Abstract
Multiple mechanisms operate to ensure T-cell tolerance toward self-antigens. Three main processes have been described: clonal deletion, anergy, and deviation to CD4+ regulatory T cells (Tregs) that suppress autoreactive T cells that have escaped the first 2 mechanisms. Although it is accepted that dendritic cells (DCs) and B cells contribute in maintaining T-cell tolerance to self-antigens, their relative contribution and the processes involved under physiologic conditions remain only partially characterized. In this study, we used different transgenic mouse models to obtain chimeras where a neo self-antigen is expressed by thymic epithelium and/or by DCs or B cells. We found that expression of cognate ligand in the thymus enhances antigen-specific FoxP3+ cells independently of whether the self-antigen is expressed on thymic epithelium or only on DCs, but not on B cells. On the contrary, self-antigen expression by B cells was very efficient in inducing FoxP3+ cells in the periphery, whereas self-antigen expression by DC led mainly to deletion and anergy of antigen-specific FoxP3− cells. The results presented in this study underline the role of B cells in Treg induction and may have important implications in clinical protocols aimed at the peripheral expansion of Tregs in patients.
Introduction
T-cell tolerance toward self-antigens is achieved through a series of mechanisms that have evolved to keep autoimmunity in check. Three main processes, which start in the thymus but continue in the periphery, have been described: clonal deletion of cells reactive to proteins present in the thymus, including peripheral tissue antigens expressed by thymic epithelial cells and blood-borne antigens; anergy induction as a result of antigen recognition under noncostimulatory or inhibitory conditions that remain only partially understood; and the generation of regulatory T cells (Tregs) that further limit peripheral reactivity toward self. The relative contribution of each of these mechanisms to the maintenance of T-cell tolerance has been subject of some debate.1 However, it is clear that the breakdown of any of these mechanisms, which start in the thymus and continue in the periphery, can lead to the development of autoimmune disease, even though the kinetics, severity, and target organs may be different. Thus, the generation and maintenance of FoxP3+ Tregs have been shown to be critical in avoiding severe lymphoproliferative disease and extensive multiorgan infiltration throughout the entire life span of the organism.2 Similarly, mice deficient for Fas or Fas ligand, and thus incapable of efficiently deleting T cells in the periphery, develop lymphoproliferation and generalized autoimmunity,3,4 although apoptosis has been reported to be dispensable in T-cell tolerance induction to a systemic self-antigen.5 Recently, E3 ubiquitin ligases, such as Cbl-b, Itch, Grail, and TRAF6, have been implicated in the development and maintenance of T-cell anergy, and mice deficient for these genes display resistance to anergy induction6,7 and enhanced susceptibility to spontaneous8,9 and induced10,11 autoimmune diseases. However, some genes typically expressed by anergic cells are also expressed by Tregs,12 and it has been difficult to dissociate anergy induction from Treg induction in vivo and determine their relative contribution in the establishment of self-tolerance.
Tolerance induction to target antigens may represent a therapeutic strategy in the treatment of autoimmune diseases and allergy. Thus, it is important to understand the conditions by which these different processes occur and, in particular, the role of the different populations of antigen-presenting cells in tolerance induction (regulatory cell induction vs anergy vs deletion). The critical role of dendritic cells (DCs) not only in the induction of efficient immune responses but also in the maintenance of T-cell tolerance, via the cross-presentation of tissue-restricted self-antigens and their transport to the lymph nodes under steady-state conditions, has been well documented.13 A large body of recent experimental data suggest that antigen presentation by DCs under noninflammatory conditions leads to the generation or expansion of Tregs,14,15 although the exact mechanisms involved remain only partially understood.
B cells are considered to be poorly immunogenic antigen-presenting cells, and it was reported that animals can be rendered tolerant to antigens presented by naive B cells.16 More recent studies show that B cells can positively or negatively regulate T cell-mediated responses through antibody-independent mechanisms and modulate the development, proliferation, and survival of Tregs.17 Indeed, B cells can efficiently generate Tregs in vitro18-20 but, on the other hand, they were reported to induce deletion of self-reactive T cells in vivo.21 Thus, the role of B cells in induction of T-cell tolerance to self-antigens under physiologic conditions, and in particular, in the induction of Tregs, remains poorly defined.
In this study, we sought to determine the role of DCs and B cells in the induction of T-cell tolerance toward a neo–self-antigen in vivo. We show that antigen presentation by these 2 different cell types results in distinct types of tolerance. Presentation by DCs favors deletion and anergy, whereas presentation by B cells leads to peripheral Treg induction.
Methods
Mice
Balb/c (H-2d) mice were from Charles River Laboratories. TCR-HA transgenic mice expressing a T-cell receptor-αβ (TCRαβ) specific for peptide 111–119 from influenza virus hemagglutinin (HA) presented by I-Ed have been previously described22 and are on the Balb/c background. These mice were crossed with mice expressing influenza HA under the control of the ubiquitous pgk promoter to generate TCR-HAxpgk-HA double-transgenic mice23 or to mice expressing influenza HA under the control of the Igk L chain promoter and enhancer to generate TCR-HAxIg-HA mice.23 FoxP3-GFP knock-in mice (C.Cg-Foxp3tm2Tch/J) were purchased from The Jackson Laboratory and backcrossed onto the TCR-HAxIg-HA and TCR-HAxpgk-HA mice. Ig-HA mice were also backcrossed onto Rag−/− Balb/c mice. All mice were used between 6 and 10 weeks of age. Procedures involving animals and their care conformed to institutional guidelines (authorization no. 11/2006-A from the Italian Ministry of Health) in compliance with national (4D.L. N.116, GU, suppl 40, 18-2-1992) and international law and policies.24 All efforts were made to minimize the number of animals used and their suffering.
Antibodies and reagents
The clonotypic 6.5 monoclonal antibody, which recognizes the transgenic TCR-HA, was produced in our laboratory and was used coupled to biotin or phycoerythrin. All other antibodies for flow cytometry were purchased from BD Biosciences PharMingen. The polyclonal Ki67 monoclonal antibody was purchased from Abcam. Cells were analyzed on a flow cytometer (FACSCanto; BD Biosciences). Cell sorting was performed using a FACSAria (BD Biosciences). FACS data were analyzed using Diva software and FlowJo software version 7.2.5. The HA peptide (SVSSFERFEIFPK) was purchased from Invitrogen. Vybrant CFDA-SE cell tracer kit (Invitrogen) and CellVue Maroon (Molecular Targeting Technologies) were used according to the manufacturer's instructions.
In vitro proliferation and suppression assays
For in vitro experiments, total lymph node and spleen suspensions from the different transgenic or chimeric mice were stained with CD4 and 6.5 antibodies and sorted on a FACSAria to obtain HA-specific 6.5+ T conventional (Tc; CD4+ 6.5+ GFP−) or 6.5+ Tregs (CD4+ 6.5+ GFP+) cells, respectively. DCs were obtained from the spleen of Balb/c mice by positive selection with anti-CD11c microbeads (Miltenyi Biotec). All assays were performed in complete Dulbecco modified Eagle medium (Lonza), supplemented with 2-mercaptoethanol (Invitrogen) and 10% FCS. A total of .5 × 104 Tc cells were incubated with DCs (1.5 × 104) in flat-bottom 96-well plates in the absence or presence of Tregs at a Tc/Treg ratio of 1:1 or 2:1. After 2 days of culture, supernatants were collected for the quantification of cytokines, and 1 μCi 3H-methylthymidine was added for an additional 16 hours. All conditions were performed in triplicates. Some experiments were performed staining T cells with CellVue Maroon, and the proliferation was analyzed by flow cytometry after 3 days of coculture. For experiments shown in Figure 3A, spleen cell suspensions were obtained by collagenase digestion, stained with CD11c and CD19 antibodies, and sorted electronically. They were then cocultured in vitro with CD4+6.5+ T cells from TCR-HA single transgenic mice.
Bone marrow chimeras
pgk-HA or Balb/c recipient mice were irradiated 700 cGy and reconstituted with bone marrow obtained from TCR-HA FoxP3-GFP mice (2 × 106 cells), together with an equal amount of bone marrow from Rag−/−, Rag−/− Ig-HA mice or 0.5 to 0.7 × 106 CD19+ cells sorted from the bone marrow of an Ig-HA mouse. Mice were kept on antibiotics for 2 weeks after transfer. Reconstitution was confirmed after 7 weeks, and mice were analyzed between 8 and 12 weeks after transfer. In all chimeric mice, the percentage of B cells in the spleen was comparable at the time of analysis (71.8% ± 1.6%).
Adoptive transfer experiments
CFSE-labeled CD4+6.5+ T cells from a Thy1.1 TCR-HA mouse (1 × 106) were injected into pgk-HA, Ig-HA, or Balb/c recipients (Thy1.2). Some Balb/c recipients had been reconstituted 7 to 8 weeks earlier with pgk-HA bone marrow. Recipient mice were killed 3 days after adoptive transfer, and cell suspensions from lymph node and spleen were analyzed by flow cytometry.
Immunohistochemistry
Frozen spleen sections (10 μm) from the different chimeric mice were fixed with 4% formalin, rehydrated with PBS, and permeabilized with PBS/Tween 0.1%. Then the slides were incubated with the anti-FoxP3 Alexa647-conjugated (1:50; BD Biosciences) and with the primary antibody anti-CD19 (1:50; eBioscience) that was revealed with the Alexa488 anti–rat antibody (1:500; Invitrogen). After washes, nuclei were counterstained with Hoechst 33258 (1 μg/mL) and mounted with ProLong (Invitrogen). Negative controls included slides incubated with the secondary antibodies alone. Acquisition of images was made by confocal microscopy Fluoview FV1000 (Olympus) with an oil immersion objective (60 × 1.4 NA Plan-Apochromat; Olympus). Images were processed using Adobe Photoshop 9.0.2. The statistical analysis was performed using Student unpaired 2-tailed t test, ANOVA 1-way test analysis with Tukey Multiple Comparison Test. For each specimen, Foxp3+ cells were counted in randomly selected CD19 positive follicles at 20× magnification. Values are expressed as mean ± SE.
Statistical analysis
Results are expressed as mean ± SD. Student t test was performed where indicated.
Results
The pattern of self-antigen expression determines the fate of antigen-specific T cells
Although it is well established that Treg selection is positively regulated by expression of the agonist ligand in the thymus,25,26 Tregs can also be generated in periphery,27 through processes that are not fully understood. Here, we took advantage of 2 mouse models-pgk-HA and Ig-HA mice-expressing the neo–self-antigen HA in the thymus. The pgk-HA mouse expresses HA on thymic epithelium, although expression on other cell types in periphery has not been explored. The Ig promoter in Ig-HA mice drives expression of HA in B cells,28 but also in DCs29 and thymic epithelium.26 These 2 different transgenic mice were backcrossed onto mice expressing a transgenic TCR (recognizable by the clonotypic antibody 6.5) specific for the immunodominant peptide of HA in the context of IEd molecules. In addition, in this study, all transgenic mice were on a FoxP3-EGFP background, to identify and isolate FoxP3+ cells by GFP expression.
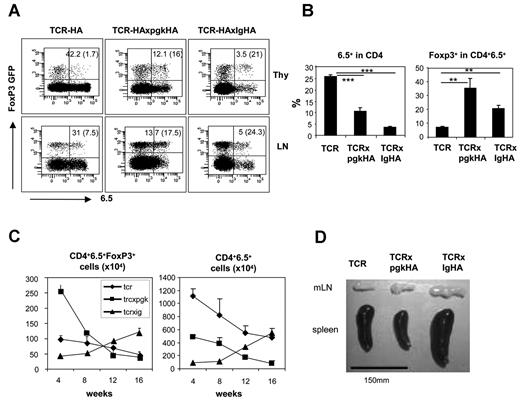
Both TCR-HAxpgk-HA and TCR-HAxIg-HA mice, despite thymic deletion of HA-specific T cells because of negative selection, are known to generate HA-specific Tregs.30 Indeed, compared with the TCR-HA single transgenic mouse, mice having thymic expression of HA showed enhanced selection of HA-specific FoxP3+ thymocytes (Figure 1A top row). This was also true for the periphery, where, despite the strong deletion of CD4+6.5+ cells observed for both types of double-transgenic mice (Figure 1A bottom row; Figure 1B left graph), the percentage of FoxP3+ cells among the 6.5+ population was significantly higher than in the single transgenic mice (Figure 1A bottom row; Figure 1B right graph). It is interesting to note that, in the periphery of single transgenic TCR-HA mice, there were more CD4+6.5+FoxP3+ cells in the periphery with respect to the thymus, suggesting either expansion of thymic-derived Tregs in periphery or their de novo generation, even in the absence of the cognate antigen. This is true both for the percentage of FoxP3+ cells among CD4+6.5+ cells, as observed in Figure 1 (thymus vs lymph nodes) and for the absolute numbers of CD4+6.5+FoxP3+ cells (8.37 ± 1.3 × 104 cells in the thymus vs 85.5 ± 30.7 × 104 cells in the lymph nodes plus spleen, reflecting an average 10-fold increase). Interestingly, when comparing absolute numbers of CD4+6.5+ cells in secondary lymphoid organs (lymph nodes and spleen) of the 3 types of mice, we observed an age-dependent accumulation in the number of FoxP3+6.5+ cells in TCR-HAxIg-HA mice (Figure 1C left graph). Indeed, the number of total CD4+6.5+ cells accumulated with age (Figure 1C right graph), and this increase was in great part because of a striking increase in total cellularity of secondary lymphoid organs of TCR-HAxIg-HA mice, clearly evident from the age of 12 weeks (Figure 1D). In contrast, this increase in total cellularity was not observed for TCR-HAxpgk-HA mice. Indeed, the absolute number of FoxP3+6.5+ and total CD4+6.5+ cells in TCR-HA single transgenic mice or TCR-HAxpgk-HA mice tended to decrease with age, independently of FoxP3 expression (Figure 1C) because the Tc/Treg ratio remained relatively constant with age (data not shown).
HA expression in thymus induces negative selection of HA-specific T cells and an increase in HA-specific FoxP3+ cells, but with a different age-dependent kinetics depending on expression of the HA transgene. (A) Primary and secondary lymphoid organs from 12-week-old TCR-HA, TCR-HAxpgk-Ha, and TCR-HAxIg-HA mice were analyzed for FoxP3 and 6.5 expression among gated CD4+ cells. Shown are representative dot plots, with the percentage of total 6.5+ cells among CD4+ cells (value outside the parentheses) and the percentage of FoxP3+ cells among CD4+6.5+ cells (value in parentheses). (B) The same data are presented for a pool of 12-week-old mice, with an average of 3 mice per time point. **P < 0.01. ***P < .001. (C) Absolute numbers of 6.5+FoxP3+ cells and of total 6.5+ cells in periphery (lymph nodes and spleen) of the 3 different types of mice vary with the age. Each time point represents 2 to 5 mice. (D) A representative image of the mesenteric lymph nodes (mLN) and spleen of a 16-week-old TCR-HA, TCR-HAxpgk-HA, and TCR-HAxIg-HA mouse.
HA expression in thymus induces negative selection of HA-specific T cells and an increase in HA-specific FoxP3+ cells, but with a different age-dependent kinetics depending on expression of the HA transgene. (A) Primary and secondary lymphoid organs from 12-week-old TCR-HA, TCR-HAxpgk-Ha, and TCR-HAxIg-HA mice were analyzed for FoxP3 and 6.5 expression among gated CD4+ cells. Shown are representative dot plots, with the percentage of total 6.5+ cells among CD4+ cells (value outside the parentheses) and the percentage of FoxP3+ cells among CD4+6.5+ cells (value in parentheses). (B) The same data are presented for a pool of 12-week-old mice, with an average of 3 mice per time point. **P < 0.01. ***P < .001. (C) Absolute numbers of 6.5+FoxP3+ cells and of total 6.5+ cells in periphery (lymph nodes and spleen) of the 3 different types of mice vary with the age. Each time point represents 2 to 5 mice. (D) A representative image of the mesenteric lymph nodes (mLN) and spleen of a 16-week-old TCR-HA, TCR-HAxpgk-HA, and TCR-HAxIg-HA mouse.
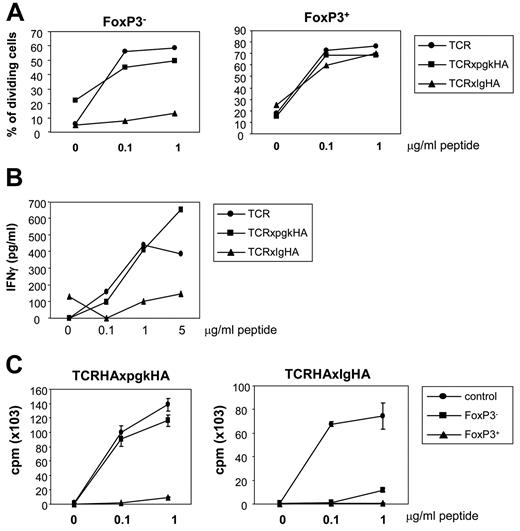
We then compared the functional properties of HA-specific FoxP3+ and FoxP3− cells obtained from these mice. By staining cells with a cell dye, we could determine by flow cytometry the division of CD4+6.5+FoxP3+ and FoxP3− cells in total lymph node cell preparations, when stimulated with different peptide doses in vitro. The 6.5+FoxP3+ cells generated in the 3 different mice were capable of proliferating at a comparable level because of exogenous interleukin-2 (IL-2) provided by the 6.5+FoxP3− cells present in the same well. In sharp contrast, 6.5+FoxP3− T cells from TCR-HAxIg-HA mice did not divide at any peptide dose (Figure 2A). Furthermore, very low interferon-γ levels were detected in the supernatant of TCR-HAxIg-HA cultures compared with those from TCR-HA and TCR-HAxpgk-HA mice (Figure 2B). These data strongly suggested that HA-specific conventional T cells were in a state of anergy in TCR-HAxIg-HA mice but they were functional in TCR-HAxpgk-HA mice. To understand whether this different proliferative capacity of FoxP3− cells was the result of differences in the suppressive capacity of their FoxP3+ counterparts, we sorted CD4+6.5+FoxP3− and FoxP3+ cells from both mice and stimulated them in vitro with the HA peptide. As shown in Figure 2C, FoxP3− cells from TCR-HAxpgk-HA mice proliferated similarly to control HA-specific T cells and, as expected, the FoxP3+ cells did not proliferate because of the absence of exogenous IL-2. In contrast, FoxP3− cells from TCR-HAxIg-HA mice were unable of responding in vitro to peptide stimulation, similar to their FoxP3+ counterparts (Figure 2C).
Different behavior of HA-specific FoxP3− cells in TCR-HAxpgk-Ha and TCR-HAxIg-HA mice. (A) Total lymph node suspensions from TCR-HA, TCR-HAxpgk-HA, or TCR-HAxIg-HA mice were stained with cell-vue Maroon and incubated in vitro with different peptide doses. Proliferation of CD4+6.5+FoxP3− and FoxP3+ cells was determined by flow cytometry. (B) Interferon-γ present in the supernatant from the same cultures was determined by enzyme-linked immunosorbent assay. Results correspond to the pool of triplicate wells, with cells obtained from one mouse of each genotype. Two independent experiments were performed with similar results. (C) CD4+6.5+FoxP3+ and FoxP3− cells from TCR-HAxpgk-HA (left graph) or TCR-HAxIg-HA (right graph) mice were electronically sorted and incubated in vitro with splenic-derived DCs and different peptide doses. FoxP3− cells from a TCR-HA single transgenic mouse were used as control of proliferation. Thymidine was added after 48 hours of culture and left for an additional 16 hours. Experiments were performed in triplicate and 1 representative experiment of 3 is shown.
Different behavior of HA-specific FoxP3− cells in TCR-HAxpgk-Ha and TCR-HAxIg-HA mice. (A) Total lymph node suspensions from TCR-HA, TCR-HAxpgk-HA, or TCR-HAxIg-HA mice were stained with cell-vue Maroon and incubated in vitro with different peptide doses. Proliferation of CD4+6.5+FoxP3− and FoxP3+ cells was determined by flow cytometry. (B) Interferon-γ present in the supernatant from the same cultures was determined by enzyme-linked immunosorbent assay. Results correspond to the pool of triplicate wells, with cells obtained from one mouse of each genotype. Two independent experiments were performed with similar results. (C) CD4+6.5+FoxP3+ and FoxP3− cells from TCR-HAxpgk-HA (left graph) or TCR-HAxIg-HA (right graph) mice were electronically sorted and incubated in vitro with splenic-derived DCs and different peptide doses. FoxP3− cells from a TCR-HA single transgenic mouse were used as control of proliferation. Thymidine was added after 48 hours of culture and left for an additional 16 hours. Experiments were performed in triplicate and 1 representative experiment of 3 is shown.
Overall, these data suggested that self-antigen-specific cells undergo a different fate depending on the pattern of expression of the self-antigen.
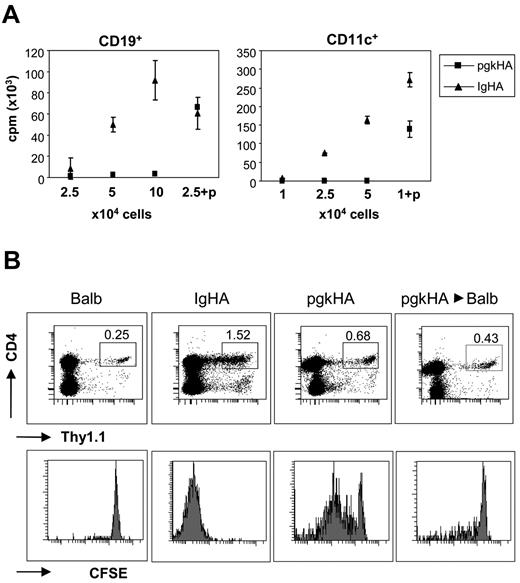
Under homeostatic conditions, HA is expressed and presented by splenic B cells and DCs in Ig-HA mice.29 As a result, sorted CD19+ or CD11c+ cells from the spleen of Ig-HA mice induced proliferation of HA-specific T cells in vitro (Figure 3A). In contrast, neither DCs nor B cells from pgk-HA mice were capable of inducing HA-specific proliferation in vitro, unless peptide was added to the culture (Figure 3A). However, CFSE-labeled HA-specific cells transferred into pgk-HA recipients did show some in vivo proliferation, even at levels much lower than those observed when the same cells were transferred into Ig-Ha recipients (Figure 3B). This proliferation was in great part because of antigen presentation by nonhematopoietic cells, such as liver sinusoidal endothelial cells,31 because HA-specific T cell transfer into chimeric recipients, where only the hematopoietic compartment was of pgk-HA origin, resulted in very poor T-cell proliferation (Figure 3B, last row). However, we cannot completely discard that, under certain inflammatory conditions, HA can be presented by DCs in pgk mice because bone marrow-derived DCs from pgk mice were able to induce HA-specific T-cell proliferation when stimulated by lipopolysaccharide, albeit at levels lower than those elicited by DCs from Ig-HA mice (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
HA presentation by hematopoietic cells in the periphery of TCR-HAxIg-HA but not in TCR-HAxpgk-HA mice. (A) CD11c+ and CD19+ cells were electronically sorted from Ig-HA and pgk-HA mice, and different amounts of cells were tested for their capacity to induce HA-specific proliferation in vitro. Peptide (p, 0.1 μg/mL) was added in 1 condition as positive control. (B) CD4+6.5+ cells from a Thy1.1 TCR-HA mouse were CFSE-labeled and transferred (1 × 106) into Balb/c, Ig-HA, or pgk-HA recipients. Balb/c mice reconstituted 7 weeks before with pgk-HA bone marrow (last column) were also used as recipients. Three days after transfer, the proliferation of CD4+Thy1.1+ cells in the lymph nodes was determined by flow cytometry. Representative dot plots are shown, and the percentage of Thy1.1+ cells within the CD4+ gate is indicated. Two mice per group and 2 independent experiments were performed with similar results.
HA presentation by hematopoietic cells in the periphery of TCR-HAxIg-HA but not in TCR-HAxpgk-HA mice. (A) CD11c+ and CD19+ cells were electronically sorted from Ig-HA and pgk-HA mice, and different amounts of cells were tested for their capacity to induce HA-specific proliferation in vitro. Peptide (p, 0.1 μg/mL) was added in 1 condition as positive control. (B) CD4+6.5+ cells from a Thy1.1 TCR-HA mouse were CFSE-labeled and transferred (1 × 106) into Balb/c, Ig-HA, or pgk-HA recipients. Balb/c mice reconstituted 7 weeks before with pgk-HA bone marrow (last column) were also used as recipients. Three days after transfer, the proliferation of CD4+Thy1.1+ cells in the lymph nodes was determined by flow cytometry. Representative dot plots are shown, and the percentage of Thy1.1+ cells within the CD4+ gate is indicated. Two mice per group and 2 independent experiments were performed with similar results.
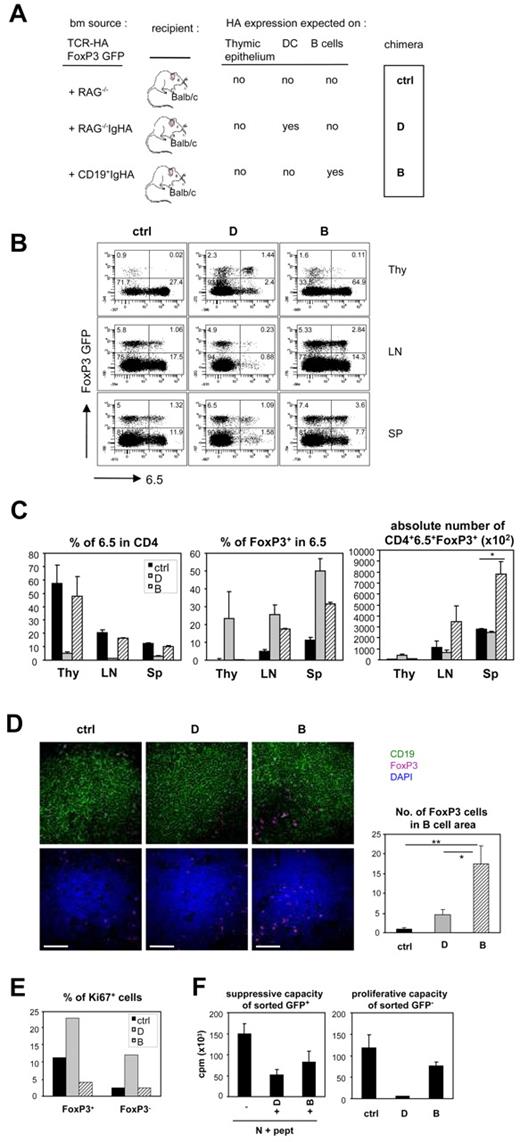
Self-antigen expression on B cells or DCs induces Tregs development or T-cell deletion/anergy, respectively
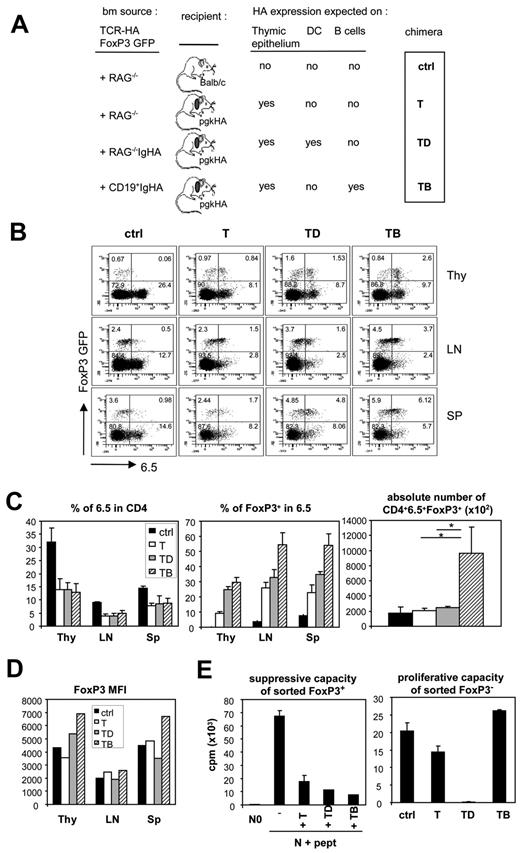
Based on the differences observed between the 2 double-transgenic mouse models described, we tried to further dissect the role of B cells versus DCs in tolerance induction toward self-antigens. For this, we generated bone marrow chimeras (Figure 4A) where HA-specific T cells (bone marrow from TCR-HA, FoxP3-GFP mice) would develop in a context with no HA expression (with Rag−/− bone marrow, in a Balb/c recipient/ctrl chimera), HA expression on thymic epithelium (with Rag−/− bone marrow in a pgk-HA recipient/T chimera), on thymic epithelium plus DCs (with Rag−/−Ig-HA bone marrow in a pgk-HA recipient/TD chimera), or on thymic epithelium plus B cells (with CD19+ cells from Ig-HA bone marrow in a pgk-HA recipient/TB chimera). Based on the results described in Figure 3B, HA expression by nonhematopoietic cells in the periphery of the pgk-HA recipients cannot be excluded, but one would expect it to remain constant between the T, TD, and TB chimeras. In all chimeras, the TCR-HA FoxP3-GFP bone marrow generated a population of TCR transgenic T cells together with non–HA-expressing B cells and DCs. HA-expressing DCs or B cells were generated by the coadministration of RAG−/−IgHA bone marrow (TD chimeras) or CD19+ cells from Ig-HA bone marrow (TB chimeras), respectively.
Development and function of HA-specific FoxP3+ and FoxP3− cells in the different chimeras expressing HA in the thymus. Thymi, lymph nodes, and spleen cell suspensions from the different chimeras illustrated in panel A were analyzed for 6.5 and GFP expression within the CD4+ gate. Shown are representative dot plots (B) as well as the percentage of 6.5 cells in the CD4 gate, of FoxP3+ cells in the CD4+6.5+ gate and the absolute numbers of CD4+6.5+FoxP3+ cells in lymph nodes and spleen (C). Three mice per group were analyzed. (D) The mean fluorescence intensity of GFP within the CD4+6.5+GFP+ gate is shown. (E) CD4+6.5+GFP+ and GFP− cells from lymph node suspensions of each type of chimera were electronically sorted and tested in vitro for their suppressive and proliferative capacity, respectively. For the suppression assay, naive 6.5+ cells were incubated with Balb/c splenic DCs in the absence or presence of peptide (0.1 μg/mL) and in the absence or presence of GFP+ cells from the different chimeras. For the proliferation assay, GFP− cells from the different chimeras were coincubated with DCs and peptide. The experiment was performed in triplicate, and 2 independent experiments gave similar results.
Development and function of HA-specific FoxP3+ and FoxP3− cells in the different chimeras expressing HA in the thymus. Thymi, lymph nodes, and spleen cell suspensions from the different chimeras illustrated in panel A were analyzed for 6.5 and GFP expression within the CD4+ gate. Shown are representative dot plots (B) as well as the percentage of 6.5 cells in the CD4 gate, of FoxP3+ cells in the CD4+6.5+ gate and the absolute numbers of CD4+6.5+FoxP3+ cells in lymph nodes and spleen (C). Three mice per group were analyzed. (D) The mean fluorescence intensity of GFP within the CD4+6.5+GFP+ gate is shown. (E) CD4+6.5+GFP+ and GFP− cells from lymph node suspensions of each type of chimera were electronically sorted and tested in vitro for their suppressive and proliferative capacity, respectively. For the suppression assay, naive 6.5+ cells were incubated with Balb/c splenic DCs in the absence or presence of peptide (0.1 μg/mL) and in the absence or presence of GFP+ cells from the different chimeras. For the proliferation assay, GFP− cells from the different chimeras were coincubated with DCs and peptide. The experiment was performed in triplicate, and 2 independent experiments gave similar results.
The different chimeras were analyzed 8 to 12 weeks after reconstitution. As shown in Figure 4B and C, the presence of HA in the thymus (chimeras T, TD, and TB) resulted in a partial deletion of 6.5+ cells compared with the control (ctrl chimera) but enhanced selection of CD4+6.5+FoxP3+ thymocytes. In the periphery, the same tendency was seen, both in lymph nodes and in spleen. However, chimeras expressing HA on both thymic epithelium and B cells (TB chimeras) displayed the higher percentage and absolute numbers of FoxP3+ HA-specific T cells in secondary lymphoid organs (Figure 4C).
We next tried to determine whether Tregs generated in the different types of chimeras were functional. The intensity of expression of FoxP3 is considered to be a marker for suppressive capacity, and decreased Foxp3 expression results in the development of an aggressive autoimmune syndrome, although anergic properties of the cells are maintained.32 Interestingly, Tregs from the TB chimeras were those with the highest FoxP3 expression (Figure 4D). CD4+6.5+FoxP3+ cells obtained from the different chimeras were all capable of suppressing HA-specific T-cell proliferation in vitro with comparable efficiency (Figure 4E). Remarkably, FoxP3− T cells sorted from the different chimeras behaved very differently; whereas HA-specific T cells from T and TB chimeras were capable of proliferating in vitro on antigenic stimulation, those from TD chimeras were not (Figure 4E).
These results indicate that self-antigen expression by B cells is very efficient in promoting FoxP3+ T cells, whereas self-antigen expression by DCs results in T cell anergy.
Self-antigen expression on thymic epithelium is not necessary for the enhancement of Treg generation by B cells
To determine whether antigen expression by B cells alone (ie, no HA expression on thymic epithelium) would also be efficient in promoting FoxP3+ T cells, we performed more experiments with bone marrow chimeras (Figure 5A). This time, all recipients were Balb/c-and thus did not express HA on thymic epithelium, but we reconstituted them with TCR-HA Foxp3EGFP bone marrow together with either DCs (bone marrow from Rag−/−IgHA mice, D chimera) or B cells (CD19+ cells from IgHA bone marrow, B chimera) expressing HA. Figure 5B-C shows that HA expression by DCs induced very efficient thymic deletion of CD4+6.5+ cells, as previously reported,29 whereas HA expression by B cells did not induce significant thymic deletion. These data are in agreement with the fact that B cells represent a very small population in the thymus and do not delete CD4+ T cells efficiently.33 In accordance, HA mRNA expression was only detected in the D chimera (supplemental Figure 2). Furthermore, these results indicate that very little B cell–derived HA antigen, if at all, is being cross-presented by DCs, at least in the thymus. As a result, the percentage of FoxP3+ cells among CD4+6.5+ thymocytes was higher in the D chimera than in the other mice (Figure 5C). However, results were different in periphery, where the percentage of FoxP3+ cells among CD4+6.5+ cells increased significantly in the B chimera (Figure 5B-C) and their absolute numbers were significantly higher than those in the D chimera (Figure 5C). Indeed, the absolute numbers of CD4+6.5+FoxP3+ cells in the D chimera were very low because of a significant deletion of HA-specific cells, both in thymus and the periphery. In vitro proliferation experiments performed with DCs sorted from the spleens of B and D chimeras confirmed that DCs from D mice expressed and presented HA antigen, as expected, whereas DCs from B mice were not capable of inducing T-cell proliferation, at least at detectable levels, thus excluding cross-presentation of B cell–derived HA antigen also in the periphery (supplemental Figure 3).
Development and function of HA-specific FoxP3+ and FoxP3− cells in the absence of HA expression in the thymus. Thymi, lymph nodes, and spleen cells suspensions from the different chimeras illustrated in panel A were analyzed for 6.5 and GFP expression within the CD4+ gate. Shown are representative dot plots (B) as well as the percentage of 6.5 cells in the CD4 gate, of FoxP3+ cells in the CD4+6.5+ gate, and the absolute numbers of CD4+6.5+FoxP3+ cells (C). A total of 3 mice per group were analyzed. (D) Immunofluorescence staining for CD19 (green), Foxp3 (purple), and nuclei (blue) in spleen sections of the different chimeras. The graphs represent the quantification of Foxp3+ cells in CD19+ follicules. Bar represents 50 μm. (E) The percentage of intracellular Ki67+ cells within the FoxP3+ and FoxP3− CD4+6.5+ cells was determined by flow cytometry. (F) CD4+6.5+GFP+ and GFP− cells from lymph node and spleen suspensions of each type of chimera were electronically sorted and tested in vitro for their suppressive and proliferative capacity, respectively, as described in Figure 4.
Development and function of HA-specific FoxP3+ and FoxP3− cells in the absence of HA expression in the thymus. Thymi, lymph nodes, and spleen cells suspensions from the different chimeras illustrated in panel A were analyzed for 6.5 and GFP expression within the CD4+ gate. Shown are representative dot plots (B) as well as the percentage of 6.5 cells in the CD4 gate, of FoxP3+ cells in the CD4+6.5+ gate, and the absolute numbers of CD4+6.5+FoxP3+ cells (C). A total of 3 mice per group were analyzed. (D) Immunofluorescence staining for CD19 (green), Foxp3 (purple), and nuclei (blue) in spleen sections of the different chimeras. The graphs represent the quantification of Foxp3+ cells in CD19+ follicules. Bar represents 50 μm. (E) The percentage of intracellular Ki67+ cells within the FoxP3+ and FoxP3− CD4+6.5+ cells was determined by flow cytometry. (F) CD4+6.5+GFP+ and GFP− cells from lymph node and spleen suspensions of each type of chimera were electronically sorted and tested in vitro for their suppressive and proliferative capacity, respectively, as described in Figure 4.
Immunohistochemical analysis revealed different distribution of Tregs in spleens (Figure 5). In control mice, the great majority of CD3 (not shown) and FoxP3 cells (Figure 5D) were outside the B-cell zones. In D chimeras, some FoxP3+ cells were inside the B-cell zones but basically remained at the margins, which are rich in follicular DCs.34 In contrast, B chimeras showed accumulation of FoxP3+ cells within the B-cell zones. These data were confirmed by a quantitative analysis of FoxP3+ cell distribution within splenic B-cell zones.
To understand whether in the B chimera B cells induced expansion of thymic-derived FoxP3+ cells or their de novo generation, we analyzed T-cell proliferation by staining for Ki67, a cell proliferation marker.35 Independently of FoxP3 expression, CD4+6.5+ cells from the B chimeras were similar to those obtained from control mice in terms of in vivo proliferation, suggesting that the increase in the CD4+6.5+FoxP3+ cell compartment observed in B chimeras is the result of de novo generation of Tregs in periphery (Figure 5E) rather than their expansion. We also observed that in D chimeras HA specific T cells were proliferating more in vivo than their “naive” counterparts, independently of their FoxP3 expression, suggesting that antigen presentation by DCs induces constitutive proliferation even under homeostatic conditions.
Finally, the suppressive capacity of FoxP3+ T cells generated in B and D chimeras was confirmed in in vitro experiments performed after sorting of FoxP3+ and FoxP3− cells (Figure 5F). This experiment also confirmed that HA-specific T cells obtained from mice that express the antigen on DCs (D chimera) are unable to proliferate (Figure 5F).
Although we cannot formally exclude that the levels of HA expression by DCs and B cells in this transgenic system may be different and may also play a role, HA mRNA expression by these cells, determined by real-time PCR, was similar (supplemental Figure 4).
Altogether, data obtained in B chimeras indicate that, even in the absence of antigen expression in the thymus, Tregs can be efficiently generated in periphery by B cells expressing a self-antigen, and this seems to be the result of a de novo generation. In contrast, self-antigen expression by DCs is very efficient in deleting antigen-specific T cells and in inducing anergy among the remaining FoxP3− cells.
Discussion
Treg induction in the thymus can be achieved by epithelial thymic cells but also by DCs and thus seems to be more dependent on the maturation state of the thymocyte than on the cell presenting the antigen.36 We confirm here that expression of agonist ligand in the thymus, either on thymic epithelial cells or on thymic DCs, leads to both negative selection of antigen-specific T cells and induction of antigen-specific Tregs. The stronger thymic deletion observed in the TCR-HAxIg-HA mice compared with the TCR-HAxpgk-HA mice (Figure 1A) is because, in the former, HA is expressed by thymic epithelium and DCs and, as expected, total mRNA HA expression levels are much higher in Ig-HA mice than in pgk-HA mice (supplemental Figure 2). It has been recently reported that thymic expression of cognate antigen can induce IL-17–producing, antigen-specific T cells in addition to FoxP3+ cells.37 Interestingly, we did indeed find more IL-17–producing cells among CD4 cells in the thymus of both strains of mice expressing HA antigen in the thymus (supplemental Figure 5); however, they were not positive for the HA-specific TCR, indicating that Tregs may favor IL-17–producing T-cell generation, but independently of their antigen specificity.
We also show here that, in single transgenic TCR-HA mice, the percentage and absolute number of HA-specific Tregs increase in the periphery compared with the thymus as has already been reported,38 strongly suggesting conversion and/or expansion of Tregs even in the absence of cognate ligand. When comparing both types of HA-expressing mice (TCR-HAxpgk-HA and TCR-HAxIg-HA), we found that the percentage and absolute numbers of HA-specific cells increased with age in the TCR-HAxIg-HA mice, whereas it decreased in the TCR and in the TCR-HAxpgk-HA mice. This increase in absolute numbers with age was in great part the result of a striking increase in the size of secondary lymphoid organs in the TCR-HAxIg-HA mice. The reasons for this are not clear, and no signs of autoimmunity could be observed in these mice as has been described for TCR-HA transgenic mice expressing HA antigen under the major histocompatibility complex class II promoter,39 although we do have some evidence for systemic B-cell activation (A.S., unpublished data, 2003).
Another striking difference between both types of mice was the fate of the HA-specific FoxP3− cells: GFP− cells from the TCR-HAxpgk-HA mice were not anergic on further antigenic stimulation in vitro, in contrast to the GFP− cells from TCR-HAxIg-HA mice. The fact that GFP− cells from TCR-HAxpgk-HA mice express slightly lower levels of the transgenic TCR compared with their counterparts from TCR-HAxIg-HA mice (Figure 1A) may contribute to explain this phenomenon because it has been reported that down-regulation of TCR levels may contribute to escape anergy induction.40
The bone marrow chimera experiments performed in this study demonstrate that different types of antigen-presenting cell can induce tolerance to self-antigens via different mechanisms. HA expression on B cells resulted in expansion of HA-specific Tregs, without the considerable deletion and anergy induction of antigen-specific FoxP3− cells observed on expression of HA by DCs. The experiments shown in Figure 5 permit us to conclude that the anergy of 6.5+FoxP3− cells from TCR-HAxIg-HA mice and from the TD chimeras is the result of antigen encounter on DC in the periphery and not of antigen encounter in the thymus or on nonhematopoietic cells. Furthermore, they confirm that HA expression by B cells alone was sufficient to induce HA-specific Tregs, and suggest that this was the result of B-cell/T-cell interactions in secondary lymphoid structures. The reason we did not observe higher numbers of 6.5+FoxP3+ cells in the periphery of TCR-HAxIg-HA mice despite expression of HA by B cells is that HA is also expressed by thymic epithelium and DCs, inducing a strong deletion of these cells.
The role of B cells in inducing Tregs has been strongly suggested by other reports. Thus, μMT KO B cell-deficient mice express lower levels of Tregs,38 are less efficient in Treg induction via oral feeding of antigen,41 and do not recover normally after acute experimental autoimmune encephalomyelitis induction.42 Furthermore, mouse43 and human19 B cells promote expansion of allogeneic Tregs ex vivo. The mechanisms involved in such induction as well as the activation state of the B cells required for such phenomena remain poorly defined. Although rituximab-mediated depletion of B cells in pathogenic conditions has been reported to ameliorate autoimmune diseases,17 repopulation with normal B cells led to amelioration of autoimmune diabetes44 and adoptive transfer of B cells suppressed inflammatory responses in a mouse model of primary biliary cirrhosis.45 Naive B cells have been shown to generate Tregs in the presence of a mature immunologic synapse.18 However, in our TCR-HAxIg-HA mice, there is evidence of B-cell activation (A.S., unpublished results, 2003), and it has been shown that CD40L-activated human B cells can efficiently induce expansion of Tregs,46 so it is not clear whether the activation state of the B cell plays a role. Cytokines, such as TGF-β3,47 TGF-β1,48 and IL-10, produced by follicular B cells49 have also been reported to be involved in Treg induction by B cells. The precise mechanisms and molecules involved in our system are currently under investigation.
In conclusion, although we do not put in doubt that DCs can generate Tregs, we show that they actually may be more efficient in inducing tolerance via deletion and anergy of antigen-specific FoxP3− cells. Contrary to DCs, B cells do not traffic from tissues to lymph nodes; thus, their capacity to induce Tregs specific for the nonhematopoietic self may be restricted under physiologic conditions. However, B cells can be made to present antigens via the administration of chimeric antibodies that target Fc receptors, an approach that was described to efficiently induce antigen-specific T-cell tolerance in mice.50 Furthermore, gene therapy approaches in mice with retroviral vectors that introduce peptide-IgG constructs in B cells have been shown to successfully reduce the incidence or onset of different autoimmune diseases.51 Thus, the data presented in this study may have important implications in clinical protocols aimed at the peripheral expansion of Tregs in patients.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Harald von Boehmer and Marinos Kallikourdis for critical reading of the manuscript and valuable suggestions, Ludger Klein for the pgk-HA mice, Chiara Buracchi and Achille Anselmo for cell sorting, and Marta Lezama for excellent animal care.
S.M. was supported by Fondazione Cassa di Risparmio delle Provincie Lombarde (grant 5808/2007). A.V. was supported by EU-FP7 SYBILLA (grant 201106) and Associazione Italiana Ricerca sul Cancro. A.S. was supported by Inserm and Fondazione Fondazione Cassa di Risparmio delle Provincie Lombarde (grant 5808/2007).
Authorship
Contribution: S.M., C.S., and A.S. performed experiments and analyzed data; S.M. and A.S. designed experiments; and A.V. and A.S. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Adelaida Sarukhan, Istituto Clinico Humanitas, IRCCS, Milan, Italy; e-mail: adelaida.sarukhan@humanitasresearch.it.