Abstract
The control of Plasmodium falciparum erythrocytic parasite density is essential for protection against malaria, because it prevents pathogenesis and progression toward severe disease. P falciparum blood-stage parasite cultures are inhibited by human Vγ9Vδ2 γδ T cells, but the underlying mechanism remains poorly understood. Here, we show that both intraerythrocytic parasites and the extracellular red blood cell–invasive merozoites specifically activate Vγ9Vδ2 T cells in a γδ T cell receptor–dependent manner and trigger their degranulation. In contrast, the γδ T cell–mediated antiparasitic activity only targets the extracellular merozoites. Using perforin-deficient and granulysin-silenced T-cell lines, we demonstrate that granulysin is essential for the in vitro antiplasmodial process, whereas perforin is dispensable. Patients infected with P falciparum exhibited elevated granulysin plasma levels associated with high levels of granulysin-expressing Vδ2+ T cells endowed with parasite-specific degranulation capacity. This indicates in vivo activation of Vγ9Vδ2 T cells along with granulysin triggering and discharge during primary acute falciparum malaria. Altogether, this work identifies Vγ9Vδ2 T cells as unconventional immune effectors targeting the red blood cell–invasive extracellular P falciparum merozoites and opens novel perspectives for immune interventions harnessing the antiparasitic activity of Vγ9Vδ2 T cells to control parasite density in malaria patients.
Introduction
Clinical malaria is associated with the intraerythrocytic asexual replication cycle of the Plasmodium sp parasite. Whereas young intraerythrocytic-stage parasites circulate in the blood, mature intraerythrocytic-stage parasites (trophozoites and schizonts) are sequestered in the microcirculation. On completion of intraerythrocytic development, extracellular invasive merozoites are released into the bloodstream, where they invade new red blood cells (RBCs), thus exponentially amplifying the density of blood-stage parasites. Control of parasite density is essential for protection against malaria, because it prevents pathogenesis and progression toward severe disease.
Despite major research efforts, the immune mechanisms involved in the control of parasite biomass remain poorly understood. This lack of understanding impedes the rational development of immune-based interventions to prevent or cure malaria. Analysis of immune effectors that control blood-stage parasites has mainly focused on antibody-dependent mechanisms, as passive transfer of immunoglobulins dramatically reduced parasite density in children with malaria.1,2 Little attention has been paid to early immune responses that play, however, a pivotal role in the race between parasite development and the deployment of protective adaptive immune mechanisms. Recent studies have highlighted the role of innate immune effectors, including innate lymphocytes, in the early control of parasitemia before significant levels of specific antibodies are produced; however, the underlying effector mechanisms remain poorly understood.3
γδ T cells expressing the Vγ9 and Vδ2 chains of the T-cell receptor represent a nonconventional T-lymphocyte subset found only in primates that accounts for 0.5% to 5% of peripheral T cells. γδ T cells circulate in the blood, patrolling vascular beds, readily responding to tumor cells and bloodborne pathogens such as Plasmodium, and participating in the early immune response and in the onset of adaptive immunity.4 They react specifically to minute amounts of small nonpeptidic metabolites, known as phosphoantigens, independent of processing or presentation by professional antigen-presenting cells.5 The most active phosphoantigens are intermediate products of the deoxy-xylulose-5-phosphate isoprenoid synthesis pathway that occurs in the Plasmodium apicoplast.6,7 During a primary malaria infection, Vγ9Vδ2 T cells are rapidly activated and expanded, reaching frequencies of up to 30% of circulating T cells.8,9
Previous studies have demonstrated that Vγ9Vδ2 T cell clones can inhibit blood-stage P falciparum parasites in vitro10,11 ; however, the contribution of this effect to the overall antiparasitic activity of PBMCs, the actual parasite developmental stage(s) that activate and trigger γδ T cell-inhibitory activity, the parasite stage(s) targeted by the γδ T cells, and the role of cytotoxic effector molecules in this process remain unclear. Furthermore, little is known concerning the in vivo activation and antiparasitic status of Vγ9Vδ2 T cells. Yet, this information is crucial to understand how γδ T cells contribute to the early control of parasite density and to harness this process to improve the control of parasite multiplication in primary infected patients.
Here, we elucidate the mechanism by which γδ T cells inhibit in vitro P falciparum blood-stage development. We report that both intracellular and extracellular stages specifically trigger Vγ9Vδ2 T cell antiparasitic activity through a TCR-dependent mechanism. Furthermore, we demonstrate that the free RBC-invasive merozoite is the only vulnerable stage in this process and that granulysin, but not perforin, is the crucial mediator of parasite inhibition. We also documented the in vivo relevance of these data by showing the presence of high levels of Plasmodium-reactive Vγ9Vδ2 T lymphocytes expressing granulysin along with high concentrations of plasma granulysin in P falciparum–infected patients. These data identify the Plasmodium merozoite as a novel activator and target of an unconventional lymphocyte subset and highlight the RBC as a niche protecting the parasite from cytotoxic mediators. Furthermore, our findings emphasize Vγ9Vδ2 T cell–mediated production of granulysin as an underestimated immune effector in malaria.
Methods
Parasite culture
P falciparum FCR3 parasites were grown in O+ RBC (EFS Aquitaine), cultured in RPMI-1640 supplemented with 10% human serum, as described previously,12 and they were regularly tested for absence of mycoplasma contamination. Parasites were synchronized by repeated sorbitol treatments. Trophozoite or schizont stages were purified by gel flotation.13
Free merozoites were isolated as described previously.14 In brief, highly synchronized midstage schizonts were purified by gel flotation, set to mature until the late-schizont stage (4-16 nuclei), and incubated with 10μM E64 (Sigma-Aldrich). After 8 hours, the culture was centrifuged for 5 minutes at 500g to remove contaminant schizonts. Supernatant containing parasitophorous-enclosed membrane merozoites was harvested, centrifuged at 2000g for 10 minutes, and enumerated. Subsequently, free merozoites were released by mild mechanical treatment. Contamination by intact schizonts was assessed by microscopic examination of Giemsa-stained smear and represented < 5%.
Generation of Vγ9Vδ2 T-cell lines
To generate Vγ9Vδ2 T-cell lines, PBMCs from healthy donors (EFS Aquitaine) were stimulated with phosphoantigens (50μM isopentenyl pyrophosphate [Sigma-Aldrich], 400nM bromohydrin pyrophosphate [BrHPP; IPH1101, Innate Pharma], a P falciparum phosphoantigen-enriched fraction6 ) or with intact purified P falciparum trophozoites and expanded in bulk in complete medium (CM; RPMI-1640 supplemented with 10% human serum, glutamine, and antibiotics) in the presence of IL-2 (300 IU/mL; PeproTech). Short-term Vγ9Vδ2 T-cell lines were functionally tested without further restimulation when they reached at least 75% of purity. For long-term Vγ9Vδ2 T-cell lines (S1 and JT lines), Vδ2 cells were sorted after 2 weeks of stimulation by positive magnetic separation (Miltenyi Biotec), subsequently restimulated with PHA-L (Sigma-Aldrich) and IL-2 (1000 IU/mL), and irradiated PBMCs, as described previously.15 Long-term T-cell lines were tested between 3 and 4 weeks after restimulation. The same procedure was followed to generate the Vγ9Vδ2 PFNdef T-cell line from a genetically perforin-deficient familial hemophagocytic lymphohistiocytosis patient with heterozygous missense mutations (G3A and G695A; Hôpital Necker).16 The Vγ4Vδ5 (4-29) T-cell clone and the Vδ3VγI T-cell line, both reactive against the colon cancer cell line HT29, and the clone T4A.5 αβ CD4+ T-cell clone were derived as described previously15,17 and restimulated under the same conditions.
Lentiviral shRNA design and T-lymphocyte transfection
The shRNA target-specific sequences were described previously: GNLYsh1 5′-AAGCCCACCCAGAGAAGTGTT-3′ and GNLYsh2 5′-GGAGGTATCAGTCTAGAGTTT-3′ were used.18 The nonsilencing (NS) sequence 5′-AAGAACGACTAGGTGGAGAA-3′ was used as a control. To produce granulysin-specific shRNA lentiviral vectors (LVs), 68 mers were designed as follows: 5′-AGCTTCC-sense21mer-TTCAAGAGA-antisense21mer-TTTTTGGAAG-3′ and phosphorylated as described at http://tronolab.epfl.ch/. Double-stranded oligonucleotides were cloned into a HindIII/Sal1-digested pIC20R (vector 30; Plateforme de Vectorologie, Bordeaux University) downstream of the H1 RNA polymerase III promoter. pIC20R-shRNA were subsequently digested by Cla1 and Sal1, and the H1/shRNA inserts obtained were subcloned into pTRIPdsRED2 (vector 117; Plateforme de Vectorologie). All the constructs were confirmed by sequencing.
LVs were produced by transient transfection of 293T cells according to standard protocols.19 Subsequently, Vγ9Vδ2 T-cell lines were infected with LV (MOI = 10) in the presence of protamine sulfate (Sigma-Aldrich). After 1 week, infected dsRED-positive Vγ9Vδ2 T cells were sorted by flow cytometry (FACSAria cell sorter; BD Biosciences) and restimulated as described in the preceding paragraph. The efficiency of silencing was assessed at the mRNA and protein levels using RT-PCR and Western blotting, respectively (see supplemental Methods, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
CD107a assay
The degranulation assay was performed as described previously.20 In brief, cells were incubated for 6 hours with schizonts, merozoites, or uninfected RBCs (uiRBCs) at various effector/target (E/T = cells/parasites) ratios in the presence of IL-2 (20 IU/mL), except in experiments using patients' cells, for which no IL-2 was added. Anti-CD107a mAb or isotype control (BD Biosciences) was added at the onset of the incubation. Cells were harvested, stained with anti-Vδ2 or anti-CD3 mAb (Beckman Coulter), and then analyzed by flow cytometry using an FACSCanto flow cytometer (BD Biosciences). For blocking experiments, cells were preincubated for 1 hour with anti-Vδ2 (clone immu389; Beckman Coulter) or anti-NKG2D (clone 149810; R&D Systems) at varying concentrations.
Parasite growth inhibition assay
For assays using PBMCs, PBMCs magnetically depleted or not of Vδ2+ T cells (Miltenyi Biotec) were stimulated with 400nM BrHPP (Innate Pharma) in CM without cytokines for 40 hours before being tested. For assays using Vγ9Vδ2 T-cell or control cell lines, cells were incubated in CM supplemented with IL-2 (20 IU/mL) or IL-15 (50 ng/mL; PeproTech) for 24 hours before being tested. Cells were cocultured in a 96-well microtiter plates at a specific E/T ratio with a trophozoite synchronized culture adjusted to 1% parasitemia and 1% final hematocrit for 24 hours. Ring parasitemia was assessed by flow cytometry (FACSCanto; BD Biosciences) using hydroethidine staining21 (for details, see supplemental Methods and supplemental Figure 1). Results were confirmed by microscopic examination of Giemsa-stained smears. Antiparasitic activity (percentage) was calculated as follows: 100 − [(average % parasitemia of replicate test culture/average % parasitemia of replicate control culture) × 100].
To test whether schizonts were targeted by Vγ9Vδ2 cells, schizonts (34-40 hours after invasion) were incubated with the Vγ9Vδ2 T cells for 6 hours, and Vγ9Vδ2 T cells were removed before schizont rupture using anti-CD2–Dynabeads (Invitrogen). Mock-treated parasites cultured without cells were used as controls. Parasites were then cultured for an additional 18 hours, and parasitemia was assessed by hydroethidine staining.
Merozoite reinvasion assay
T cells were incubated with purified merozoites and uiRBCs for 28 hours, and the parasitemia resulting from red blood cell reinvasion was assessed by hydroethidine staining. Inhibition of merozoite reinvasion (percentage) was calculated as follows: 100 − [(average % parasitemia with cells/average % parasitemia without cells) × 100].
Clinical samples and flow cytometry
PBMCs were isolated from clinical blood sample leftovers of P falciparum–infected patients admitted to the Teaching University Hospital of Bordeaux and from healthy donors from the blood bank (EFS Aquitaine). Patients were informed according to the rules of the hospital ethical board, and the research was approved by the University of Bordeaux Institutional Review Board. PBMCs were stained directly with mAb specific for CD3, CD27, and CD45RA (BD Biosciences), as well as Cδ and Vδ2 (Beckman Coulter). For granulysin staining, PBMCs were first stained with anti-CD3 and anti-Vδ2 mAbs and then fixed in 2% formaldehyde, permeabilized in 0.1% Triton, and incubated with anti-granulysin mAb (BD Biosciences). Cells were analyzed by 6-color flow cytometry using FACSCanto and FACSDiva software (BD Biosciences).
Granulysin ELISA
Granulysin ELISAs were performed on plasma and culture supernatants as described previously.22
Statistical analysis
Wilcoxon signed rank test was used for paired comparisons, Mann-Whitney or Kruskal-Wallis test was used for unpaired comparisons, and Spearman rank was used for correlation analysis. P values ≤ .05 were considered significant.
Results
Vγ9Vδ2 T cells exhibit antiparasitic activity in PBMCs or as purified T-cell lines
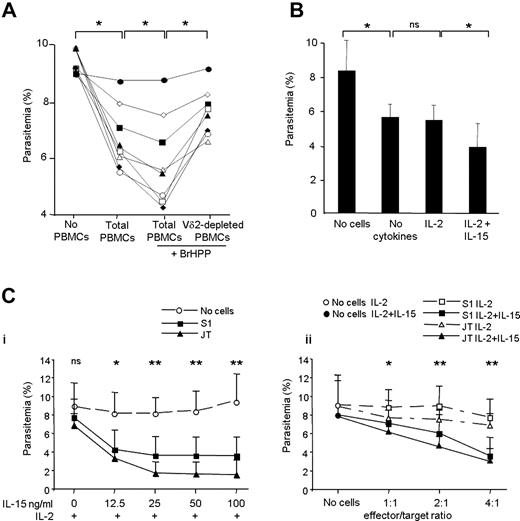
We first assessed the antiparasitic activity of Vγ9Vδ2 T cells in PBMCs using a parasite growth inhibition assay. In comparison with parasites alone, a decrease of parasitemia was observed in parasite coculture with resting PBMCs for all but 1 donor. This decrease was slightly enhanced when the PBMCs were activated before performing the parasite growth inhibition assay with the synthetic phosphoantigen BrHPP that selectively stimulates the Vγ9Vδ2 T cells. Depletion of Vδ2+ T cells from PBMCs before activation reduced the inhibitory effect of BrHPP-activated PBMCs (Figure 1A). Of note, the effect of resting PBMCs on parasitemia was similar whether or not Vδ2+ T cells were depleted (data not shown). Together, this suggests that although Vγ9Vδ2 T cells represent a minor subset of PBMCs (ranging from 0.5% to 1.9% of PBMCs for the donors analyzed), once activated, they contribute to PBMCs' parasite growth inhibition.
Antiplasmodial activity of Vγ9Vδ2 T cells in PBMCs and as purified T-cell lines. (A) Undepleted PBMCs (total PBMCs) or Vδ2+ T cell–depleted PBMCs (Vδ2-depleted PBMCs) from 8 different healthy donors were activated with BrHPP (400nM) or left untreated for 40 hours and then cocultured in a standard parasite inhibition assay at a 4/1 E/T ratio with a synchronized trophozoite culture for 24 hours. At the end of this period, parasitemia in cocultured samples was compared with that in synchronized trophozoite cultures incubated without PBMCs by hydroethidine staining. The percentage of Vδ2+ CD3+ cells among total PBMCs varied among the donors (from 0.5% to 1.9%). Data represent the parasitemia (means of duplicates) of cocultures with PBMCs of each donor tested (n = 8; *P ≤ .05 by the Wilcoxon signed ranked test). (B) Short-term Vγ9Vδ2 T-cell lines (STL) were tested after a 24-hour priming with no cytokine added or with IL-2 (20 IU/mL) only or with IL-15 (50 ng/mL) and cocultured with the parasites at a 4/1 E/T ratio in a standard parasite inhibition assay. Data represent the mean parasitemia in the various cocultures conditions (n = 10 STL; **P ≤ .01 for Wilcoxon signed ranked test comparisons). (C) S1 and the JT long-term Vγ9Vδ2 T-cell lines were (i) primed for 24 hours with IL-2 (20 IU/mL) and increasing doses of IL-15 and cocultured with the parasites at a 4/1 E/T ratio or (ii) primed for 24 hours with IL-2 (20 IU/mL) with or without added IL-15 (50 ng/mL) and cocultured with the parasites at increasing E/T ratios as indicated. Graphs represent the mean of parasitemia ± SD of 4 independent experiments (n = 4; *P ≤ .05 and **P ≤ .01 by Mann-Whitney rank sum test; ns indicates not significant).
Antiplasmodial activity of Vγ9Vδ2 T cells in PBMCs and as purified T-cell lines. (A) Undepleted PBMCs (total PBMCs) or Vδ2+ T cell–depleted PBMCs (Vδ2-depleted PBMCs) from 8 different healthy donors were activated with BrHPP (400nM) or left untreated for 40 hours and then cocultured in a standard parasite inhibition assay at a 4/1 E/T ratio with a synchronized trophozoite culture for 24 hours. At the end of this period, parasitemia in cocultured samples was compared with that in synchronized trophozoite cultures incubated without PBMCs by hydroethidine staining. The percentage of Vδ2+ CD3+ cells among total PBMCs varied among the donors (from 0.5% to 1.9%). Data represent the parasitemia (means of duplicates) of cocultures with PBMCs of each donor tested (n = 8; *P ≤ .05 by the Wilcoxon signed ranked test). (B) Short-term Vγ9Vδ2 T-cell lines (STL) were tested after a 24-hour priming with no cytokine added or with IL-2 (20 IU/mL) only or with IL-15 (50 ng/mL) and cocultured with the parasites at a 4/1 E/T ratio in a standard parasite inhibition assay. Data represent the mean parasitemia in the various cocultures conditions (n = 10 STL; **P ≤ .01 for Wilcoxon signed ranked test comparisons). (C) S1 and the JT long-term Vγ9Vδ2 T-cell lines were (i) primed for 24 hours with IL-2 (20 IU/mL) and increasing doses of IL-15 and cocultured with the parasites at a 4/1 E/T ratio or (ii) primed for 24 hours with IL-2 (20 IU/mL) with or without added IL-15 (50 ng/mL) and cocultured with the parasites at increasing E/T ratios as indicated. Graphs represent the mean of parasitemia ± SD of 4 independent experiments (n = 4; *P ≤ .05 and **P ≤ .01 by Mann-Whitney rank sum test; ns indicates not significant).
To directly assess the effect of Vγ9Vδ2 T cells, 10 short-term Vγ9Vδ2 T-cell lines (STLA to STLJ) derived from different donors by stimulation of PBMCs with phosphoantigens (either BrHPP or P falciparum phosphoantigen-enriched fraction) were tested for their ability to inhibit parasite growth. Parasite growth was inhibited by γδ T-cell lines in absence of added cytokines and similarly when cells were exposed to low quantities of IL-2 (20 IU/mL; Figure 1B). Since IL-15 has been shown to favor the differentiation of cytotoxic-effector phenotype of γδ T cells23 and enhance their growth-inhibitory activity,24 cells were tested after 24 hours of incubation with IL-15 in addition to IL-2. Parasite growth inhibition was most pronounced under this condition (Figure 1B) and individual γδ T-cell lines growth inhibitions ranged from 35% to 72% (supplemental Table 1). These data indicate that freshly expanded Vγ9Vδ2 T-cell lines inhibit parasite growth, with an optimal effect achieved by cells incubated with IL-15.
To gain insight into the mechanisms underlying the γδ T cell–mediated antiparasitic activity, 2 stable long-term Vγ9Vδ2+ cells T-cells lines (> 95% pure) were generated from 2 different donors after stimulation with isopentenyl pyrophosphate (S1) or intact live trophozoites (JT). These T-cell lines were maintained through repeated PHA restimulation and required IL-2 (20 IU/mL) for their survival. For both T-cell lines, reproducible parasite growth inhibitions was dependent on the IL-15 dose, with the maximum inhibition reached (80%) with IL-15 doses greater than 25 ng/mL (Figure 1Ci) and E/T ratios of 4/1 (Figure 1Cii). Of note, inhibition efficiency did not depend on the antigen used to derive the cell line (ie, phosphoantigen or intact trophozoite). Vγ9Vδ2 T cells express various natural killer (NK) receptors that can modulate their functions.25 The S1 and JT cell lines exhibited stable expression of NK cell receptors, most of which were comparable in both cell lines, except CD94/NKG2A and CD56, which were more highly expressed on JT cells (supplemental Figure 2). These data indicated that the S1 and JT cell lines, although generated differently, were phenotypically and functionally similar and represented useful tools to further investigate the antiparasitic activity of γδ T cells. Based on these findings, a 4/1 E/T ratio after 24 hours of incubation in the presence of IL-15 (50 ng/mL) in addition to IL-2 (20 IU/mL) was used throughout the study to assess the antiparasitic activity of the long-term γδ T-cell lines.
Granulysin, not perforin, mediates Vγ9Vδ2 T-cell antiparasitic activity
Separation of γδ T cells from the parasite culture in a Transwell insert culture system abolished the parasite growth inhibition (supplemental Figure 3), confirming that contact or proximity between effector cells and parasites was required.10,26 The cytotoxic activity of T lymphocytes, including γδ T cells, operates via 2 major pathways: 1 pathway involves the ligation of death receptors on the target cells, whereas the second pathway is dependent on the exocytosis-mediated delivery of cytotoxic granule content, such as perforin, granzymes, or granulysin, in the vicinity of the target cell.27 Whether infected or not, RBCs do not express Fas or death receptors for TRAIL (supplemental Figure 4), ruling out a possible involvement of this pathway in cytotoxicity against blood-stage parasites. This is in line with previous findings showing that the antiparasitic activity of γδ T cells relies on granule exocytosis.26 We thus investigated the roles of perforin and granulysin, 2 cytotoxic molecules involved in the killing of various microorganisms, including bacteria28-30 and fungi.18 To assess the role of perforin, a long-term Vγ9Vδ2 T-cell line (PFNdef) was generated from a perforin-deficient patient. The PFNdef line expressed normal levels of granulysin but no detectable perforin (Figure 2A). Parasite inhibition by PFNdef was similar to the perforin-proficient cell lines S1 and JT (P > .05), indicating that perforin was dispensable for antiplasmodial activity (Figure 2B). Importantly, the irrelevant αβ T-cell clone T4A5 did not display any inhibitory activity under the same conditions.
Perforin is dispensable for Vγ9Vδ2 antiparasitic activity. A Vγ9Vδ2 T-cell line was generated from a perforin-deficient familial hemophagocytic lymphohistiocytosis (FLH) patient, and its antiparasitic activity was assessed in a standard parasite inhibition assay. (A) Flow cytometry histograms showing perforin and granulysin expression in Vγ9Vδ2 T-cell lines generated from 2 different donors (S1 and JT) and from an FLH patient (PFNdef). Mean fluorescence intensity (MFI) for perforin and granulysin intracellular staining is indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (B) Comparison of the antiparasitic activity of the PFNdef, S1 and JT cell lines. The αβ T4A.5 T-cell clone was used as a negative control. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 4 independent experiments (n = 4; *P ≤ .05 by Mann-Whitney rank sum test comparing the PFNdef cell line with the S1, JT, or T4A.5 T-cell lines).
Perforin is dispensable for Vγ9Vδ2 antiparasitic activity. A Vγ9Vδ2 T-cell line was generated from a perforin-deficient familial hemophagocytic lymphohistiocytosis (FLH) patient, and its antiparasitic activity was assessed in a standard parasite inhibition assay. (A) Flow cytometry histograms showing perforin and granulysin expression in Vγ9Vδ2 T-cell lines generated from 2 different donors (S1 and JT) and from an FLH patient (PFNdef). Mean fluorescence intensity (MFI) for perforin and granulysin intracellular staining is indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (B) Comparison of the antiparasitic activity of the PFNdef, S1 and JT cell lines. The αβ T4A.5 T-cell clone was used as a negative control. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 4 independent experiments (n = 4; *P ≤ .05 by Mann-Whitney rank sum test comparing the PFNdef cell line with the S1, JT, or T4A.5 T-cell lines).
To assess the role of granulysin, we used RNA interference to generate granulysin knockdown T-cell lines. The S1 line was infected with a lentiviral vector expressing GNLYsh1 or GNLYsh2 granulysin-specific shRNA, resulting in Gnly1 or Gnly2 cell lines, respectively. A non-silencing (NS) shRNA was used as a control. Granulysin mRNA expression was found to be reduced in the Gnly1 and Gnly2 cell lines compared with the NS or noninfected S1 lines (Figure 3A). Importantly, immunoblotting showed that the amount of granulysin protein in both shRNA-expressing cell lines was much lower than that in the NS or the noninfected S1 lines (Figure 3B). Perforin expression remained unaltered, indicating specific shRNA targeting. Moreover, the 3 lentivirus-infected Vγ9Vδ2 T-cell lines produced similar levels of TNF-α following phosphoantigen stimulation, although slightly lower than the noninfected S1 cell line (supplemental Figure 5). This supports the notion that, aside from decreased granulysin expression, the functional responses of the lentivirus-infected lines are maintained. Reduced granulysin expression was stable over time and consistently more pronounced in the Gnly2 than in Gnly1 cell line (Figure 3C). The inhibitory activity of the silenced cell lines was significantly reduced (P ≤ .05; Figure 3D). Interestingly, the greatest loss of inhibitory activity was observed in the Gnly2 cell line that also displayed the lowest expression of granulysin. These data show that granulysin, but not perforin, is essential for the Vγ9Vδ2 T cell–mediated antiparasitic activity.
Granulysin is essential for Vγ9Vδ2 antiparasitic activity. The S1 T-cell line was infected with the lentiviral vector containing the granulysin-specific shRNA sequences GNLYsh1, GNLYsh2, or a NS shRNA sequence, and their antiparasitic activity has been assessed in a standard parasite inhibition assay. (A) RT-PCR assessment of granulysin mRNA levels in the noninfected S1 cell line (Ctrl) or S1 cell line infected with NS, GNLYsh1 (Gnly1), or GNLYsh2 (Gnly2) shRNA constructs. β2-Microglobulin mRNA levels were measured as a control. (B) Granulysin and perforin protein levels were detected in S1 (Ctrl), NS, Gnly1, and Gnly2 cell lines by Western blotting. Actin expression was measured as a loading control. (C) Intracellular granulysin expression was measured using flow cytometry in the NS, Gnly1, and Gnly2 cell lines. The percentage of granulysin-positive cells and the MFI of granulysin intracellular staining are indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (D) Antiparasitic activity of the NS, Gnly1, and Gnly2 cell lines. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 2 independent experiments (n = 2; *P ≤ .05 by Mann-Whitney rank sum test comparing NS with Gnly1 and Gnly2 T-cell lines).
Granulysin is essential for Vγ9Vδ2 antiparasitic activity. The S1 T-cell line was infected with the lentiviral vector containing the granulysin-specific shRNA sequences GNLYsh1, GNLYsh2, or a NS shRNA sequence, and their antiparasitic activity has been assessed in a standard parasite inhibition assay. (A) RT-PCR assessment of granulysin mRNA levels in the noninfected S1 cell line (Ctrl) or S1 cell line infected with NS, GNLYsh1 (Gnly1), or GNLYsh2 (Gnly2) shRNA constructs. β2-Microglobulin mRNA levels were measured as a control. (B) Granulysin and perforin protein levels were detected in S1 (Ctrl), NS, Gnly1, and Gnly2 cell lines by Western blotting. Actin expression was measured as a loading control. (C) Intracellular granulysin expression was measured using flow cytometry in the NS, Gnly1, and Gnly2 cell lines. The percentage of granulysin-positive cells and the MFI of granulysin intracellular staining are indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (D) Antiparasitic activity of the NS, Gnly1, and Gnly2 cell lines. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 2 independent experiments (n = 2; *P ≤ .05 by Mann-Whitney rank sum test comparing NS with Gnly1 and Gnly2 T-cell lines).
Accordingly, the granulysin concentrations measured in the supernatants harvested at the end of the parasite growth inhibition test in the 10 short-term Vγ9Vδ2 T-cell lines positively correlated with the antiparasitic activities of the individual lines (supplemental Figure 6).
Schizonts-infected RBCs and extracellular merozoites trigger Vγ9Vδ2 T-cell degranulation in a TCR-dependent manner
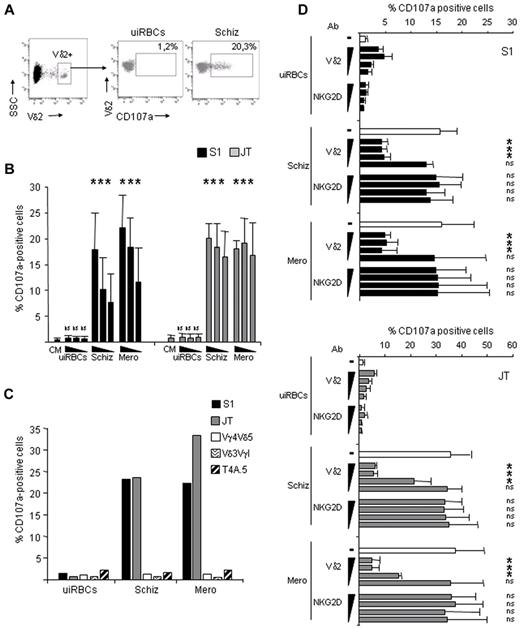
The release of granulysin and other cytotoxic lysosomal molecules via exocytosis (degranulation) is associated with transient cell surface expression of lysosomal membrane-associated glycoproteins such as CD107a (Lamp1).20 To identify the parasitic stages that trigger Vγ9Vδ2 T-cell degranulation, we performed a CD107a mobilization assay in the presence of schizonts or merozoites. Both stages triggered dose-dependent CD107a surface expression by the S1 and JT lines, whereas uiRBCs did not induce any significant CD107a expression (Figure 4A-B). In contrast, no degranulation was observed in γδ T cells expressing other T-cell receptor chains such as Vγ4Vδ5 or Vδ3VγI, or in the αβ-T4A.5 T-cell clone, suggesting specific Vγ9Vδ2 TCR involvement in degranulation (Figure 4C). To confirm this, we performed CD107a assays in the presence of an anti-Vδ2 blocking antibody.31 An anti-NKG2D blocking antibody was used as a relevant isotype control,15 because NKG2D is another activating receptor expressed by the S1 and JT cell lines (supplemental Figure 2). The anti-Vδ2 antibody, but not the anti-NKG2D antibody, inhibited the expression of CD107a triggered by schizonts and merozoites in a dose-dependent manner in both T-cell lines (Figure 4D). Thus, both intraerythrocytic-stage (ie, schizonts) and extracellular-stage parasites (ie, merozoites) specifically induced Vγ9Vδ2 degranulation in a TCR-dependent manner.
Vγ9Vδ2 T cells degranulate in the presence of trophozoites and merozoites in a TCR-dependent mechanism. The S1 and JT Vγ9Vδ2 T-cell lines were incubated for 6 hours with uiRBCs, purified schizonts (Schiz), or merozoites (Mero), and CD107a surface expression was detected as described in “Methods.” (A) Representative flow cytometry dot-plot showing the gating strategy for Vδ2+ T cells and for detection of CD107a surface expression on gated cells after incubation with uiRBCs or schizonts. (B) Percentage of CD107a+ cells from S1 and JT cell lines incubated in CM or with uiRBCs, purified schizonts, or merozoites at decreasing E/T ratios (1/10, 1/5, and 1/2.5). Data represent mean ± SD of 4 independent experiments (n = 4) and were obtained by collecting of 10 000 Vδ2+ events (*P ≤ .05 by Mann-Whitney rank sum test comparing cells incubated with uiRBCs, schizonts, or merozoites with cells incubated in CM). (C) Percentage of CD107a+ cells among S1 and JT cells, or among control T cells (a Vγ4Vδ5 T-cell line, a Vδ3VγI T-cell line, and an αβ T4A.5 T-cell clone) incubated in uiRBCs, purified schizonts, or merozoites at 1/10 E/T ratio. The figure is representative of 3 independent experiments (n = 3). (D) Percentage of CD107a+ cells among S1 (top) and JT cells (bottom) preincubated for 1 hour with 1, 0.5, 0.1, and 0.01 μg/mL of anti-Vδ2 (IgG1, clone immu389) or anti-NKG2D (IgG1, clone 149810) blocking antibodies and then incubated with uiRBCs, purified schizonts, or merozoites at 1/10 E/T ratio. Data represent mean ± SD of 4 independent experiments (n = 4) and were obtained by collecting 10 000 Vδ2+ events (*P ≤ .05 by Mann-Whitney rank sum test comparing cells incubated with different concentrations of anti-Vδ2 or anti-NKG2D blocking antibodies with untreated cells on schizont or merozoite stimulation).
Vγ9Vδ2 T cells degranulate in the presence of trophozoites and merozoites in a TCR-dependent mechanism. The S1 and JT Vγ9Vδ2 T-cell lines were incubated for 6 hours with uiRBCs, purified schizonts (Schiz), or merozoites (Mero), and CD107a surface expression was detected as described in “Methods.” (A) Representative flow cytometry dot-plot showing the gating strategy for Vδ2+ T cells and for detection of CD107a surface expression on gated cells after incubation with uiRBCs or schizonts. (B) Percentage of CD107a+ cells from S1 and JT cell lines incubated in CM or with uiRBCs, purified schizonts, or merozoites at decreasing E/T ratios (1/10, 1/5, and 1/2.5). Data represent mean ± SD of 4 independent experiments (n = 4) and were obtained by collecting of 10 000 Vδ2+ events (*P ≤ .05 by Mann-Whitney rank sum test comparing cells incubated with uiRBCs, schizonts, or merozoites with cells incubated in CM). (C) Percentage of CD107a+ cells among S1 and JT cells, or among control T cells (a Vγ4Vδ5 T-cell line, a Vδ3VγI T-cell line, and an αβ T4A.5 T-cell clone) incubated in uiRBCs, purified schizonts, or merozoites at 1/10 E/T ratio. The figure is representative of 3 independent experiments (n = 3). (D) Percentage of CD107a+ cells among S1 (top) and JT cells (bottom) preincubated for 1 hour with 1, 0.5, 0.1, and 0.01 μg/mL of anti-Vδ2 (IgG1, clone immu389) or anti-NKG2D (IgG1, clone 149810) blocking antibodies and then incubated with uiRBCs, purified schizonts, or merozoites at 1/10 E/T ratio. Data represent mean ± SD of 4 independent experiments (n = 4) and were obtained by collecting 10 000 Vδ2+ events (*P ≤ .05 by Mann-Whitney rank sum test comparing cells incubated with different concentrations of anti-Vδ2 or anti-NKG2D blocking antibodies with untreated cells on schizont or merozoite stimulation).
RBC-invasive merozoites are the targets of the Vγ9Vδ2 T-cell antiparasitic activity
Vγ9Vδ2 T cell–mediated parasite inhibition may reflect cytotoxicity targeting either the developing intracellular trophozoites or schizonts or the invasive extracellular merozoites. Examination of Giemsa-stained smears failed to identify intracellular parasites with abnormal morphology or pyknotic forms, and schizont maturation seemed undelayed (data not shown), suggesting that trophozoites or schizonts were insensitive to the Vγ9Vδ2 T-cell antiparasitic activity. To exclude the possibility that schizonts could release impaired or less invasive merozoites after contact with Vγ9Vδ2 T cells, we removed the cells from the culture 6 hours after coculture (just before schizont rupture), and we incubated the culture for an additional 24 hours (Figure 5Ai), which abrogated the inhibitory activity of the S1 and JT cell lines (Figure 5Aii-iii). These results indicate that Vγ9Vδ2 T cells do not inhibit schizont maturation or merozoite development, since merozoites were invasive after egress; however, granulysin was exocytosed during the 6 hours of contact with the maturing schizonts, because the intracellular amount of granulysin after 6 hours of coculture (T6 hours) was lower than that before the incubation period (T0; Figure 5Aiii).
Merozoites, not trophozoites, are the target of Vγ9Vδ2 antiparasitic activity. (A) Primed S1 or JT Vγ9Vδ2 T cells were cocultured with purified trophozoites (E/T ratio 4/1) for either 24 hours until merozoite reinvasion (no removal of γδ) or were removed by magnetic depletion after 6 hours of coculture, just before schizont rupture; [removal of γδ(T6h)]. Mock-treated parasites cultured without cells were used as a control. After cell removal, the parasitemia was similar under the various conditions. (i) Schematic representation of the experimental design. (ii) Antiparasitic activity was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represents the mean ± SD of the antiparasitic activity observed in 3 independent experiments performed in duplicate (*P ≤ .05 for Mann-Whitney rank sum test comparing the conditions [removal of γδ] and [no removal of γδ] for each T-cell line). (iii) Histograms represent the mean of parasitemia ± SD observed in 1 representative experiment performed in duplicate with the S1 and the JT cell lines. No cells: parasites cultured in the absence of cells (*P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia of parasites cultured in the presence of T cells [S1 or JT] with the parasitemia in absence of T cells [no cells], for each condition (that is, [removal of γδ] or [no removal of γδ]). Flow cytometry histograms show granulysin expression in the S1 and JT cell lines before (T0) and after 6 hours (T6hr) of coculture with trophozoite-stage parasites. Dotted lines represent isotype control antibody. (B) Purified merozoites were incubated with fresh uiRBCs alone (no cells) or in the presence of S1 or JT T cells or the αβ T4A.5 T-cell clone, and the parasitemia was assessed after 28 hours. (i) Schematic representation of the experimental design. (ii) Inhibition of merozoite reinvasion (percentage) was calculated as 100 − [(average % parasitemia with cells/average % parasitemia without cells) × 100]. Data represent the mean ± SD of the inhibition of merozoite invasion observed in 3 independent experiments performed in duplicate (n = 3; *P ≤ .05 by Mann-Whitney rank sum test comparing S1 or JT with T4A.5). (iii) Parasitemia from 1 representative experiment is shown (mean ± SD; *P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia in the presence of T cells [S1, JT, or T4A.5] with the parasitemia in absence of T cells [no cells]).
Merozoites, not trophozoites, are the target of Vγ9Vδ2 antiparasitic activity. (A) Primed S1 or JT Vγ9Vδ2 T cells were cocultured with purified trophozoites (E/T ratio 4/1) for either 24 hours until merozoite reinvasion (no removal of γδ) or were removed by magnetic depletion after 6 hours of coculture, just before schizont rupture; [removal of γδ(T6h)]. Mock-treated parasites cultured without cells were used as a control. After cell removal, the parasitemia was similar under the various conditions. (i) Schematic representation of the experimental design. (ii) Antiparasitic activity was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represents the mean ± SD of the antiparasitic activity observed in 3 independent experiments performed in duplicate (*P ≤ .05 for Mann-Whitney rank sum test comparing the conditions [removal of γδ] and [no removal of γδ] for each T-cell line). (iii) Histograms represent the mean of parasitemia ± SD observed in 1 representative experiment performed in duplicate with the S1 and the JT cell lines. No cells: parasites cultured in the absence of cells (*P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia of parasites cultured in the presence of T cells [S1 or JT] with the parasitemia in absence of T cells [no cells], for each condition (that is, [removal of γδ] or [no removal of γδ]). Flow cytometry histograms show granulysin expression in the S1 and JT cell lines before (T0) and after 6 hours (T6hr) of coculture with trophozoite-stage parasites. Dotted lines represent isotype control antibody. (B) Purified merozoites were incubated with fresh uiRBCs alone (no cells) or in the presence of S1 or JT T cells or the αβ T4A.5 T-cell clone, and the parasitemia was assessed after 28 hours. (i) Schematic representation of the experimental design. (ii) Inhibition of merozoite reinvasion (percentage) was calculated as 100 − [(average % parasitemia with cells/average % parasitemia without cells) × 100]. Data represent the mean ± SD of the inhibition of merozoite invasion observed in 3 independent experiments performed in duplicate (n = 3; *P ≤ .05 by Mann-Whitney rank sum test comparing S1 or JT with T4A.5). (iii) Parasitemia from 1 representative experiment is shown (mean ± SD; *P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia in the presence of T cells [S1, JT, or T4A.5] with the parasitemia in absence of T cells [no cells]).
Together, these data suggest that Vγ9Vδ2 T-cell antiparasitic activity targets merozoites. To demonstrate targeting of the merozoites, we performed a merozoite invasion assay in the presence of the γδ T-cell lines. Invasive merozoites (prepared as described in “Methods” and supplemental Figure 7) were incubated with Vγ9Vδ2 T-cell lines or with the αβ T-cell clone T4A.5 for 28 hours, after which parasitemia was measured (Figure 5Bi). Both the S1 and JT lines inhibited merozoite reinvasion, whereas the T4A.5 clone did not (Figure 5Bi-ii). In addition, short-term Vγ9Vδ2 T-cells lines displayed an inhibition of merozoite invasion ranging from 30% to 60% (supplemental Table 1). Taken together, these data show that the intraerythrocytic-stage (trophozoite/schizont) parasites are insensitive to the Vγ9Vδ2 T-cell granulysin-mediated cytotoxic machinery and that the invasive extracellular stage merozoites are the only targets vulnerable to Vγ9Vδ2 T-cell antiparasitic activity.
High frequency of granulysin-producing Vδ2 T cells in malaria patients
To investigate Vγ9Vδ2 T-cell granulysin-triggering during human infection, we first assessed the presence of granulysin in circulating γδ T cells. Intracytoplasmic granulysin was detected ex vivo in Vδ2 T cells from patients with acute P falciparum infection. The percentage of Vδ2 granulysin-positive cells was much higher in infected patients than in control donors (median, 48.9% vs 8.5%; P = .001), indicating that P falciparum infection primed Vγ9Vδ2 T cells to produce granulysin (Figure 6A). To confirm the primed status of Vδ2 cells in vivo, we examined the expression of cell surface markers specific for different effector/memory subpopulations.32 The ratio of Vδ2 T cells exhibiting an effector memory (ie, TEM:CD27−CD45RA−) versus a central memory (ie, TCM:CD27+CD45RA−) phenotype was reversed in infected patients compared with that of healthy controls (Figure 6Bi-ii). Furthermore, the total proportion of effector cells, including TEM:CD27−CD45RA− and TEMRA:CD27−CD45RA+ cells, was higher in infected patients compared with controls (65.7 ± 14.3 vs 26.5 ± 10.9; P = .001). Granulysin plasma levels were higher in malaria patients (n = 12) than in healthy controls (n = 13; median, 95.6 vs 25.3 ng/mL; P = .00001; Figure 6Ci) and correlated positively with the percentage of Vδ2 T cells (Spearman rho = 0.785, P = .036; Figure 6Cii). This suggests that Vδ2 T cells are an important source of plasma granulysin. For 2 patients (P1 and P2), we could measure the in vitro antiparasitic potential of the circulating Vδ2 cells. We performed a CD107a assay with PBMCs from these patients and observed that a significant proportion of Vδ2+ cells degranulated under schizont stimulation (14.3% for P1 and 10.7% for P2), whereas uiRBCs induced only minimal expression of CD107a (Figure 6D). Of note, Vδ2− T cells did not express significant levels of CD107a under the same conditions, highlighting the specific involvement of Vδ2 T cells in parasite-triggered degranulation. Together, these data demonstrate that Vδ2 T-cell activation in vivo is associated with granulysin expression, which enables the cells to contribute to the control of parasitemia through a granulysin-dependent mechanism.
Granulysin and Vδ2+ T-cell phenotype in primary-infected patients. (A) PBMCs from P falciparum primary-infected patients and healthy donors were stained ex vivo for intracellular granulysin and effector/memory surface markers. (i) Representative flow cytometry dot-plot outlining the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Flow cytometry histograms showing granulysin expression in Vδ2+ gated T cells (black line) compared with isotype control antibody (dotted line) in a representative patient and healthy donor (control). The percentage of positive cells for granulysin intracellular staining is indicated in the top right corner of each panel. (ii) Percentages of CD3+Vδ2+ cells positive for granulysin in malaria patients and healthy donors (controls). The box represents the 75th and 25th percentiles, and the bar represents the median. P value was determined using Mann-Whitney rank sum test to compare patients (n = 7) with controls (n = 10). Data were obtained by collecting 300 000 total events. (Bi) Representative example of flow cytometry data showing the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Expression of the CD27 and CD45RA cell surface markers in the gated Vδ2+ T cells define distinct effector/memory subpopulations (TNAIVE, TCM, TEM, and TEMRA). (ii) Data represent the mean ± SD of the percentage of Vδ2+ T cells of each effector/memory subset from patients or controls (*P ≤ .05 by Mann-Whitney rank sum test comparing patients [n = 6] with controls [n = 10]). Data were obtained by collecting 300 000 total events. (Ci) Plasma granulysin levels in patients and controls (i) were detected by ELISA. Box represents the 75th and 25th percentiles, and the bar represents the median. The P value was determined using Mann-Whitney rank sum test to compare patients (n = 12) with controls (n = 13). (ii) Log-transformed levels of plasma granulysin plotted against the percentage of CD3+ T cells expressing Vδ2 in patients. Statistical analysis was performed using Spearman rank correlation test, and the ρ and the P value are indicated (n = 7). (D) Fresh PBMCs from 2 patients (P1 and P2) were cocultured with purified trophozoites (iRBCs) or uiRBCs at a 1/5 E/T ratio. CD107a surface expression detected after 6 hours of coculture was measured. The percentage of CD3+Vδ2+ T cells or CD3+Vδ2− T cells expressing CD107a is shown. Data were obtained by collecting 300 000 total events.
Granulysin and Vδ2+ T-cell phenotype in primary-infected patients. (A) PBMCs from P falciparum primary-infected patients and healthy donors were stained ex vivo for intracellular granulysin and effector/memory surface markers. (i) Representative flow cytometry dot-plot outlining the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Flow cytometry histograms showing granulysin expression in Vδ2+ gated T cells (black line) compared with isotype control antibody (dotted line) in a representative patient and healthy donor (control). The percentage of positive cells for granulysin intracellular staining is indicated in the top right corner of each panel. (ii) Percentages of CD3+Vδ2+ cells positive for granulysin in malaria patients and healthy donors (controls). The box represents the 75th and 25th percentiles, and the bar represents the median. P value was determined using Mann-Whitney rank sum test to compare patients (n = 7) with controls (n = 10). Data were obtained by collecting 300 000 total events. (Bi) Representative example of flow cytometry data showing the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Expression of the CD27 and CD45RA cell surface markers in the gated Vδ2+ T cells define distinct effector/memory subpopulations (TNAIVE, TCM, TEM, and TEMRA). (ii) Data represent the mean ± SD of the percentage of Vδ2+ T cells of each effector/memory subset from patients or controls (*P ≤ .05 by Mann-Whitney rank sum test comparing patients [n = 6] with controls [n = 10]). Data were obtained by collecting 300 000 total events. (Ci) Plasma granulysin levels in patients and controls (i) were detected by ELISA. Box represents the 75th and 25th percentiles, and the bar represents the median. The P value was determined using Mann-Whitney rank sum test to compare patients (n = 12) with controls (n = 13). (ii) Log-transformed levels of plasma granulysin plotted against the percentage of CD3+ T cells expressing Vδ2 in patients. Statistical analysis was performed using Spearman rank correlation test, and the ρ and the P value are indicated (n = 7). (D) Fresh PBMCs from 2 patients (P1 and P2) were cocultured with purified trophozoites (iRBCs) or uiRBCs at a 1/5 E/T ratio. CD107a surface expression detected after 6 hours of coculture was measured. The percentage of CD3+Vδ2+ T cells or CD3+Vδ2− T cells expressing CD107a is shown. Data were obtained by collecting 300 000 total events.
Discussion
Human immune effector mechanisms able to promptly and swiftly limit parasite blood-stage multiplication remain largely unknown. Here, we confirm and elucidate the antiplasmodial activity of human Vγ9Vδ2 T cells, an innate-like lymphocyte subset. We show in vitro that (1) activated γδ T cells contribute to PBMCs' parasite growth inhibition; (2) γδ T-cell lines inhibit parasite growth; (3) granulysin, but not perforin, is essential for this antiparasitic activity; (4) both the intraerythrocytic parasitic stages and the extracellular free merozoites trigger TCR-specific Vγ9Vδ2 activation, degranulation, and granulysin release; and (5) the vulnerable target of Vγ9Vδ2 T cells is the extracellular merozoite. Finally we provide ex vivo data showing that during a primary P falciparum infection, circulating Vγ9Vδ2 T cells express granulysin and degranulate when they encounter P falciparum parasites. Altogether, this work demonstrates that the extracellular merozoite is an activator and a target of unconventional cytotoxic T cells and provides strong indication for a direct contribution of Vγ9Vδ2 T cells in the early control of parasite density.
In vitro inhibition of P falciparum growth by Vγ9Vδ2 T cells required degranulation and contact between γδ T cells and parasites, confirming previous observations.26 The short-term degranulation assay used here, allowed us to show for the first time that intact live P falciparum blood stages either intracellular (P falciparum–infected RBCs) or extracellular (merozoites) may directly trigger γδ T-cell activation through a γδ TCR-dependent mechanism without intervention from accessory cells. These 2 stages contain deoxy-xylulose-5-phosphate phosphoantigen metabolites known to stimulate Vγ9Vδ2 T cells33 ; however, thus far, they have only been shown to stimulate γδ T cells as lysates or semipurified extracts6,34,35 or in the presence of accessory cells.25,36 The data presented here provide a new model for the identification of molecular mechanisms involved in the still enigmatic activation process of Vγ9Vδ2 T cells by eukaryotic microorganisms.
Perforin and granulysin have been implicated in the antimicrobial activity of γδ T cells. Granulysin is a positively charged cytolytic protein that can be detected in T- and NK-cell granules in humans and has no equivalent in mice.37 It displays antimicrobial activity against different microorganisms, including bacteria, fungi, and parasites.28 Killing of intracellular microorganisms by granulysin has been shown to be dependent on perforin29,30 ; perforin allows granulysin to penetrate host membranes in a manner similar to granzymes, leaving the cell intact.38 In contrast, perforin is not required to kill extracellular bacteria,29 since granulysin is sufficient to cause lysis.39 The generation of granulysin-silenced and perforin-deficient Vγ9Vδ2 T-cell lines provided us with powerful tools to investigate the relative contribution of these molecules to the antiparasitic activity. Granulysin-silencing reduced antiplasmodial activity dramatically, demonstrating that granulysin is required for the antiplasmodial activity of γδ T cells in vitro. The essential role of granulysin in this process is further supported by previous reports that showed that anti-granulysin antibodies abolished γδ T-cell inhibitory activity.26 In contrast, perforin seems to play a minor role in antiparasitic activity, including against the intracellular forms of P falciparum. Indeed, although trophozoites and schizonts specifically triggered degranulation and granulysin release, their intracellular development was not impaired when cocultured with Vγ9Vδ2 T cells. Because the erythrocytic membrane is resistant to granulysin,40 perforin does not seem to be sufficient to allow granulysin to pass this barrier and reach the intravacuolar parasite. Remaining protected from cytotoxic molecules within the erythrocyte for the duration of the intracellular development can be viewed as a Plasmodium evasion strategy that has not been appreciated previously. In contrast, the extracellular merozoite comes in direct contact with cytotoxic molecules such as granulysin, which impairs its invasiveness for RBCs and thereby decreases parasitemia. How granulysin reduces P falciparum merozoite infectivity remains unclear. Granulysin induces osmotic lysis of bacteria by altering membrane permeability.39 In eukaryotic tumor cells, granulysin destabilizes membrane integrity through its positive charges, causing a rapid increase in cytoplasmic calcium that leads to apoptosis.41 The merozoite membrane differs both from the outer wall/membrane of bacteria and from the classic eukaryotic membrane bilayer,42 and further investigation is required to elucidate the molecular mechanisms by which granulysin damages merozoites.
High plasma levels of granulysin and a high frequency of circulating Vγ9Vδ2 T cells containing granulysin were detected in P falciparum–infected patients, further indicating that natural infection primes Vγ9Vδ2 T cells for granulysin production. The positive correlation between the plasmatic granulysin concentration and the frequency of Vγ9Vδ2 T cells suggests that this subset might be an important contributor to the circulating granulysin in malaria patients. This conclusion is supported by the observation that Vγ9Vδ2 T cells were the only T-lymphocyte population triggered by P falciparum–infected RBCs to degranulate. Further studies are required to investigate whether granulysin expression correlates with in vivo control of parasite density and protection against severe malaria. Because perforin has been involved in experimental malaria pathology,43 it will be of interest to examine whether perforin and granulysin expression are parallel or diverge depending on the malaria clinical form, as has been shown in leprosy patients.44
An intriguing question raised by our data is how and where do activated effector Vγ9Vδ2 T cells target extracellular merozoites? Although binding of γδ T cells with merozoites could be observed in vitro, it is not clear whether this leads to a contact-oriented granule release. Even if this does not occur, it is possible that γδ T cells degranulate toward schizonts, creating a locally enriched granulysin environment into which merozoites are released. Although not required for antiparasitic activity, perforin might favor the egress of merozoites similarly to the recently described falciparum–perforin-like protein45 and thus promote a targeted action of granulysin on egressing merozoites. Further studies are required to address this point.
A plausible in vivo scenario is that sequestration of trophozoites and schizonts into microvessels creates a local inflammatory environment, eliciting the recruitment of primed Vγ9Vδ2 T cells. This could constitute a favorable niche for direct contact between infected RBCs and γδ T cells, leading to granulysin release and targeting of merozoites. These events may occur along the microvessel endothelial cells of deep organs or in the red pulp of the spleen, the site of P falciparum–infected RBC retention and γδ T-cell accumulation during malaria infection.46,47 Recent data from studies of patients with Stevens-Johnson syndrome have highlighted massive concentrations of granulysin in blisters (up to 10 000 ng/mL), suggesting that high granulysin concentrations compatible with toxic activity may be achieved in confined surroundings.22 In addition to its direct cytotoxic role, granulysin may exacerbate local inflammation and indirectly promote parasite clearance through its chemotactic activity for myeloid cells and its proinflammatory properties.48
The present work identified the RBC-invasive merozoite as a novel activator and target for unconventional cytotoxic T cells and adds Vγ9Vδ2 T cell–mediated granulysin release to the list of effector mechanisms operating in concert at early points in P falciparum infection. In addition, our data extend to malaria—a blood-perpetuating infection—the indications for γδ T cell–based immunotherapy, which have yielded encouraging results in the treatment of hematologic malignancies.49
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the cytometry core facility and the vectorology platform (Bordeaux University), S. Netzer, M. Taillepierre, and J. Dallennes for technical assistance. They are grateful to G. Milon, L. Couzi, and M. Mamani-Matsuda for valuable discussions.
This study was funded by Center National de la Recherche Scientifique (Unité Mixte de Recherche 5164), Ministère de la Défense (DGA-AGENPPAL n°07co401), Region Aquitaine, Fondation pour la Recherche Médicale, the European Community's 6th Framework Program (BioMalPar Network of Excellence grant LSHP-CT-2004-503578), and 7th Framework Program (EVIMALAR FP7/2007-242095). G.C. is a fellow of the MalParTraining FP6-Marie Curie Action (MEST-CT-2005-020492).
Authorship
Contribution: G.C. performed experiments, analyzed data, and wrote the manuscript; S.L., M.G., and I.M. performed experiments, analyzed data, or both; F.H., G.d.S.-B., and V.P. provided vital reagents used in this work; J.D.-M., J.-F.M., and M.T.-B. reviewed the manuscript and provided critical discussion; O.M.-P. reviewed the manuscript, provided critical discussion, and secured funding; and C.B. supervised the entire project, designed research, wrote the manuscript, and secured funding.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Charlotte Behr, CNRS UMR 5164, Université de Bordeaux Segalen, 146 rue Léo Saignat, 33076 Bordeaux Cedex, France; e-mail: charlotte.behr@u-bordeaux2.fr.

![Figure 2. Perforin is dispensable for Vγ9Vδ2 antiparasitic activity. A Vγ9Vδ2 T-cell line was generated from a perforin-deficient familial hemophagocytic lymphohistiocytosis (FLH) patient, and its antiparasitic activity was assessed in a standard parasite inhibition assay. (A) Flow cytometry histograms showing perforin and granulysin expression in Vγ9Vδ2 T-cell lines generated from 2 different donors (S1 and JT) and from an FLH patient (PFNdef). Mean fluorescence intensity (MFI) for perforin and granulysin intracellular staining is indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (B) Comparison of the antiparasitic activity of the PFNdef, S1 and JT cell lines. The αβ T4A.5 T-cell clone was used as a negative control. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 4 independent experiments (n = 4; *P ≤ .05 by Mann-Whitney rank sum test comparing the PFNdef cell line with the S1, JT, or T4A.5 T-cell lines).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/118/26/10.1182_blood-2011-08-376111/4/m_zh89991183620002.jpeg?Expires=1767698515&Signature=u2ntCj2jER3F9pCcv1USCZPNF6evsZRADwaUxQ6Ostjhf~yik1cnT39AwoR6e466GDdRSGi4XyHXValgju6U7gHEThC3rQlAnaKfNLJ8Cmu-ANXsc9E-lmlrV-rJYp6Z1Ht3i~qez2n1BrRq66oo6EGSMaLAPl1XjM0S4cVZQAns02MvMX4qC-w4R3Z~t4Kxcz3h~sB5b4d1puDOXuEuVclb~RTNx4038LBuOXjZjEl2L~sluCmWgtobKWxID~2GSurP733F~w6O0Eow8paepXY2Qox4whvdCxq8L6~PVDZ12~BOp8z5euQ71sq409km2euoACGemt7to2ji~SuUyQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 3. Granulysin is essential for Vγ9Vδ2 antiparasitic activity. The S1 T-cell line was infected with the lentiviral vector containing the granulysin-specific shRNA sequences GNLYsh1, GNLYsh2, or a NS shRNA sequence, and their antiparasitic activity has been assessed in a standard parasite inhibition assay. (A) RT-PCR assessment of granulysin mRNA levels in the noninfected S1 cell line (Ctrl) or S1 cell line infected with NS, GNLYsh1 (Gnly1), or GNLYsh2 (Gnly2) shRNA constructs. β2-Microglobulin mRNA levels were measured as a control. (B) Granulysin and perforin protein levels were detected in S1 (Ctrl), NS, Gnly1, and Gnly2 cell lines by Western blotting. Actin expression was measured as a loading control. (C) Intracellular granulysin expression was measured using flow cytometry in the NS, Gnly1, and Gnly2 cell lines. The percentage of granulysin-positive cells and the MFI of granulysin intracellular staining are indicated in the top right corner of each panel. Dotted lines represent isotype control antibody. (D) Antiparasitic activity of the NS, Gnly1, and Gnly2 cell lines. Antiparasitic activity (percentage) was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represent the mean ± SD of 2 independent experiments (n = 2; *P ≤ .05 by Mann-Whitney rank sum test comparing NS with Gnly1 and Gnly2 T-cell lines).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/118/26/10.1182_blood-2011-08-376111/4/m_zh89991183620003.jpeg?Expires=1767698515&Signature=wzOIklVYBwBDL1RXGZ0fjdOGVpj8Wo6xjcRyp1WGROLNRdktJSlmF-Fr2ZCr4sXmNLx-F8YxmNbdTDZm6XtQKyYsxDi-EWLkmhAMEgZ4pXj4ETwU9MEy0Srst~AiBbWTMA5oMDm4uckuVQeBUq1Xon4RRM1T-5LTQ8OC8ii5QH70qyVk1~jBvA9-MLH1TgrnKlwywR085yp8rImKI8PVY~AM~VHQ8eooQYjyn61P8Yy2E-8cVLMKid-ECYx8FedU036fiL~Kcns43yAXo90D5cCSWzqDMIQ03DO4N-84vMy3wy~eV2Mbpj1D0jIsPpEq4wzvJ7X4kb41o-wEIIu0xw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. Merozoites, not trophozoites, are the target of Vγ9Vδ2 antiparasitic activity. (A) Primed S1 or JT Vγ9Vδ2 T cells were cocultured with purified trophozoites (E/T ratio 4/1) for either 24 hours until merozoite reinvasion (no removal of γδ) or were removed by magnetic depletion after 6 hours of coculture, just before schizont rupture; [removal of γδ(T6h)]. Mock-treated parasites cultured without cells were used as a control. After cell removal, the parasitemia was similar under the various conditions. (i) Schematic representation of the experimental design. (ii) Antiparasitic activity was calculated as 100 − [(average % parasitemia of duplicate with cells in the presence of IL-2 + IL-15/average % parasitemia of duplicate with cells in the presence of IL-2) × 100]. Data represents the mean ± SD of the antiparasitic activity observed in 3 independent experiments performed in duplicate (*P ≤ .05 for Mann-Whitney rank sum test comparing the conditions [removal of γδ] and [no removal of γδ] for each T-cell line). (iii) Histograms represent the mean of parasitemia ± SD observed in 1 representative experiment performed in duplicate with the S1 and the JT cell lines. No cells: parasites cultured in the absence of cells (*P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia of parasites cultured in the presence of T cells [S1 or JT] with the parasitemia in absence of T cells [no cells], for each condition (that is, [removal of γδ] or [no removal of γδ]). Flow cytometry histograms show granulysin expression in the S1 and JT cell lines before (T0) and after 6 hours (T6hr) of coculture with trophozoite-stage parasites. Dotted lines represent isotype control antibody. (B) Purified merozoites were incubated with fresh uiRBCs alone (no cells) or in the presence of S1 or JT T cells or the αβ T4A.5 T-cell clone, and the parasitemia was assessed after 28 hours. (i) Schematic representation of the experimental design. (ii) Inhibition of merozoite reinvasion (percentage) was calculated as 100 − [(average % parasitemia with cells/average % parasitemia without cells) × 100]. Data represent the mean ± SD of the inhibition of merozoite invasion observed in 3 independent experiments performed in duplicate (n = 3; *P ≤ .05 by Mann-Whitney rank sum test comparing S1 or JT with T4A.5). (iii) Parasitemia from 1 representative experiment is shown (mean ± SD; *P ≤ .05 by Mann-Whitney rank sum test comparing the parasitemia in the presence of T cells [S1, JT, or T4A.5] with the parasitemia in absence of T cells [no cells]).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/118/26/10.1182_blood-2011-08-376111/4/m_zh89991183620005.jpeg?Expires=1767698515&Signature=XsIUhj0IRRmRvpDiZU49MBT8Lr3KQm-6L8hh4PL4I~GrCFFxi81y9Cj5dSHe9PGq2eHh9w9wM3ONb~zP5zaPvOJafgQGXv1lTPuJJMFxRZSh8icZ7p96LiFTOgCnBAxVdn9htTMNl9~Wcngl~ZqhNI7J8yknP-C0NTnst9WrRh3YEnbNfP5dHA14OLy3Kwds75haq6JQPRWduMBxfRFAxeBzJSVGU-Eo2vTVtjykMhIkT2cSCdPLotHgFlnBQQbqqd-47tPfOylB5g5FErehyEc4L23AN2YizAOEMNpr~z5b241v~9F7v2obec97kxh-b2V3LO9xniIxwg-bgTpL0g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 6. Granulysin and Vδ2+ T-cell phenotype in primary-infected patients. (A) PBMCs from P falciparum primary-infected patients and healthy donors were stained ex vivo for intracellular granulysin and effector/memory surface markers. (i) Representative flow cytometry dot-plot outlining the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Flow cytometry histograms showing granulysin expression in Vδ2+ gated T cells (black line) compared with isotype control antibody (dotted line) in a representative patient and healthy donor (control). The percentage of positive cells for granulysin intracellular staining is indicated in the top right corner of each panel. (ii) Percentages of CD3+Vδ2+ cells positive for granulysin in malaria patients and healthy donors (controls). The box represents the 75th and 25th percentiles, and the bar represents the median. P value was determined using Mann-Whitney rank sum test to compare patients (n = 7) with controls (n = 10). Data were obtained by collecting 300 000 total events. (Bi) Representative example of flow cytometry data showing the gating strategy for Vδ2+ T cells (CD3+Vδ2+ lymphocytes). Expression of the CD27 and CD45RA cell surface markers in the gated Vδ2+ T cells define distinct effector/memory subpopulations (TNAIVE, TCM, TEM, and TEMRA). (ii) Data represent the mean ± SD of the percentage of Vδ2+ T cells of each effector/memory subset from patients or controls (*P ≤ .05 by Mann-Whitney rank sum test comparing patients [n = 6] with controls [n = 10]). Data were obtained by collecting 300 000 total events. (Ci) Plasma granulysin levels in patients and controls (i) were detected by ELISA. Box represents the 75th and 25th percentiles, and the bar represents the median. The P value was determined using Mann-Whitney rank sum test to compare patients (n = 12) with controls (n = 13). (ii) Log-transformed levels of plasma granulysin plotted against the percentage of CD3+ T cells expressing Vδ2 in patients. Statistical analysis was performed using Spearman rank correlation test, and the ρ and the P value are indicated (n = 7). (D) Fresh PBMCs from 2 patients (P1 and P2) were cocultured with purified trophozoites (iRBCs) or uiRBCs at a 1/5 E/T ratio. CD107a surface expression detected after 6 hours of coculture was measured. The percentage of CD3+Vδ2+ T cells or CD3+Vδ2− T cells expressing CD107a is shown. Data were obtained by collecting 300 000 total events.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/118/26/10.1182_blood-2011-08-376111/4/m_zh89991183620006.jpeg?Expires=1767698515&Signature=mR6mBd8zmwHjtg1y-7YMGD27DciUAw44IGh4Y9znEP18unLujdX4tviQvfHrxRV8uozZ~qXIUXXhU1VwxoNlkpI4KKxlg7v5Mnhp4E5LchyI3154ecGhp9V6s-iPRk4NFBT4w-08BtchQL863Emd0esDIHh9PiOnXjVuo6VS7TcFNbFbaXsxlO2dp8bzIaqSYAHlVbxXicwG9jEI6A3ENUlFBtYOHkQ6Db5rnOrSXDZ4ASlU9UATh~BhmM0zkjj-59IwjCb2lOH3FlsehvK89fJw05dOEyZQZ70vUHUFV5L9THu~wYVgNtuoOgqVhxiTTtJZIMLQNvA77eVszFbT6g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal