Abstract
Emerging evidence demonstrates that proangiogenic cells (PACs) originate from the BM and are capable of being recruited to sites of ischemic injury where they contribute to neovascularization. We previously determined that among hematopoietic progenitor stem cells, common myeloid progenitors (CMPs) and granulocyte-macrophage progenitor cells (GMPs) differentiate into PACs and possess robust angiogenic activity under ischemic conditions. Herein, we report that a TGF-β1–responsive Krüppel- like factor, KLF10, is strongly expressed in PACs derived from CMPs and GMPs, ∼ 60-fold higher than in progenitors lacking PAC markers. KLF10−/− mice present with marked defects in PAC differentiation, function, TGF-β responsiveness, and impaired blood flow recovery after hindlimb ischemia, an effect rescued by wild-type PACs, but not KLF10−/− PACs. Overexpression studies revealed that KLF10 could rescue PAC formation from TGF-β1+/− CMPs and GMPs. Mechanistically, KLF10 targets the VEGFR2 promoter in PACs which may underlie the observed effects. These findings may be clinically relevant because KLF10 expression was also found to be significantly reduced in PACs from patients with peripheral artery disease. Collectively, these observations identify TGF-β1 signaling and KLF10 as key regulators of functional PACs derived from CMPs and GMPs and may provide a therapeutic target during cardiovascular ischemic states.
Introduction
Accumulating evidence suggests that in healthy persons, circulating endothelial progenitor cells, broadly defined as proangiogenic cells (PACs), represent a population of BM-derived stem and progenitor cells responsible for repairing injured tissue and initiating neovasculogenesis.1,2 Potentiation of PAC mobilization, homing, or adhesion has been shown to ameliorate the development of ischemic injury in animal models.1,2 In addition, blockade of proangiogenic cytokines or their signaling pathways is believed to alter PAC function and to lead to impaired angiogenesis in response to vascular injury and in end-organ ischemia.1,2 Indeed, reduced levels of circulating PACs and diminished PAC function have been reported and found to correlate with a wide spectrum of atherosclerotic vascular diseases, including peripheral artery disease (PAD).3-5
Several early phase 1/2 trials have been conducted to assess the efficacy of cell-based therapies to treat patients with PAD but have yielded mixed results.1,2,6-9 Identification of specific PAC subtypes that are endowed with superior capacity to promote neovascularization may represent a particularly efficacious therapeutic strategy. We have demonstrated that among hematopoietic progenitor stem cells, the common myeloid progenitors (CMPs) and granulocyte-macrophage progenitors (GMPs) constitute a population of BM-derived cells that preferentially differentiate into PACs and possess robust angiogenic activity under ischemic conditions in vivo.10 However, the signaling pathways and downstream factors that mediate these proangiogenic functions remain poorly understood.
The pleiotropic TGF-β1 plays an important role in cell growth, differentiation, and activation in a number cell types.11 TGF-β1 has been shown to contribute to various aspects of neovascularization, including cell adhesion, migration, and homing. These effects may be mediated in part by induction of integrins, chemokine receptors, or responsiveness to important growth factors for cell homing such as stromal cell-derived factor-1 (SDF-1).12-15 Thus, controlled modulation of TGF-β1 and its downstream signaling pathways may allow for fine-tuning of the angiogenic response, perhaps through mechanisms related to PAC differentiation or function.
Krüppel-like factors (KLFs), a subclass of the zinc-finger family of transcription factors, participate in various aspects of cellular growth, development, and differentiation.16,17 KLFs are characterized by a DNA-binding domain that contains 3 C2H2-type zinc fingers capable of binding to either a CACCC-element or GC-box in the promoter region of target genes, thereby regulating transcriptional activity and gene expression. Gene-targeting studies have implicated KLFs as important in immune and hematopoietic cell biology.16,17 Because of the critical role played by KLFs in the development of different hematopoietic lineages, we hypothesized that a related Krüppel-like zinc-finger protein may regulate the differentiation or function of CMP- or GMP-derived PACs.
Our studies provide evidence that, in response to TGF-β1, KLF10 plays an important role in controlling CMP- and GMP-derived PAC differentiation and function in vitro and in vivo. Notably, KLF10−/− CMP- and GMP-derived PACs possess multiple defects in effector functions, including adhesion, migration, and elaboration or expression of chemokines, chemokine receptors, and integrins critical to neovascularization. In addition, KLF10−/− mice display reduced levels of circulating PACs and impaired blood flow recovery after hindlimb ischemia, an effect rescued by wild-type (WT) PACs but not by KLF10−/− PACs. Mechanistically, KLF10 targets VEGFR2, which may explain, in part, these effects. Importantly, KLF10 expression was found to be reduced in PACs from patients with PAD. Taken together, these observations indicate that KLF10 acts as a key transcriptional regulator of TGF-β1 in PAC differentiation and function and may represent a potential target for therapeutic intervention to regulate angiogenesis.
Methods
Mice
KLF10−/− mice were generated in T.C.S.'s laboratory (Mayo Clinic),18 and TGF-β1+/−/Rag2−/− mice were obtained from the National Cancer Institute Mouse Repository. Mouse genotypes were verified by PCR. Mice aged 8-12 weeks were used for most experiments.
Isolation and in vitro differentiation of PACs
CMPs, GMPs, megakaryocyte-erythrocyte progenitors (MEPs), and hematopoietic stem cells (HSCs) were isolated from C57BL/6 mice and KLF10−/− mice BM with the use of multicolor FACS (BD ARIAFACS; BD Biosciences) as previously described.19 Single-cell suspensions were prepared from BM, and red cells were lysed with red cell lysis solution (QIAGEN).
In vivo subcutaneous Matrigel plug
The subcutaneous Matrigel plug mouse model was generated from 8- to 10-week-old male WT or KLF10−/− mice. Matrigel plugs that had been admixed with 0.8 mL of Matrigel (BD Biosciences), basic fibroblast growth factor (250 ng/mL; R&D Systems), and heparin (60 U/mL; Hospira Inc) were implanted subcutaneously. After 8 days, Matrigel plugs were removed, embedded in paraffin, and sectioned for detection of angiogenesis using an anti–mouse CD31 antibody (eBioscience).
Hindlimb ischemia
Ischemic injury was produced by unilateral femoral artery ligation in C57BL/6 mice. The right femoral artery was isolated under direct visualization. Proximal and distal sutures were tied around the femoral artery relative to the origin of the deep femoral artery. The deep femoral artery was cauterized, and the complete severance of the main femoral artery was performed between the 2 ligatures. Immediately after surgery, mice were imaged on a 785-nm near-infrared Laser Doppler Imager-2 (Moor Instruments Inc). In some studies, the relevant BM-derived PACs from WT or KLF10−/− mice were injected intramuscularly into KLF10−/− or WT mice into the right quadriceps immediately after surgery.
Statistical analysis
Values are expressed as mean ± SD. Differences between values were examined with the Student t test (2-tailed) and were considered significant at P < .05.
Additional detailed information can be found in supplemental Methods (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Results
TGF-β1 modulation of PAC differentiation and function
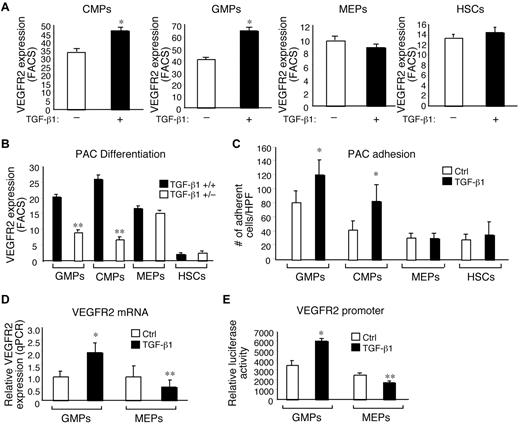
Our previous observations suggested that CMPs and GMPs, as opposed to MEPs, HSCs, or common lymphoid progenitors. preferentially differentiated into PACs and exhibited high angiogenic activity in vivo.10 Signals emanating from TGF-β and IFN-γ are known to antagonize normal cell growth and differentiation events and have been implicated in regulating different aspects of angiogenesis.20-22 To assess the effect of TGF-β1 signaling on PAC differentiation, BM progenitor-derived PACs were cultured for 7 days in the presence or absence of recombinant TGF-β1; modulation of the PAC marker VEGFR2 was then examined. As shown in Figure 1A, treatment of CMP- and GMP-derived progenitors with TGF-β1 resulted in enhanced PAC differentiation by ∼ 28% and ∼ 35%, respectively, as measured by VEGFR2 cell surface expression. To examine the role of IFN-γ on PAC differentiation, BM-derived progenitors were treated in the presence or absence of recombinant IFN-γ in an analogous manner. PAC differentiation was markedly impaired from CMP- and GMP-derived progenitors in the presence of IFN-γ (∼ 31% and 74%, respectively; supplemental Figure 1). To further verify the role of TGF-β1 on PAC formation, we isolated BM progenitors from TGF-β1 heterozygous/Rag2 knockout mice and assessed their ability to differentiate into PACs. As shown in Figure 1B, CMP- and GMP-derived progenitors exhibited marked defects (∼ 73% and 60%, respectively) in their ability to differentiate into PACs, whereas the MEPs from these mice were only minimally impaired. Furthermore, we explored the effect of TGF-β1 on PAC adhesion capacity of the various BM-derived progenitors. Progenitors were cultured in the presence or absence of TGF-β1 and examined for their ability to adhere to fibronectin-coated plates. Although TGF-β1 was able to promote CMP- and GMP-derived PAC adherence, no effect of TGF-β1 on MEPs or HSCs was observed (Figure 1C). Collectively, these observations showed that PAC differentiation from BM-derived progenitors can be regulated in response to antagonistic signaling pathways. Furthermore, these findings suggested that TGF-β1 signaling may be critically involved in the generation of the proangiogenic CMP- and GMP-derived PACs.
TGF-β1 regulates PAC differentiation and function. (A) VEGFR2 expression in BM-derived progenitors isolated from WT mice (A) or TGF-β1+/+ or TGF-β1+/− mice (B) and grown in the presence or absence of TGF-β1 (A) for 7 days (n = 3 per group). Percentage of VEGFR2 expression was analyzed by flow cytometry. *P < .01 versus no TGF-β1; **P < .01 versus TGF-β1+/−. (C) BM-derived progenitors grown in the presence of Ctrl (vehicle) or TGF-β1 and plated in fibronectin-coated wells were assessed for adhesion (n = 6 per group). HPF indicates high power field. *P < .05 versus Ctrl. (D) BM-derived GMPs and MEPs were grown in the presence or absence of TGF-β1 treatment were assessed for VEGFR2 mRNA expression by quantitative PCR (n = 3 per group). *P < .01 versus Ctrl; **P < .05 versus Ctrl. (E) TGF-β1–stimulated expression of the VEGFR2 promoter-luciferase reporter transfected in BM-derived GMPs and MEPs (n = 3 per group). *P < .01 versus Ctrl; **P < .05 versus Ctrl.
TGF-β1 regulates PAC differentiation and function. (A) VEGFR2 expression in BM-derived progenitors isolated from WT mice (A) or TGF-β1+/+ or TGF-β1+/− mice (B) and grown in the presence or absence of TGF-β1 (A) for 7 days (n = 3 per group). Percentage of VEGFR2 expression was analyzed by flow cytometry. *P < .01 versus no TGF-β1; **P < .01 versus TGF-β1+/−. (C) BM-derived progenitors grown in the presence of Ctrl (vehicle) or TGF-β1 and plated in fibronectin-coated wells were assessed for adhesion (n = 6 per group). HPF indicates high power field. *P < .05 versus Ctrl. (D) BM-derived GMPs and MEPs were grown in the presence or absence of TGF-β1 treatment were assessed for VEGFR2 mRNA expression by quantitative PCR (n = 3 per group). *P < .01 versus Ctrl; **P < .05 versus Ctrl. (E) TGF-β1–stimulated expression of the VEGFR2 promoter-luciferase reporter transfected in BM-derived GMPs and MEPs (n = 3 per group). *P < .01 versus Ctrl; **P < .05 versus Ctrl.
We next assessed whether TGF-β1 was able to effectively promote PAC differentiation through regulation of VEGFR2 gene expression by investigating the transcript levels and promoter activity. As shown in Figure 1D, exposure to TGF-β1 led to a ∼ 2-fold increase in VEGFR2 mRNA expression in GMP-derived PACs, whereas there was no effect detectable in MEP-derived PACs. To assess whether TGF-β1 could directly mediate the activity of the VEGFR2 promoter, we performed transient transfection reporter studies in BM progenitor-derived PACs. As shown in Figure 1E, TGF-β1 treatment of GMP-derived PACs led to increased (∼ 43%) VEGFR2 promoter activity. In contrast, VEGFR2 promoter activity was reduced by ∼ 28% in MEP-derived PACs. Taken together, these findings suggested that TGF-β1 may promote PAC differentiation from GMP-derived PACs, in part, by increasing VEGFR2 gene expression.
KLF10 expression and TGF-β1 responsiveness in PACs
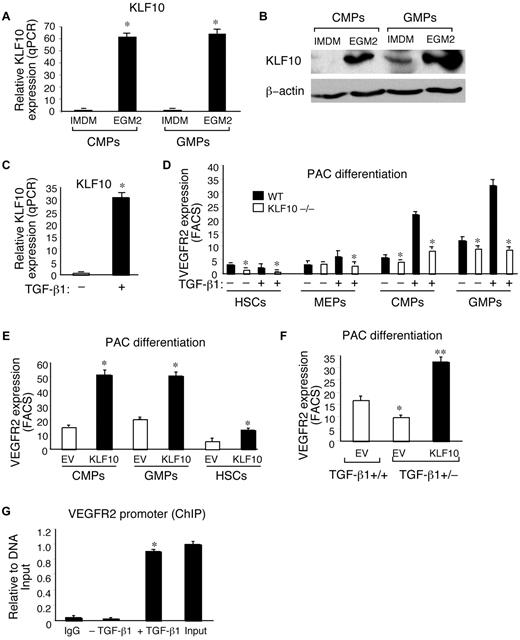
Taking into consideration the acknowledged role for KLFs in other hematopoietic cell types, we hypothesized that members of this family may also play a role in PAC biology. With the use of real-time PCR, we screened expression levels of known KLFs (KLF1-17) in freshly isolated CMPs and GMPs and PACs grown in culture from either CMPs or GMPs. We found that only 1 KLF member, KLF10, was robustly expressed (∼ 60-fold) in fully differentiated PACs at both the mRNA and protein level compared with CMPs or GMPs grown in hematopoietic IMDM medium (Figure 2A-B). In contrast, all the other KLFs were found to be minimally expressed, reduced, or unchanged (data not shown). Recent studies by others have shown that KLF10, also known as the transforming growth factor-inducible early gene-1 (TIEG1), is a TGF-β1–responsive factor in several cell types.23 As shown in Figure 2C, TGF-β1 treatment potently increased KLF10 expression in GMP-derived PACs (∼ 32-fold). Importantly, KLF10−/− BM GMP and CMP progenitors were significantly impaired in their ability to differentiate into PACs at baseline (∼ 21% and ∼ 6%, respectively) and exhibited a near complete absence of TGF-β1 responsiveness as measured by VEGFR2 cell surface expression (Figure 2D). In addition, the defect of differentiation in KLF10−/− PACs was not accompanied by an increase of apoptosis or senescence (supplemental Figure 2A-B). To assess the ability of KLF10 to promote PAC differentiation, we performed overexpression studies with the use of a retrovirus transduction system. VEGFR2 cell surface expression was increased by > 3-fold in CMPs and GMPs overexpressing KLF10 (Figure 2E). In addition, VEGFR2 expression was also induced by ∼ 2-fold in KLF10-overexpressing HSCs (Figure 2E), which possess lower angiogenic properties than CMPs and GMPs.10 To assess whether the defect in PAC differentiation from TGF-β1+/− GMPs could be rescued by exogenous KLF10, GFP-EV (Ctrl), or KLF10 (GFP-RV-KLF10) was transduced in TGF-β1+/+ or TGF-β1+/− GMPs, and VEGFR2 expression was measured by FACS. As shown in Figure 2F, KLF10-overexpressing cells were capable of rescuing VEGFR2 expression in TGF-β1+/− GMPs to levels even higher than that achieved in TGF-β1+/+ GMPs transduced with EV Ctrl. Finally, to determine whether KLF10 was capable of binding to the VEGFR2 promoter, we performed ChIP studies. As shown in Figure 2G, in response to TGF-β1 treatment, KLF10 bound to a region within the VEGFR2 promoter in which a consensus CACCC KLF site was located. Collectively, these observations suggested that, in response to TGF-β1, KLF10 may be a key downstream transcriptional regulator of PAC differentiation and function.
Identification of KLF10 expression in PACs and responsiveness to TGF-β1. (A-B) BM-derived progenitors grown in either hematopoietic IMDM medium or EGM-2 were harvested, and expression of Klf10 was examined by quantitative PCR (A) or Western blot analysis (B). *P < .01. β-actin was used as an internal loading control. (C-D) BM-derived progenitors grown in EGM-2 medium in the presence or absence of TGF-β1. Klf10 mRNA expression was examined in GMP-derived PACs by quantitative PCR (C). *P < .01 versus no TGF-β1. (D) VEGFR2 expression was examined by flow cytometry for the indicated WT or KLF10−/− PACs (n = 3 per group); *P < .01 versus WT. (E-F) BM-derived progenitors were transduced with retrovirus GFP-RV-EV (empty vector; ctrl) or GFP-RV-KLF10. The percentage of GFP+ cells that also expressed VEGFR2 in WT CMP-, GMP-, and HSC-derived PACs (E) or TGF-β1+/+ and TGF-β1+/− CMP-derived PACs (F) was assessed by FACS. *P < .01 versus empty EV; **P < .05 versus EV TGF-β1+/+. (G) ChIP analysis of KLF10 binding to the VEGFR2 promoter in GMP-derived PACs. IgG was used as a nonspecific control. Assays were performed in triplicate by real-time quantitative PCR with the use of primers at −294 bp and −30 bp of the VEGFR2 promoter. Values are presented as relative to DNA input. *P < .01 versus without TGF-β1 treatment.
Identification of KLF10 expression in PACs and responsiveness to TGF-β1. (A-B) BM-derived progenitors grown in either hematopoietic IMDM medium or EGM-2 were harvested, and expression of Klf10 was examined by quantitative PCR (A) or Western blot analysis (B). *P < .01. β-actin was used as an internal loading control. (C-D) BM-derived progenitors grown in EGM-2 medium in the presence or absence of TGF-β1. Klf10 mRNA expression was examined in GMP-derived PACs by quantitative PCR (C). *P < .01 versus no TGF-β1. (D) VEGFR2 expression was examined by flow cytometry for the indicated WT or KLF10−/− PACs (n = 3 per group); *P < .01 versus WT. (E-F) BM-derived progenitors were transduced with retrovirus GFP-RV-EV (empty vector; ctrl) or GFP-RV-KLF10. The percentage of GFP+ cells that also expressed VEGFR2 in WT CMP-, GMP-, and HSC-derived PACs (E) or TGF-β1+/+ and TGF-β1+/− CMP-derived PACs (F) was assessed by FACS. *P < .01 versus empty EV; **P < .05 versus EV TGF-β1+/+. (G) ChIP analysis of KLF10 binding to the VEGFR2 promoter in GMP-derived PACs. IgG was used as a nonspecific control. Assays were performed in triplicate by real-time quantitative PCR with the use of primers at −294 bp and −30 bp of the VEGFR2 promoter. Values are presented as relative to DNA input. *P < .01 versus without TGF-β1 treatment.
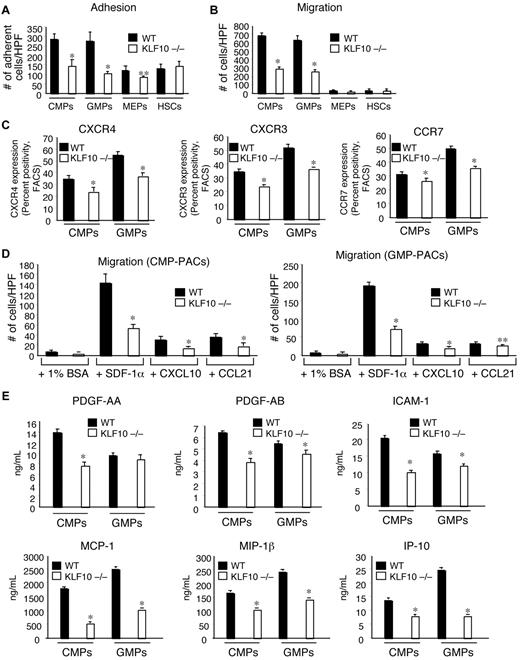
KLF10−/− PACs possess markedly reduced migratory function and release of soluble paracrine factors
To explore whether KLF10 deficiency was associated with impaired PAC functional responses, we performed a series of studies and measured effects on cell adhesion, migration, endothelial “wound healing,” as well as the elaboration or expression of cytokines, chemokines, and chemokine receptors. To assess whether KLF10−/− PACs have impaired adhesive properties in vitro, we plated equal numbers of BM progenitor–derived PACs from WT or KLF10−/− mice onto fibronectin-coated plates. As shown in Figure 3A, KLF10−/− PACs derived from CMPs and GMPs exhibited reduced adherence (by ∼ 48% and ∼ 60%, respectively), compared with WT CMP- and GMP-derived PACs. In contrast, KLF10−/− PACs derived from HSCs presented no significant differences in adhesion, whereas KLF10−/− MEP-derived PACs showed a more modest reduction (∼ 26%) than WT MEP-derived PACs. To examine the relative contribution of integrin-mediated effects in this assay, we incubated WT HSC-, MEP-, CMP-, and GMP-derived PACs in the presence or absence of integrin-blocking antibodies. As shown in supplemental Figure 4, blocking antibodies to either β1 or β2 integrins had modest effects (∼ 13%-28%) at inhibiting the adherence of WT CMP- or GMP-derived PACs to fibronectin-coated plates. These data suggest that integrin-mediated events play a minor role in CMP- or GMP-derived PAC adhesion.
KLF10−/− CMP- and GMP-derived PACs possess markedly reduced migratory function and release of soluble paracrine factors. (A) The indicated WT or KLF10−/− BM-derived PACs were assayed for adhesion on fibronectin-coated plates. The number of adherent cells was quantitated after 15 minutes (n = 6 per group). *P < .01 versus WT; **P < .05 versus WT. (B) The indicated WT or KLF10−/− BM-derived PACs were assayed using a modified Transwell Boyden chamber in response to serum. The number of cells in the lower chamber was quantitated after 4 hours (n = 6 per group). *P < .01 versus WT. (C) Cell surface expression of the chemokine receptors CXCR4, CXCR3, and CCR7 was determined on the indicated WT or KLF10−/− BM-derived PACs by flow cytometry and expressed as percentage of positivity. (D) The indicated WT or KLF10−/− BM-derived PACs were assayed with a modified Transwell Boyden chamber in response to 1% BSA control or the chemokines SDF-1α, CXCL10, or CCL21. The number of cells in the lower chamber was quantitated after 4 hours (n = 6 per group). *P < .01 versus WT; **P < .05 versus WT. (E) Culture supernatants were harvested from the indicated WT or KLF10−/− CMP- and GMP-derived PACs assessed by ELISA for the indicated cytokines, growth factors, or chemokines (n = 3 per group). *P < .01 versus WT.
KLF10−/− CMP- and GMP-derived PACs possess markedly reduced migratory function and release of soluble paracrine factors. (A) The indicated WT or KLF10−/− BM-derived PACs were assayed for adhesion on fibronectin-coated plates. The number of adherent cells was quantitated after 15 minutes (n = 6 per group). *P < .01 versus WT; **P < .05 versus WT. (B) The indicated WT or KLF10−/− BM-derived PACs were assayed using a modified Transwell Boyden chamber in response to serum. The number of cells in the lower chamber was quantitated after 4 hours (n = 6 per group). *P < .01 versus WT. (C) Cell surface expression of the chemokine receptors CXCR4, CXCR3, and CCR7 was determined on the indicated WT or KLF10−/− BM-derived PACs by flow cytometry and expressed as percentage of positivity. (D) The indicated WT or KLF10−/− BM-derived PACs were assayed with a modified Transwell Boyden chamber in response to 1% BSA control or the chemokines SDF-1α, CXCL10, or CCL21. The number of cells in the lower chamber was quantitated after 4 hours (n = 6 per group). *P < .01 versus WT; **P < .05 versus WT. (E) Culture supernatants were harvested from the indicated WT or KLF10−/− CMP- and GMP-derived PACs assessed by ELISA for the indicated cytokines, growth factors, or chemokines (n = 3 per group). *P < .01 versus WT.
PACs promote angiogenesis in response to injury through several mechanisms, including adhesion and subsequent transmigration. To explore migratory function in detail, various PACs were placed in the top of a Transwell Boyden chamber and were assessed for their ability to translocate to the lower chamber in response to serum (Figure 3B) or to chemokines implicated in neovascularization (Figure 3D). The KLF10−/− PACs derived from CMPs and GMPs were markedly impaired in their ability to transmigrate in response to serum (Figure 3B); these cells migrated ∼ 57% and ∼ 58% less than their respective WT PACs (Figure 3B). In contrast, those KLF10−/− PACs derived from MEPs and HSCs showed no differences in their ability to transmigrate compared with their WT PAC counterparts. We next examined if the expression of chemokine receptors implicated in neovascularization may be reduced in KLF10−/− CMP- and GMP-derived PACs. Indeed, compared with WT CMP- and GMP-derived PACs, KLF10−/− PACs exhibited reduced cell surface expression of the chemokine receptors CXCR4, CXCR3, and CCR7 (Figure 3C). We further assessed the relative ability of CMP- and GMP-derived PACs to migrate in response to the chemokines SDF-1α (ligand for CXCR4), CXCL10 (ligand for CXCR3), and CCL21 (ligand for CCR7). As shown in Figure 3D, migration was significantly reduced by > 60% in response to the chemokine SDF-1α for both KLF10−/− CMP- and GMP-derived proangiogenic cells compared with their WT counterparts. Furthermore, among WT CMP- and GMP-derived PACs, SDF-1α produced a more potent migratory response (19- and 23-fold higher than with BSA controls) compared with the chemokines CXCL10 and CCL21 (∼ 4-fold). Finally, migration was reduced more modestly in response to the chemokines CXCL10 and CCL21 in KLF10−/− proangiogenic cells, an effect underscoring that the SDF-1α/CXCR4 axis is one of the dominant migratory defects exhibited by KLF10−/− CMP- and GMP-derived proangiogenic cells.
PACs can elaborate a variety of proangiogenic cytokines, growth factors, and chemokines. To assess the ability of KLF10−/− PACs to elaborate such factors, we first performed the classic in vitro endothelial “scratch wound assay” with the use of the conditioned medium from WT and KLF10−/− PACs. The ability of HUVECs to “close” over the wound within 24 hours showed that conditioned medium harvested from KLF10−/− PACs derived from CMPs and GMPs was impaired in its ability to promote wound healing by ∼ 57% and ∼ 26%, respectively, compared with WT PACs (supplemental Figure 2A-B); in contrast, no differences were observed between conditioned medium collected from WT or KLF10−/− for either MEP- or HSC-derived PACs. Finally, to explore which factors normally secreted from CMP- or GMP-derived PACs may be reduced as a result of KLF10 deficiency, the conditioned medium was analyzed by ELISA. As shown in Figure 3E, KLF10−/− PACs were unable to elaborate many of the growth factors, cytokines, and chemokines investigated. In particular, conditioned medium from CMP-derived KLF10−/− PACs was found to have strikingly reduced levels of PDGF-AA and PDGF-AB (∼ 39% and ∼ 44%, respectively), compared with WT CMP-derived PACs. In contrast, PDGF-AB secreted from GMP-derived KLF10−/− PACs was reduced to a lesser extent (∼ 18%), and PDGF-AA secretion was only slightly different from WT. Other factors such as ICAM-1 and the chemokines MCP-1, MIP-1β, and IFN-γ–inducible protein (IP-10) were potently reduced in both CMP- and GMP-derived KLF10−/− PACs, compared with their WT counterparts (Figure 3E). Collectively, these findings indicated that KLF10−/− CMP- and GMP-derived PACs possess major functional defects in their ability to migrate, specifically in response to SDF-1α, and in their ability to release several soluble paracrine factors implicated in promoting angiogenesis.
KLF10−/− mice develop markedly impaired blood flow recovery associated with reduced levels of peripheral blood PACs and neovascularization in response to hindlimb ischemia
To examine whether the impaired differentiation responses in KLF10−/− PACs in vitro correlated to defects in an in vivo mouse model of neovascularization, we performed hindlimb ischemia studies by femoral artery ligation. Approximately 7-14 days after femoral artery ligation, KLF10−/− mice developed either autoamputation of the ischemic leg (n = 2 of 21 KLF10−/− mice vs 0 of 21 WT mice; Figure 4A) or severely impaired blood flow recovery responses as measured by laser Doppler imaging (Figure 4B). Quantitation performed at days 14, 21, and 28 after ligature surgery showed significantly reduced blood flow recovery (23%, 24%, and 12%, respectively) in KLF10−/− mice compared with WT mice. Measurement of peripheral blood PACs at day 7 after ligation surgery showed that KLF10−/− mice had significantly decreased amounts of mobilized peripheral blood PACs, ∼ 38% lower than WT mice (Figure 4C). To assess the relative contribution of WT and KLF10−/− PACs in their ability to rescue the defect in blood flow recovery in KLF10−/− mice, intramuscular injections were performed at the time of femoral artery ligation. Although WT PACs (derived from equal portions of CMPs and GMPs) were able to completely rescue blood flow recovery in KLF10−/− mice, KLF10−/− PACs (also derived equally from CMPs and GMPs) had no effect (Figure 4D). Furthermore, immunofluorescence staining for CD31 indicated markedly reduced neovascularization in quadriceps muscles after intramuscular injections with KLF10−/− PACs, opposed to that seen in quadriceps muscles injected with WT PACs (Figure 4E). Quadriceps muscles injected with KLF10−/− PACs also showed higher caspase-3 levels when evaluated by immunostaining, suggesting that KLF10−/− PACs may not be able to protect against injury-induced apoptosis (supplemental Figure 5). Finally, despite that the WT PACs were capable of incorporating into capillary structures, albeit at extremely low frequencies, we could not find any evidence of similar incorporation by the KLF10−/− PACs (Figure 4F). Taken together, these observations highlight that KLF10−/− mice have markedly reduced blood flow recovery, an effect that can be rescued by WT PACs but not KLF10−/− PACs.
Effect of KLF10 deficiency on hindlimb ischemia. (A-E) WT or KLF10−/− mice underwent femoral artery ligation to induce hindlimb ischemia. (A) KLF10−/− mice (n = 2 of 21) developed autoamputation of the ischemic leg. Mice were photographed with a Nikon Coolpix 4600 digital camera. (B) Images (left) are representative of blood flow recovery for each time point over 28 days. Quantitation (right) of blood flow recovery was calculated as the mean blood flow (right [ischemic] leg)/left [(nonischemic] leg) by laser Doppler imaging (785-nm near-infrared Laser Doppler Imager-2; Moor Instruments).*P < .01 versus WT; **P < .05 versus WT. (C) FACS analyses of circulating PACs (Sca-1+/VEGFR2+) in WT or KLF10−/− mice 7 days after femoral artery ligation (n = 9-10 per group). *P < .05 versus WT. (D) WT or KLF10−/− PACs (1:1 mix of CMP- and GMP-derived PACs) were intramuscularly injected immediately after femoral artery ligation in KLF10−/− mice. Mean blood flow recovery (ischemic leg/nonischemic leg) was measured by laser Doppler imaging after 3 days. *P < .05 versus WT +PBS. (E-F) Frozen sections of quadriceps muscles harvested 3 days after intramuscular injection of WT or KLF10−/− PACs were labeled with cell tracker (red) and a FITC-conjugated mAb to CD31 (green). (E) Sections were analyzed for CD31 staining with the use of an AQUA/PM2000 Imaging Platform (HistoRx), and automated quantitative analysis was performed with Software suite Version 2.2 (HistoRx). *P < .01 versus WT; n = 4 mice per group. (F) Sections were examined with an Olympus, Fluoview, Model FV1000 camera at 10× magnification and FV10-ASW Version 02.01 software to determine the percentage of labeled PACs (red) that colocalized (yellow) with CD31+ cells (green). *P < .01 versus WT; n = 4 mice per group.
Effect of KLF10 deficiency on hindlimb ischemia. (A-E) WT or KLF10−/− mice underwent femoral artery ligation to induce hindlimb ischemia. (A) KLF10−/− mice (n = 2 of 21) developed autoamputation of the ischemic leg. Mice were photographed with a Nikon Coolpix 4600 digital camera. (B) Images (left) are representative of blood flow recovery for each time point over 28 days. Quantitation (right) of blood flow recovery was calculated as the mean blood flow (right [ischemic] leg)/left [(nonischemic] leg) by laser Doppler imaging (785-nm near-infrared Laser Doppler Imager-2; Moor Instruments).*P < .01 versus WT; **P < .05 versus WT. (C) FACS analyses of circulating PACs (Sca-1+/VEGFR2+) in WT or KLF10−/− mice 7 days after femoral artery ligation (n = 9-10 per group). *P < .05 versus WT. (D) WT or KLF10−/− PACs (1:1 mix of CMP- and GMP-derived PACs) were intramuscularly injected immediately after femoral artery ligation in KLF10−/− mice. Mean blood flow recovery (ischemic leg/nonischemic leg) was measured by laser Doppler imaging after 3 days. *P < .05 versus WT +PBS. (E-F) Frozen sections of quadriceps muscles harvested 3 days after intramuscular injection of WT or KLF10−/− PACs were labeled with cell tracker (red) and a FITC-conjugated mAb to CD31 (green). (E) Sections were analyzed for CD31 staining with the use of an AQUA/PM2000 Imaging Platform (HistoRx), and automated quantitative analysis was performed with Software suite Version 2.2 (HistoRx). *P < .01 versus WT; n = 4 mice per group. (F) Sections were examined with an Olympus, Fluoview, Model FV1000 camera at 10× magnification and FV10-ASW Version 02.01 software to determine the percentage of labeled PACs (red) that colocalized (yellow) with CD31+ cells (green). *P < .01 versus WT; n = 4 mice per group.
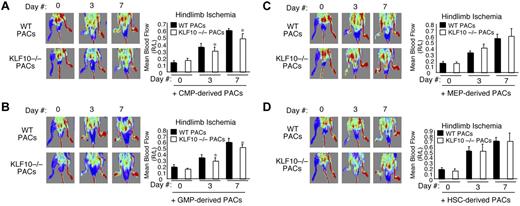
To verify the effects on blood flow recovery between individual WT and KLF10−/− BM-derived PAC subsets in WT mice, intramuscular injections were performed in an analogous manner at the time of femoral artery ligation. As shown in Figure 5, KLF10−/− CMP- and GMP-derived PACs had reduced ability to rescue blood flow recovery in WT mice compared with WT CMP- and GMP-derived PACs (Figure 5A and B, respectively). In contrast, there were no reductions in blood flow recovery observed after intramuscular injections of KLF10−/− MEP- or HSC-derived PACs compared with WT MEP- or HSC-derived PACs (Figure 5C and D, respectively). Thus, KLF10-deficient CMP- and GMP-derived PACs exhibit significant defects in promoting blood flow recovery in WT mice. These findings further underscore the inability of KLF10−/− CMP- and GMP-derived PACs to promote neovascularization either directly by incorporation into capillaries or indirectly by paracrine-mediated effects.
Effect of KLF10−/−PACs on blood flow recovery in WT mice. (A-D) WT mice underwent femoral artery ligation to induce hindlimb ischemia. WT or KLF10−/− CMP-, GMP-, MEP-, or HSC-derived PACs were intramuscularly injected immediately after femoral artery ligation (n = 5 per group). Mean blood flow recovery (ischemic leg/nonischemic leg) was measured by tissue Doppler imaging. *P < .05 versus WT PACs.
Effect of KLF10−/−PACs on blood flow recovery in WT mice. (A-D) WT mice underwent femoral artery ligation to induce hindlimb ischemia. WT or KLF10−/− CMP-, GMP-, MEP-, or HSC-derived PACs were intramuscularly injected immediately after femoral artery ligation (n = 5 per group). Mean blood flow recovery (ischemic leg/nonischemic leg) was measured by tissue Doppler imaging. *P < .05 versus WT PACs.
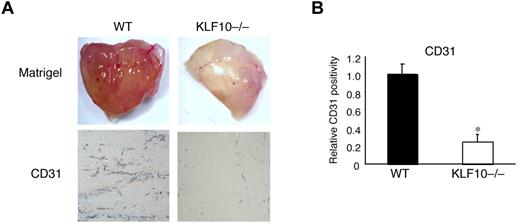
Reduced angiogenesis in Matrigel plugs from KLF10−/− mice
The Matrigel plug assay is a well-established model of angiogenesis in vivo.24 To determine whether KLF10−/− mice develop fewer capillaries than their WT counterparts, we performed Matrigel plug implantation studies. On explantation, Matrigel plugs from KLF10−/− mice were found to be markedly less red (Figure 6A) and to have ∼ 75% less angiogenesis than plugs from WT mice by CD31 staining (Figure 6B). These findings further showed that KLF10−/− mice possess marked in vivo defects in neovascularization.
Reduced angiogenesis in Matrigel plugs implanted in KLF10−/− mice. (A-B) Matrigel plugs subcutaneously implanted for 8 days in WT or KLF10−/− mice (n = 10 per group) were stained for CD31. (A) Angiogenesis in whole Matrigel plugs. Matrigel images were photographed with an Olympus, Model SZ61 camera (top). CD31 staining in paraffin sections (5 μm; bottom) was analyzed with an Olympus, Fluoview, Model FV1000 camera at 10× magnification and FV10-ASW Version 02.01 software and quantitated as relative CD31 positivity (B). *P < .01 versus WT.
Reduced angiogenesis in Matrigel plugs implanted in KLF10−/− mice. (A-B) Matrigel plugs subcutaneously implanted for 8 days in WT or KLF10−/− mice (n = 10 per group) were stained for CD31. (A) Angiogenesis in whole Matrigel plugs. Matrigel images were photographed with an Olympus, Model SZ61 camera (top). CD31 staining in paraffin sections (5 μm; bottom) was analyzed with an Olympus, Fluoview, Model FV1000 camera at 10× magnification and FV10-ASW Version 02.01 software and quantitated as relative CD31 positivity (B). *P < .01 versus WT.
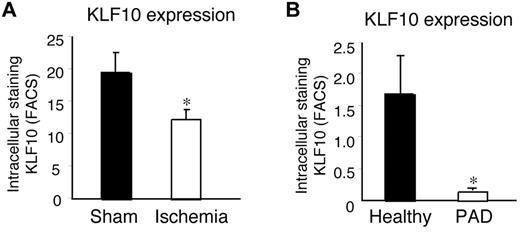
KLF10 expression during hindlimb ischemia in mice and in humans with PAD
Several studies have identified an association with reduced PAC levels or function in patients with ischemic disease states such as PAD.3-5 Because our findings thus far had suggested KLF10 expression as being important for optimal PAC function, we hypothesized that KLF10 expression in circulating PACs would be reduced both in mice with hindlimb ischemia as well as in human patients with PAD. First, we performed femoral artery ligation studies in mice and measured the KLF10 expression in PACs by intracellular staining and FACS. Compared with circulating PACs from sham-operated control mice, KLF10 levels were significantly reduced (by 34%) in PACs from mice with hindlimb ischemia (Figure 7A). Reduced expression of KLF10 was also observed in PACs from patients with PAD (91% lower than healthy controls; Figure 7B). Demographics are shown in Table 1 for healthy subject controls and patients with PAD, including sex, age, and presence of diabetes. Although the patients with PAD exhibited increased age (67.8 ± 8.6 years vs 57.3 ± 7.0 years) compared with the healthy subject control group, there was no correlation of KLF10 expression with increasing age within either group (data not shown). In addition, expression levels of KLF10 were also reduced in patients with disease states known to be associated with PAC dysfunction, including diabetes (reduced by 71%) and stent thrombosis (reduced by 78%; supplemental Figure 6). Taken together, these findings suggest that reduced KLF10 levels in PACs may represent an effective biomarker for the presence of PAD and that TGF-β1/KLF10 signaling may be important for optimal PAC function.
KLF10 expression in response to hindlimb ischemia in mice and in human patients with PAD. (A) Eight- to 10-week-old, male WT mice underwent femoral artery ligation to induce hindlimb ischemia (ischemia) or sham control operation (sham), and expression of Klf10 was determined by intracellular staining of circulating PACs (Sca1+/VEGFR2+) after 7 days by flow cytometry. *P < .01 versus sham. (B) Expression of KLF10 was determined in circulating PACs (CD34+/VEGFR2+) obtained from healthy control subjects or patients with symptomatic PAD. *P < .01 versus healthy controls.
KLF10 expression in response to hindlimb ischemia in mice and in human patients with PAD. (A) Eight- to 10-week-old, male WT mice underwent femoral artery ligation to induce hindlimb ischemia (ischemia) or sham control operation (sham), and expression of Klf10 was determined by intracellular staining of circulating PACs (Sca1+/VEGFR2+) after 7 days by flow cytometry. *P < .01 versus sham. (B) Expression of KLF10 was determined in circulating PACs (CD34+/VEGFR2+) obtained from healthy control subjects or patients with symptomatic PAD. *P < .01 versus healthy controls.
Demographics of healthy subject controls and PAD patients
| Identification no. . | PAD, symptomatic claudication or ABI < 0.9 . | Sex . | Age, y . | Diabetes . |
|---|---|---|---|---|
| Healthy subject controls | ||||
| 1 | No | M | 47 | No |
| 2 | No | M | 49 | No |
| 3 | No | F | 51 | Yes |
| 4 | No | M | 61 | No |
| 5 | No | M | 64 | No |
| 6 | No | F | 64 | No |
| 7 | No | M | 62 | No |
| 8 | No | M | 60 | No |
| Patients with PAD | ||||
| 9 | Yes | M | 68 | Yes |
| 10 | Yes | M | 80 | No |
| 11 | Yes | M | 75 | No |
| 12 | Yes | F | 80 | No |
| 13 | Yes | F | 71 | No |
| 14 | Yes | M | 67 | Yes |
| 15 | Yes | M | 55 | No |
| 16 | Yes | M | 73 | No |
| 17 | Yes | M | 66 | No |
| 18 | Yes | F | 61 | No |
| 19 | Yes | M | 63 | No |
| 20 | Yes | M | 54 | Yes |
| Identification no. . | PAD, symptomatic claudication or ABI < 0.9 . | Sex . | Age, y . | Diabetes . |
|---|---|---|---|---|
| Healthy subject controls | ||||
| 1 | No | M | 47 | No |
| 2 | No | M | 49 | No |
| 3 | No | F | 51 | Yes |
| 4 | No | M | 61 | No |
| 5 | No | M | 64 | No |
| 6 | No | F | 64 | No |
| 7 | No | M | 62 | No |
| 8 | No | M | 60 | No |
| Patients with PAD | ||||
| 9 | Yes | M | 68 | Yes |
| 10 | Yes | M | 80 | No |
| 11 | Yes | M | 75 | No |
| 12 | Yes | F | 80 | No |
| 13 | Yes | F | 71 | No |
| 14 | Yes | M | 67 | Yes |
| 15 | Yes | M | 55 | No |
| 16 | Yes | M | 73 | No |
| 17 | Yes | M | 66 | No |
| 18 | Yes | F | 61 | No |
| 19 | Yes | M | 63 | No |
| 20 | Yes | M | 54 | Yes |
ABI indicates ankle-brachial index.
Discussion
In this study we have provided evidence that KLF10 is able to regulate PAC differentiation and function both in vitro and in vivo. Specifically, KLF10 was found to be a TGF-β1–responsive gene expressed highly in CMP- and GMP-derived PACs. Its activity programmed CMPs and GMPs toward a proangiogenic phenotype, at least in part, by targeted induction of the VEGFR2 gene. Similarly, we found that KLF10−/− mice are impaired in their ability to produce peripheral PACs in response to ischemic injury and that KLF10−/− CMP- and GMP-derived PACs are unable to robustly express VEGFR2 in response to TGF-β1 exposure. Remarkably, KLF10−/− CMP- and GMP-derived PACs were found to possess pronounced defects in specific PAC effector functions, including migration, particularly in response to SDF1-α, and in the release of soluble paracrine factors critical to neovascularization. Furthermore, we provide cogent evidence for the inability of KLF10−/− CMP- or GMP-derived PACs to promote blood flow recovery after hindlimb ischemia in WT or KLF10−/− mice. Compared with WT PACs (derived from equal pools of CMPs and GMPs), KLF10−/− PACs were ineffective at incorporating into capillary structures and reducing injury-induced apoptosis. Taken together, our findings have delineated unique mechanisms through which KLF10 is able to control PAC differentiation and function and have defined the critical role that KLF10 plays in neovascularization.
Other KLFs are involved in hematopoietic progenitor cell differentiation, activation, and function.16,17 For example, KLF1 is highly expressed in the megakaryocyte-erythrocyte progenitors and promotes erythroid maturation by repressing promoter activity of the Fli-1 transcription factor, an ETS-related factor that is required for megakaryopoiesis.25 Another KLF, KLF4, is expressed in monocytes and macrophages. Ectopic overexpression of this factor in either CMPs or HSCs was reported to have preferentially induced differentiation of only monocytes in clonogenic assays. In contrast, inhibition of KLF4 led to increased granulocytes and decreased monocyte maturation.19 In vivo studies have shown that KLF4−/− “chimeras” develop reduced numbers of monocytic cells in BM, resident monocytes (CD115+Gr1−) in spleen, and the near absence of circulating inflammatory monocytes (CD115+Gr1+) in blood.26 KLF4 has also been implicated in regulating macrophage M1/M2 polarization.27 Finally, a recent study has shown that expression of KLF2 is correlated with animals age; circulating hematopoietic progenitors of aged (16- to 18-month-old) mice were greatly reduced compared with levels present in young (4-week-old) mice.28 Overexpression of KLF2 restored defects in these senescent progenitors as evidenced by increased growth potential ex vivo and improved blood flow recovery after hindlimb ischemia.28 Collectively, these observations suggest that KLFs can have profound, often cell-type and stage-specific, phenotypic effects among hematopoietic progenitor cells. The studies presented here extend the roles of KLF proteins to a participatory activity in CMP- and GMP-derived PACs.
Accumulating evidence supports a critical role for TGF-β1 in various aspects of neovascularization. First, studies that use a nonischemic model of femoral artery ligation has shown that exogenous administration of TGF-β1 produced an increase in both the number of collateral arteries as well as the conductance of the collateral circulation in New Zealand White rabbits.29 In addition, another potential role for TGF-β1 has been suggested by the findings related to homing capacities of hematopoietic stem cell/progenitors. A recent study showed that BM cells from TGF-β1−/− neonates developed markedly impaired short- and long-term reconstitutive activity associated with reduced in vivo homing capacity of lineage-negative cells.12 Although the downstream mechanism(s) underlying the homing defect in TGF-β1−/− hematopoietic progenitors remain undefined, clues may be gathered from the fact that TGF-β1 can induce migration and positively regulate the chemokine receptors CXCR4, CCR1, CCR3, CCR5, and CCR6 expression in immune cells, such as T cells or dendritic cells.13,14 In our studies, KLF10−/− CMP- and GMP-derived PACs displayed multiple defects in the expression of the chemokine receptors CXCR4, CXCR3, and CCR7, suggesting that a possible defect in homing, such as with the CXCR4/SDF-1 axis (Figure 3), may be partially responsible for reduced blood flow recovery after hindlimb ischemia in KLF10−/− mice (Figure 4). Indeed, compared with WT mice, KLF10−/− mice exhibited reduced numbers of circulating PACs in response to hindlimb ischemia. However, although local intramuscular injection of WT CMP- and GMP-derived PACs effectively rescued blood flow recovery after hindlimb ischemia in the KLF10−/− mice, KLF10−/− CMP- and GMP-derived PACs had only minimal effects, suggesting that an emigration defect from the BM could not significantly account for the reduced blood flow recovery observed in KLF10−/− mice. Rather, intrinsic chemotactic defects in KLF10−/− PACs may be more critical for tissue neovascularization. In support of a defect in chemotaxis, KLF10−/− CMP- and GMP-derived PACs had markedly reduced migration in Transwell Boyden chambers in vitro. Collectively, these findings suggest that KLF10−/− CMP- and GMP-derived PACs possess striking defects in chemotaxis, an effect which may be important for local tissue invasion or homing or both in response to ischemic injury.
Therapeutic use of PACs have highlighted 2 main mechanisms that may explain their beneficial effects after transplantation: (1) PACs interact with the new vasculature by physically incorporating into the vessel wall or by accumulating periadventitially; (2) PACs participate in paracrine signaling by secreting proangiogenic cytokines and growth factors that may promote de novo angiogenesis or activation of proximal progenitors.1,2,30,31 Consistent with previously reported studies, we noted that WT PACs incorporated into capillary structures at very low frequencies; however, there was minimal incorporation by the KLF10−/− PACs (Figure 4F). Interestingly, under normal steady state conditions, CMPs and GMPs were found to have contributed between 1% and 2% of the mature vascular endothelial cells residing in the portal vein after transgenic parabiosis experiments,32 an effect that lent credence to the notion that these specific progenitors may harbor significant abilities to facilitate endothelial repair processes. Several paracrine defects were also observed from CMP- and GMP-derived KLF10−/− PACs in our study, including decreased release of the growth factor PDGF-AB and the chemokines MCP-1, MIP-1β, and IP-10 in KLF10−/− CMP- and GMP-derived PACs compared with WT PACs (Figure 3E). Several studies have shown that PDGF-AB and PDGF-AA are indispensable for angiogenic events and are necessary for stabilizing newly formed blood vessels.33-35 These chemokines may be important in the recruitment of other PACs or leukocytes, which in turn contribute to development and progression of angiogenesis36 ; for example, MCP-1 can recruit PACs to a wound site to accelerate re-endothelialization.37 Finally, although CMP- and GMP-derived PACs were able to elaborate higher levels of VEGF compared with MEP- or HSC-derived PACs,10 we were surprised to find a striking absence of a decrease in the elaboration of VEGF in KLF10−/− CMP- and GMP-derived PACs compared with WT PACs (data not shown). Thus, it appears that, in response to TGF-β1, KLF10 maintains PAC effector functions by regulating the elaboration of those chemokines and growth factors that are critical to the initiation of angiogenesis.
The ability of TGF-β1 to mediate transdifferentiation of cells into another lineage has been well described with the use of numerous cell systems.38-41 Indeed, TGF-β family members play important roles in epithelial-mesenchymal transformation during normal development and in pathologic conditions and can redirect differentiation along mesenchymal lineages (for adipocytes, osteoblasts, or chondrocytes) in response to TGF-β or bone morphogenetic protein signals. TGF-β1, in particular, has been characterized as being able to regulate expression of endothelial markers; exogenous administration of TGF-β1 increased endothelial-specific expression in mouse embryoid bodies and inhibited expression of endodermal markers.42 However, we did not detect any differences between WT and KLF10−/− PACs for expression of the mesenchymal marker CD105, which was expressed at low levels compared with VEGFR2, after differentiation in vitro (supplemental Figure 7A). In addition, expression of the mesenchymal markers Ng2 and PDGFR were not significantly different after hindlimb ischemia studies in skeletal muscles of WT and KLF10−/− mice (supplemental Figure 7B), suggesting that KLF10 probably does not alter mesenchymal cell expression. Recent studies by others highlighted the ability of TGF-β1 to transdifferentiate BM-derived PACs into proangiogenic smooth muscle cells.43,44 However, we have not observed an increase in smooth muscle markers such as SM-α-actin from PAC differentiation from any of the individual BM progenitors isolated and differentiated into PACs (data not shown). These discordant findings probably reflect the differential approaches used in their studies and ours, namely the types of BM cells (total BM vs prospective isolation of individual BM hematopoietic progenitors), duration of culture (3 weeks vs 7-10 days), and treatment methods (TGF-β1, 5 ng/mL, used between days 15 and 22 vs TGF-β1, 1 ng/mL, used for 7-10 days). Nonetheless, our findings reinforce the notion that TGF-β1 has cell type–specific effects with CMP- and GMP-derived PACs possessing the most responsiveness to TGF-β1–mediated induction of VEGFR2 expression.
Although a variety of cell surface molecules have been proposed for use as markers of the distinct PAC subsets, only a few cell type–specific transcription factors have been identified in PACs or associated with underlying ischemic disease states. One example is the forkhead box-containing protein O subfamily (FOXO) member FOXO3a, which can repress PAC differentiation.45 Investigations into whether TGF-β1/KLF10 signaling may antagonistically regulate the Akt/Foxo3a signaling pathway are thus of interest. To our knowledge, KLF10 is the first member of the KLF family of transcription factors identified in PACs that is associated with both hindlimb ischemia in mice and PAD in human subjects. Future clinical studies will be necessary to determine whether reduced expression of intracellular KLF10 or its upstream signaling pathways in PACs will be effective in providing additional diagnostic or prognostic information for patients with PAD or other ischemic conditions.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Francis W. Luscinskas for helpful discussion and suggestions.
This work was supported by funding from the National Institutes of Health (grants HL080174 and HL091076, M.W.F.; grant F32HL088819, A.K.W.; grant DE14036, T.C.S. and M.S.; and grant HL075771, M.A.C.); the American Cancer Society (Research Scholar grant RSG0719501-LIB, M.W.F.); the Boston Area Diabetes Endocrinology Research Center (pilot grant P30DK057521, M.W.F.); and a Watkins Cardiovascular Medicine Discovery Award (M.W.F.). A.R. is a principal faculty member of the Harvard Stem Cell Institute. S.Y.F. was supported by the Clinical Investigators Training Program: Beth Israel Deaconess Medical Center–Harvard/MIT Health Sciences and Technology, in collaboration with Pfizer Inc and Merck & Co. This research was also supported in part by the Leducq Foundation Network of Research Excellence (A.R. and S.Y.F).
National Institutes of Health
Authorship
Contribution: A.K.W. designed experiments, performed research, analyzed and interpreted data, and wrote the manuscript; S.Y.F., K.C., X.S., B.I., F.E., J.-S.L., E.I.L., D.L.-L., and R.L.P. performed research and analyzed the data; Y.T. performed research; M.S. and T.C.S. provided essential materials (KLF10 knockout mice) and edited the manuscript; M.A.C. and A.R. interpreted the data and edited the manuscript; and M.W.F. designed experiments, performed research, interpreted the data, and wrote the manuscript.
Conflict-of-interest disclosure: M.W.F. and the Brigham and Women's Hospital have a patent pending related to the work that is described in the present study. The remaining authors declare no competing financial interests.
Correspondence: Mark W. Feinberg, Department of Medicine, Cardiovascular Division, Brigham and Women's Hospital, Harvard Medical School, 77 Avenue Louis Pasteur, NRB-742F, Boston, MA 02115; e-mail: mfeinberg@rics.bwh.harvard.edu.

![Figure 4. Effect of KLF10 deficiency on hindlimb ischemia. (A-E) WT or KLF10−/− mice underwent femoral artery ligation to induce hindlimb ischemia. (A) KLF10−/− mice (n = 2 of 21) developed autoamputation of the ischemic leg. Mice were photographed with a Nikon Coolpix 4600 digital camera. (B) Images (left) are representative of blood flow recovery for each time point over 28 days. Quantitation (right) of blood flow recovery was calculated as the mean blood flow (right [ischemic] leg)/left [(nonischemic] leg) by laser Doppler imaging (785-nm near-infrared Laser Doppler Imager-2; Moor Instruments).*P < .01 versus WT; **P < .05 versus WT. (C) FACS analyses of circulating PACs (Sca-1+/VEGFR2+) in WT or KLF10−/− mice 7 days after femoral artery ligation (n = 9-10 per group). *P < .05 versus WT. (D) WT or KLF10−/− PACs (1:1 mix of CMP- and GMP-derived PACs) were intramuscularly injected immediately after femoral artery ligation in KLF10−/− mice. Mean blood flow recovery (ischemic leg/nonischemic leg) was measured by laser Doppler imaging after 3 days. *P < .05 versus WT +PBS. (E-F) Frozen sections of quadriceps muscles harvested 3 days after intramuscular injection of WT or KLF10−/− PACs were labeled with cell tracker (red) and a FITC-conjugated mAb to CD31 (green). (E) Sections were analyzed for CD31 staining with the use of an AQUA/PM2000 Imaging Platform (HistoRx), and automated quantitative analysis was performed with Software suite Version 2.2 (HistoRx). *P < .01 versus WT; n = 4 mice per group. (F) Sections were examined with an Olympus, Fluoview, Model FV1000 camera at 10× magnification and FV10-ASW Version 02.01 software to determine the percentage of labeled PACs (red) that colocalized (yellow) with CD31+ cells (green). *P < .01 versus WT; n = 4 mice per group.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/118/24/10.1182_blood-2011-06-363713/4/m_zh89991179020004.jpeg?Expires=1767704796&Signature=BzyZXhQq0F74vYeLQisUglwbwXOUfW0Xx5JvFgSk6NUXVUsPyJQT5Nwheqq0RerFY2HUzLkj-OoDGOVPXqF76UXfO8eeZaxTP1BTyOfxHm3TAQaOBWnf7BXOhxDLL~Z8QtgmYh~ioVYENwgc9uIW0cMat28qxJI8i6lig8t6jXrm6uEeBdMoIdkoPknFh9CeIvIQvftONwpw6GcVBYEEzR4jvwNFUnQRFk8p08QCR4Ov3m0IlvEKBFHdRj-zLDnwUBCoYmfvA8R3S0-lQAYY5DLq3S6iN9K-ZjzK8d8EGnPd8tmIT7Ob9CsH4TQJ-cdlO9pmvHo8j2OrpAvD2yX4vQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)