD) after cord blood transplant (CBT) varies widely in the literature, with some studies suggesting that cGVHD is more responsive to treatment after CBT than after conventional hematopoietic cell transplant (HCT). The 2005 National Institutes of Health (NIH) consensus criteria were designed to standardize the diagnosis and scoring of cGVHD. While these criteria have been used to evaluate GVHD after bone marrow (BMT) and mobilized blood (PBSCT) cell transplantation, analysis of GVHD after CBT by NIH criteria has been limited. We report the results of a single-center, prospective analysis of GVHD evaluated according to the NIH diagnostic criteria in adults and children receiving unrelated CBT after high or reduced-intensity conditioning.
Eighty-seven consecutive patients who received a first single or double CBT between 2006 and 2011 were included. GVHD prophylaxis consisted of cyclosporine and mycophenolate mofetil. Grafts were HLA-typed at the antigen level for HLA-A and B, and high resolution for HLA-DRB1. Patients were prospectively evaluated for GVHD at day 80, 1-year, and at any other time as clinically indicated.
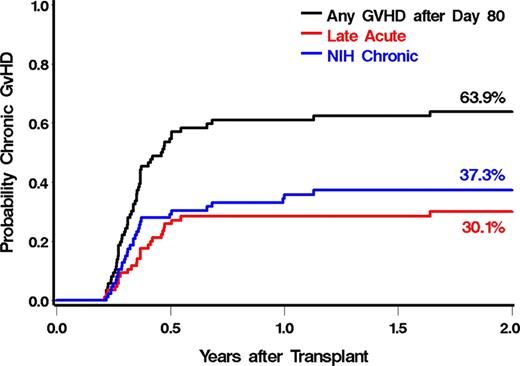
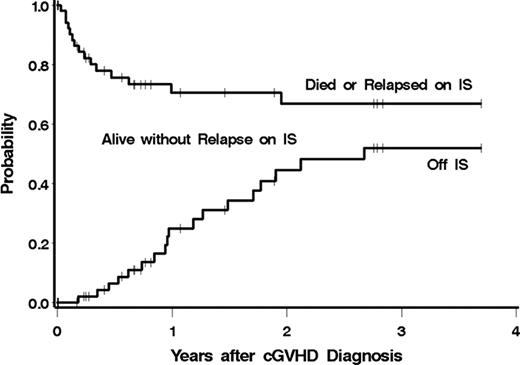
Median patient age was 31 years (range 0.8–70). Diagnosis at transplant included AML (n=49), ALL (n=20), CML (n=5), MDS/MPD (n=5), and other hematologic malignancy (n=8). The median follow-up after CBT was 24 months (range 1–127). Most patients received high-intensity conditioning (79%, n=69) and a double CB graft (86%, n=75). HLA-matching was 4/6 in 59% (n=51) of patients, 5/6 in 37% (n=32), and 6/6 in 4% (n=4). Median total infused cell doses were: 3.8 × 107 TNC/kg, 0.21 × 106 CD34+ cells/kg, and 10.9 × 106 CD3+ cells/kg. Neutrophil engraftment occurred in 90% of patients (n=78), at a median of 22 and 13 days after high and reduced-intensity conditioning, respectively. The cumulative incidence (CI) of grades II-IV and III-IV acute GVHD (aGVHD) was 74.7% and 29.9%, respectively. Sixty-eight patients (78%) were alive, engrafted with donor cells, and without relapse at day 80. Fifty-four patients had GVHD requiring systemic immunosuppressive treatment after day 80, for an estimated 2-year CI of 64%. Most patients had quiescent or interrupted onset (69%) and 48% had thrombocytopenia at time of diagnosis. By NIH criteria, 25 patients presented with “late” acute GVHD, and 29 presented with NIH cGVHD. Two patients who presented with “late” acute GVHD subsequently developed NIH cGVHD (Figure 1). Most patients with “late” acute GVHD had recurrent acute GVHD (n=20) with a median onset at 141 days after CBT (range 77–599). Organs affected by “late” acute GVHD were the GI tract (n=17), skin (n=12), and liver (n=5). Of the 31 patients with NIH cGVHD, 7 developed only the classic subtype with a median onset at 123 days after CBT (range 91–363). Organs affected in patients with classic NIH cGVHD were mouth (n=5), skin (n=5), lung (n=1), serosa (n=2), and genital (n=1). Most patients with NIH cGVHD had the overlap subtype (n=24), occurring at a median of 114 days after CBT (range 80–412). Organs involved in the overlap subtype included the GI tract (n=22), liver (n=7), acute skin (n=9), chronic skin (n=6), mouth (n=21), eyes (n=3), lung (n=1), esophagus (n=1), and serosa (n=3). The estimated 3-year CI of discontinuing immunosuppressive therapy (IST) while alive without relapse was 52%, while the 3-year estimated CI of death or relapse during IST was 33% (Figure 2). Among those who discontinued IST, the median time from onset of late acute GVHD or NIH cGVHD to discontinuation of IST was 12 months. In a previous study, the median time to discontinuation of IST for patients with cGVHD after BMT or PBSCT was 23 months.
Estimated Probability of Discontinuing Immunosuppressive Therapy after Diagnosis of Chronic GVHD after CBT
Estimated Probability of Discontinuing Immunosuppressive Therapy after Diagnosis of Chronic GVHD after CBT
Despite a highly HLA-mismatched donor source, the CI of cGVHD after CBT is comparable to that after conventional HLA-matched unrelated donor HCT previously reported from our center. Our results indicate that GVHD occurring after day 80 post CBT frequently manifests itself as acute GVHD predominantly involving the GI tract. More importantly, these preliminary results suggest that time to resolution of GVHD diagnosed after day 80 appears to be shorter after CBT compared to after BMT or PBSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal