Abstract
Abstract 4120
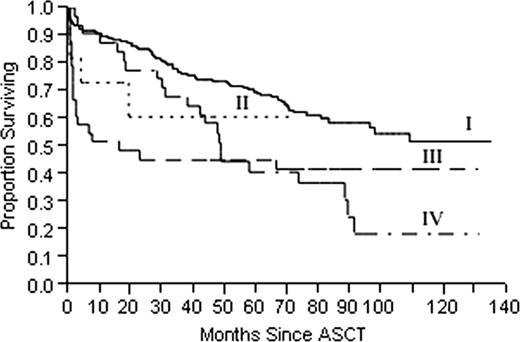
Autologous stem cell transplantation (ASCT) remains an effective treatment for immunoglobulin light chain (AL) amyloidosis but its high treatment related mortality is a concern. The development of acute renal failure can strongly affect the survival of these patients. This study looks at the impact of the timing of dialysis initiation on the overall survival (OS). Methods: AL patients who underwent ASCT from 3/96 to 1/10 were selected. Patients were placed into 4 groups: I - never dialyzed, II - initiated dialysis prior to ASCT, III - dialysis began within 30 days of ASCT and IV - dialysis was started after 30 days of ASCT. Results: Four hundred and ten patients were selected for study and 75 (18.3%) received dialysis. Baseline characteristics are listed in Table 1. In univariate analysis, serum creatinine (Scr) and b-2 microglobulin (b2m) were associated with dialysis post-ASCT. Both became non-significant in the multivariate model suggesting they are co-dependent. Dialysis had a strong influence on survival, p < 0.001 (Fig 1). This was most evident when dialysis was started after ASCT (group III (p = 0.003) and IV (p = 0.004)), but not before (II, p = 0.19).To explore the interactions of dialysis with cardiac biomarkers in their relationship with OS, cardiac troponins T (cTnT) and N terminal-pro-brain natriuretic peptide (NT-pro-BNP) were analyzed with timing of dialysis in a proportional hazard model. Timing of dialysis (p < 0.001), cTnT (p = 0.03) and NT-pro-BNP (p = 0.03) all were associated with OS. Using Receiver Operator Characteristic (ROC) curves, best cut points were chosen for cTnT (0.01 ng/ml) and NT-pro-BNP (1350 pg/ml) for survival. When treated as categorical variables, the proportional hazard model found that only NT-pro-BNP (p = 0.002) and timing of dialysis (p < 0.001) were independent predictors of OS but cTnT had loss its significance (p = 0.07). Using Kaplan Meier method, dialysis was a significant risk factor in patients with low cTnT and both high and low NT-pro-BNP (p < 0.001) but not in patients with elevated cTnT (p = 0.25). Discussion: The timing of acute renal failure strongly affects the OS of AL patients undergoing ASCT. In our study, patients who started dialysis prior to ASCT did not have an inferior OS compared to patients who never needed dialysis. On the other hand, starting dialysis after ASCT significantly shortened OS. The timing of dialysis was an independent predictor of OS even when combined with cardiac biomarkers. NT-pro-BNP appears to be the stronger marker when timing of dialysis is considered in the multivariate analysis.
Patient characteristics
| . | I . | II . | III . | IV . | p-value . |
|---|---|---|---|---|---|
| N | 335 | 11 | 40 | 24 | |
| Age | 57 (25–75) | 56 (31–70) | 58 (36–73) | 58 (42–65) | 0.98 |
| Sex (male %) | 58.2 | 72.7 | 67.5 | 45.8 | 0.28 |
| albumin (g/dl) | 2.8 (0.8–4.4) | 2.8 (1.2–3.8) | 2.1 (0.9–3.7) | 2.0 (1.1–3.9) | <0.001 |
| Alk phos (U/L) | 88 (36–1014) | 114 (61–675) | 92.5 (28–1395) | 100 (48–646) | 0.31 |
| Scr (mg/dl) | 1.0 (0.4–2.6) | 6.6 (1.6–12) | 1.3 (0.8–5.6) | 1.2 (0.7–2.2) | <0.001 |
| CrCl (ml/min/1.73m2) | 74 (12–148) | 7 (0–71) | 58 (8–108) | 67 (28–104) | <0.001 |
| Proteinuria (g/d) | 3.0 (0.01–21.4) | 9.8 (0.6–35.4) | 6.6 (0.1–26.2) | 6.5 (0.0–18.5) | <0.001 |
| cTnT (ng/ml) | 0.01 (0.0–1.0) | 0.06 (0.01–0.2) | 0.02 (0.01–0.4) | 0.01 (0.01–0.1) | <0.001 |
| NTproBNP (pg/ml) | 520 (17.5–17330) | 8467 (1089–35000) | 1537 (50.3–8008) | 1079 (40.6–4085) | 0.002 |
| B2m (mcg/ml) | 2.5 (1.0–10.1) | 23.9 (3.5–35.–1) | 3.2 (1.0–15.2) | 2.5 (1.0–5.7) | <0.001 |
| CRP (mg/L) | 0.4 (0.01–40.4) | 1.4 (0.2–9.5) | 0.4 (0.03–13.1) | 0.3 (0.05–5.9) | 0.14 |
| Time to Dialysis | –170 (–700–7) | 14 (4–30) | 866 (36–3106) |
| . | I . | II . | III . | IV . | p-value . |
|---|---|---|---|---|---|
| N | 335 | 11 | 40 | 24 | |
| Age | 57 (25–75) | 56 (31–70) | 58 (36–73) | 58 (42–65) | 0.98 |
| Sex (male %) | 58.2 | 72.7 | 67.5 | 45.8 | 0.28 |
| albumin (g/dl) | 2.8 (0.8–4.4) | 2.8 (1.2–3.8) | 2.1 (0.9–3.7) | 2.0 (1.1–3.9) | <0.001 |
| Alk phos (U/L) | 88 (36–1014) | 114 (61–675) | 92.5 (28–1395) | 100 (48–646) | 0.31 |
| Scr (mg/dl) | 1.0 (0.4–2.6) | 6.6 (1.6–12) | 1.3 (0.8–5.6) | 1.2 (0.7–2.2) | <0.001 |
| CrCl (ml/min/1.73m2) | 74 (12–148) | 7 (0–71) | 58 (8–108) | 67 (28–104) | <0.001 |
| Proteinuria (g/d) | 3.0 (0.01–21.4) | 9.8 (0.6–35.4) | 6.6 (0.1–26.2) | 6.5 (0.0–18.5) | <0.001 |
| cTnT (ng/ml) | 0.01 (0.0–1.0) | 0.06 (0.01–0.2) | 0.02 (0.01–0.4) | 0.01 (0.01–0.1) | <0.001 |
| NTproBNP (pg/ml) | 520 (17.5–17330) | 8467 (1089–35000) | 1537 (50.3–8008) | 1079 (40.6–4085) | 0.002 |
| B2m (mcg/ml) | 2.5 (1.0–10.1) | 23.9 (3.5–35.–1) | 3.2 (1.0–15.2) | 2.5 (1.0–5.7) | <0.001 |
| CRP (mg/L) | 0.4 (0.01–40.4) | 1.4 (0.2–9.5) | 0.4 (0.03–13.1) | 0.3 (0.05–5.9) | 0.14 |
| Time to Dialysis | –170 (–700–7) | 14 (4–30) | 866 (36–3106) |
Overall survival (OS) from the time of autologous stem cell transplant (ASCT). Group I represents patients who never received dialysis. Patients in group II received dialysis prior to ASCT. Group III started dialysis within 30 days of ASCT and group IV started dialysis after 30 days. Significant differences in OS were noted in group III (p = 0.003) and IV (p = 0.004) when compared to Group I.
Overall survival (OS) from the time of autologous stem cell transplant (ASCT). Group I represents patients who never received dialysis. Patients in group II received dialysis prior to ASCT. Group III started dialysis within 30 days of ASCT and group IV started dialysis after 30 days. Significant differences in OS were noted in group III (p = 0.003) and IV (p = 0.004) when compared to Group I.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal