Abstract
To specify the incidence and risk factors for secondary autoimmune diseases (ADs) after HSCT for a primary AD, we retrospectively analyzed AD patients treated by HSCT reported to EBMT from 1995 to 2009 with at least 1 secondary AD (cases) and those without (controls). After autologous HSCT, 29 of 347 patients developed at least 1 secondary AD within 21.9 (0.6-49) months and after allogeneic HSCT, 3 of 16 patients. The observed secondary ADs included: autoimmune hemolytic anemia (n = 3), acquired hemophilia (n = 3), autoimmune thrombocytopenia (n = 3), antiphospholipid syndrome (n = 2), thyroiditis (n = 12), blocking thyroid-stimulating hormone receptor antibody (n = 1), Graves disease (n = 2), myasthenia gravis (n = 1), rheumatoid arthritis (n = 2), sarcoidosis (n = 2), vasculitis (n = 1), psoriasis (n = 1), and psoriatic arthritis (n = 1). After autologous HSCT for primary AD, the cumulative incidence of secondary AD was 9.8% ± 2% at 5 years. Lupus erythematosus as primary AD, and antithymocyte globulin use plus CD34+ graft selection were important risk factors for secondary AD by multivariate analysis. With a median follow-up of 6.2 (0.54-11) years after autologous HSCT, 26 of 29 patients with secondary AD were alive, 2 died during their secondary AD (antiphospholipid syndrome, hemophilia), and 1 death was HSCT-related. This European multicenter study underlines the need for careful management and follow-up for secondary AD after HSCT.
Introduction
Hematopoietic stem cell transplantation (HSCT) fundamentally interferes with the immune system. As a consequence, several types of autoimmune diseases (ADs) were observed after both autologous and allogeneic HSCT.1 Published data stem from isolated case reports or from single-center series of patients with new onset of AD after HSCT for different diseases. Most frequently, antibody-associated organ-specific autoimmune diseases, such as thyroiditis, immune thrombocytopenia (ITP), autoimmune hemolytic anemia (AIHA), or myasthenia gravis, have been reported.2-4
When treating severe AD, conditioning prior HSCT targets the immune system and autoreactive cells within the immune system. Therefore, intense lympho-depleting conditioning regimens are used for these patients.5 This profound interaction with the adaptive immune system and the possibility of a genetic disposition for a patient to develop more than 1 AD6 may set patients with primary AD at higher risk for developing a secondary AD after HSCT.
With increased transplant activity for patients with severe AD, several cases of secondary AD were reported. First, in a single-center North American retrospective study,7 6 of 155 patients with various ADs developed a secondary AD after autologous HSCT, partly related to intense T-cell depletion during conditioning with antithymocyte globulin (ATG) or alemtuzumab (CD-52 antibodies). Two other cases of systemic sclerosis patients were studied after HSCT for secondary onset of ITP, followed by Graves disease and systemic lupus erythemathosus (SLE) with antiphospholipid syndrome in the first one8 and myasthenia gravis in the other.9 Because secondary ADs may occur after HSCT for a primary AD, identification of their risk factors is important to improve patient care and may impact on outcome after HSCT. Using the worldwide largest cohort, the European Blood and Marrow Transplantation (EBMT) database ProMISe, with > 1300 patients treated by HSCT for a primary AD, we designed the present study aiming to characterize the nature, incidence, and risk factors for secondary AD after HSCT for a primary AD.
Methods
This retrospective study was approved and conducted by the EBMT Autoimmune Disease Working Party following the EBMT study guidelines. The EBMT centers report systematically all their consecutive transplants for AD to the EBMT. All EBMT centers were invited to participate and fill up a specific questionnaire (MED C, including specific diagnostic criteria for secondary AD) to identify patients having (cases) or not (controls) developed one or more AD after first HSCT. Twenty-eight centers agreed to participate enabling us to collect information on 363 patients treated by HSCT for a primary AD. Referring physicians were asked whether the diagnostic criteria of the respective secondary AD were fulfilled. They had to complete information on primary AD diagnosis, HSCT, and outcome for all cases and controls and on diagnosis, treatment, and outcome of secondary AD for the identified cases. Informed consent was obtained from all patients before HSCT in accordance with the Declaration of Helsinki.
Results are given as numbers with median (ranges). Patients having developed secondary AD after allogeneic HSCT are only described because of the low number of cases and controls. All patients and controls after autologous HSCT were included in statistical analyses. The primary endpoint was the incidence of secondary AD. Patient-, disease-, and transplant-related variables of both groups (cases vs controls) were compared, using the χ2 statistic or the Fisher exact test for categorical and the Mann-Whitney test for continuous variables. Cumulative incidence curves were used for estimating incidence of secondary AD considering death as a competing event. Gray test was used for univariate comparisons.10 Associations of patient, disease, and graft characteristics after autologous HSCT with outcomes were evaluated in multivariate analyses using proportional subdistribution hazard regression model of Fine and Gray.11 The following parameters were included in this analysis: age at HSCT, time from diagnosis to HSCT, year of HSCT, diagnosis of primary AD, conditioning (cyclophosphamide, fludarabine, and cyclophosphamide in combination with fludarabine; BCNU, etoposide, Ara-C, and melphalan; busulfan; total body irradiation; and ATG), CD34+ selection of the graft, source of stem cells (bone marrow or peripheral blood), and maintenance therapy after HSCT. A stepwise backward procedure was used to construct a set of independent predictors of secondary AD. All predictors achieving a P value < .20 were considered and sequentially removed if the P value in the multiple model was > .10. All tests were 2-sided. The type I error rate was fixed at .05 for determination of factors associated with time to event outcomes. Statistical analyses were performed with SPSS Version 18.0 and TIBCO Spotfire S+ Version 8.1 software packages.
Results
Among 363 primary AD patients included from 28 centers in 12 European countries, 32 developed at least 1 secondary AD after HSCT. All patients were transplanted between June 1995 and November 2009. Because of the low number of patients having received allogeneic HSCT for a primary AD within this study and the major immunologic differences between autologous and allogeneic HSCT, cumulative incidence and risk factors for secondary AD were calculated only among patients having received autologous HSCT for an AD. Twenty-nine of these developed a secondary AD in median 21.9 months (range, 0.6-49 months) after autologous HSCT compared with 318 patients who did not develop a secondary AD after autologous HSCT and served as controls.
Patient characteristics for all patients and controls having received autologous HSCT
Detailed description of the patients' characteristics, original autoimmune disease, conditioning, type of graft, and graft manipulation for the cases and the controls having received autologous HSCT are given in Table 1. In short, patients who developed secondary AD were younger (P = .04), transplanted earlier after primary AD diagnosis (P = .06), and suffered more often from SLE as compared with controls (P = .02).
Characteristics of the patients (secondary AD case and control groups) treated by autologous HSCT for a primary AD
| Characteristics of the patients treated by autologous HSCT for a primary AD . | Secondary AD cases (n = 29) . | Controls (n = 318) . | P . |
|---|---|---|---|
| Female sex | 21 (72%) | 190 (60%) | .23 |
| Age at diagnosis, y | 20.3 (1.1-55) | 27 (< 1-62) | .17 |
| Age at HSCT, y | 27 (6.7-55.4) | 35.3 (4.2-65) | .04 |
| Interval (mo) from primary AD diagnosis to HSCT | 42.6 (2-179) | 63 (0.4-341) | .06 |
| Year of HSCT | 2002 (1997-2009) | 2002 (1995-2009) | .7 |
| Initial diagnosis, reason for HSCT | |||
| MS | 8 (28%) | 126 (40%) | |
| SSc | 10 (35%) | 94 (30%) | |
| JIA | 4 (14%) | 32 (10%) | |
| SLE | 5 (17%) | 15 (5%) | |
| RA | 1 (3%) | 21 (7%) | |
| Others* | 1 (3%) | 30 (9%) | |
| Conditioning | |||
| Cyclophosphamide | 17 (63%) | 164 (58%) | .27 |
| Fludarabine | 1 (4%) | 1 (< 1%) | |
| Cyclophosphamide/fludarabine | 2 (7%) | 17 (6%) | |
| BEAM | 3 (11%) | 67 (24%) | |
| TBI | 3 (11%) | 25 (9%) | |
| Busulfan | 1 (4%) | 10 (4%) | |
| Serotherapy | |||
| ATG | 26 (90%) | 251 (79%) | .23 |
| Alemtuzumab | 0 | 1 | |
| CD34+ selection | 22 (76%) | 169 (53%) | .04 |
| Stem cell source | |||
| Peripheral blood | 25 (86%) | 293 (92%) | .29 |
| Bone marrow | 4 (14%) | 25 (8%) | |
| Maintenance treatment after HSCT | 9 (31%) | 62 (28%) | .87 |
| Characteristics of the patients treated by autologous HSCT for a primary AD . | Secondary AD cases (n = 29) . | Controls (n = 318) . | P . |
|---|---|---|---|
| Female sex | 21 (72%) | 190 (60%) | .23 |
| Age at diagnosis, y | 20.3 (1.1-55) | 27 (< 1-62) | .17 |
| Age at HSCT, y | 27 (6.7-55.4) | 35.3 (4.2-65) | .04 |
| Interval (mo) from primary AD diagnosis to HSCT | 42.6 (2-179) | 63 (0.4-341) | .06 |
| Year of HSCT | 2002 (1997-2009) | 2002 (1995-2009) | .7 |
| Initial diagnosis, reason for HSCT | |||
| MS | 8 (28%) | 126 (40%) | |
| SSc | 10 (35%) | 94 (30%) | |
| JIA | 4 (14%) | 32 (10%) | |
| SLE | 5 (17%) | 15 (5%) | |
| RA | 1 (3%) | 21 (7%) | |
| Others* | 1 (3%) | 30 (9%) | |
| Conditioning | |||
| Cyclophosphamide | 17 (63%) | 164 (58%) | .27 |
| Fludarabine | 1 (4%) | 1 (< 1%) | |
| Cyclophosphamide/fludarabine | 2 (7%) | 17 (6%) | |
| BEAM | 3 (11%) | 67 (24%) | |
| TBI | 3 (11%) | 25 (9%) | |
| Busulfan | 1 (4%) | 10 (4%) | |
| Serotherapy | |||
| ATG | 26 (90%) | 251 (79%) | .23 |
| Alemtuzumab | 0 | 1 | |
| CD34+ selection | 22 (76%) | 169 (53%) | .04 |
| Stem cell source | |||
| Peripheral blood | 25 (86%) | 293 (92%) | .29 |
| Bone marrow | 4 (14%) | 25 (8%) | |
| Maintenance treatment after HSCT | 9 (31%) | 62 (28%) | .87 |
MS indicates multiple sclerosis; SSc, systemic sclerosis; JIA, juvenile idiopathic arthritis; RA, rheumatoid arthritis; BEAM, BCNU, etoposide, Ara-C, and melphalan; TBI, total body irradiation; ATG, antithymocyte globulin; and y, years.
Others for AD include patients with insulin-dependent diabetes mellitus; others for controls include non-Rheumatoid arthritis, other neurologic diseases, other connective diseases, vasculitis, and hematologic AD.
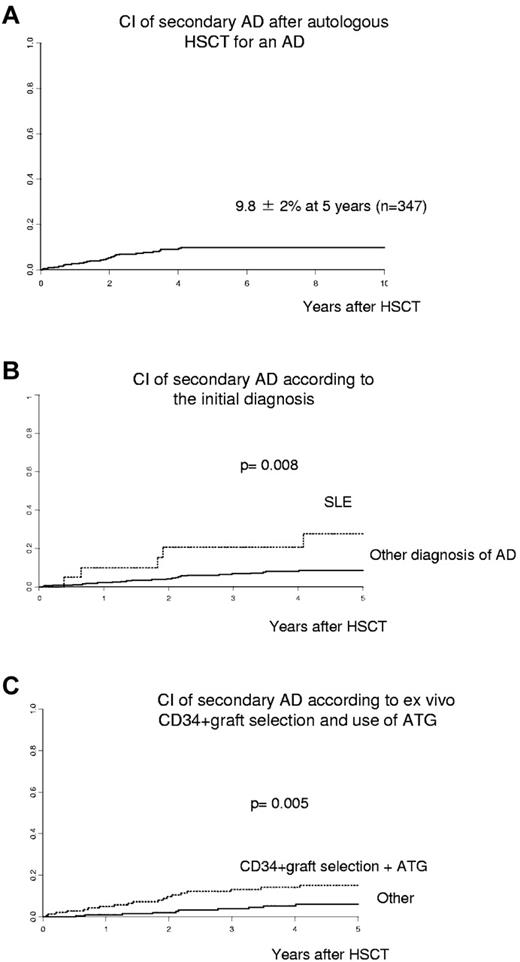
Incidence of secondary AD after autologous HSCT
The cumulative incidence of secondary AD after HSCT for AD was 7.7% (± 1%) after 3 years and 9.8% (± 2%) after 5 years (Figure 1). The observed secondary AD included: autoimmune hemolytic anemia (n = 3), acquired hemophilia (n = 3), autoimmune thrombocytopenia (n = 3), antiphospholipid syndrome (n = 2), thyroiditis (n = 10), blocking thyroid-stimulating hormone receptor antibody-associated hypothyroidism (n = 1), Graves disease (n = 2), myasthenia gravis (n = 1), rheumatoid arthritis (n = 2), sarcoidosis (n = 2), and psoriasis (n = 1), with 1 patient having developed 2 secondary ADs after HSCT. Disease-specific diagnostic criteria were fulfilled for all diagnoses. For the 2 cases with sarcoidosis, other causes of granulomatous disease were thoroughly excluded. One case of hypothyroidism was related to a blocking antibody against the thyroid-stimulating hormone receptor. One patient developed thrombocytopenia and, 2 months later, AIHA after autologous HSCT for multiple sclerosis. There was no association between the type of secondary AD and the time of onset after HSCT.
Cumulative incidence (CI). (A) Secondary ADs. (B) According to diagnosis of SLE versus other. (C) According to ex vivo CD34+ graft selection and ATG use for conditioning.
Cumulative incidence (CI). (A) Secondary ADs. (B) According to diagnosis of SLE versus other. (C) According to ex vivo CD34+ graft selection and ATG use for conditioning.
Risk factors for developing a secondary AD after autologous HSCT for primary AD
After multivariate analysis, initial diagnosis of SLE (P = .019; hazard ratio [HR] = 3.21; 95% confidence interval [CI], 1.21-8.48), the association of both ex vivo CD34+ selection after mobilization of peripheral blood stem cells and use of ATG for conditioning (P = .009; HR = 2.74; 95% CI, 1.29-5.80) and interval from diagnosis to autologous HSCT less than the median of 61 months (P = .028; HR = 2.32; 95% CI, 1.09-4.93) appeared as significant risk factors for developing a secondary AD after HSCT. There was also a trend for a higher risk of secondary AD in patients younger than the median age of 34.7 years at HSCT (P = .062; HR = 2.13; 95% CI, 0.96-4.71). The results of multivariate analyses are shown in Table 2.
Multivariate analysis of risk factors for secondary AD for all patients having received autologous HSCT for a primary AD
| Risk factors . | P . | HR . | 95.0% CI . |
|---|---|---|---|
| Age < 34.7 y | .062 | 2.13 | 0.96-4.71 |
| Interval diagnosis to HSCT < 62 mon | .028 | 2.32 | 1.09-4.93 |
| SLE vs other | .019 | 3.21 | 1.21-8.48 |
| ATG + CD34+ selection | .009 | 2.74 | 1.29-5.80 |
| Risk factors . | P . | HR . | 95.0% CI . |
|---|---|---|---|
| Age < 34.7 y | .062 | 2.13 | 0.96-4.71 |
| Interval diagnosis to HSCT < 62 mon | .028 | 2.32 | 1.09-4.93 |
| SLE vs other | .019 | 3.21 | 1.21-8.48 |
| ATG + CD34+ selection | .009 | 2.74 | 1.29-5.80 |
CI indicates confidence interval; AD, autoimmune disease; SLE, systemic lupus erythematosus; and vs, versus.
Treatment and outcome of secondary AD after autologous HSCT
The 5-year probability of overall survival was 88% ± 2% in controls versus 89% ± 6% in patients with a secondary AD (P = .71). Twenty-six of 29 cases (90%) with secondary AD were alive at a median follow-up of 6.2 years (range, 0.54-11 years) after autologous HSCT and 276 of 318 controls at a median follow-up of 5.9 years (range, 0.1-15 years) after HSCT. Among the 3 patients who died, one death in a patient primarily treated for multiple sclerosis was considered HSCT related after multidisciplinary evaluation, whereas the secondary AD (AIHA and ITP) was still ongoing. Two cases after autologous HSCT died during the course of their secondary AD: 1 from cerebral ischemia within 1 month after HSCT for primary systemic sclerosis, while at that time an antiphospholipid syndrome with positive lupus anticoagulant was first diagnosed; the other one, primarily treated for multiple sclerosis, died of hemorrhage because of an acquired factor VIII antibody, despite treatment with cyclophosphamide, rituximab, intravenous immunoglobulins, and recombinant factor VIIa (novo 7).
Twenty-four cases received specific therapy for their secondary AD and 5 did not. Ten patients with secondary autoimmune thyroiditis or Graves disease required L-thyroxine substitution and/or thyreostatic therapy. One case with secondary rheumatoid arthritis received prednisone, methotrexate, and abatacept. Patients with acquired hemophilia or AIHA received intense immunosuppression. At last follow-up, 10 patients remained in remission of secondary AD without treatment, 10 required ongoing therapy, and 5 had persistent secondary AD without therapy (Table 3).
Treatment and outcome of secondary AD in all patients having received autologous HSCT for a primary AD
| Original AD . | Secondary AD . | No. of patients . | Treatment of AD . | Status of secondary AD at last follow-up . |
|---|---|---|---|---|
| SLE | AIHA | 1 | Prednisone, cyclophosphamide, rituximab | Resolved |
| SSc | AIHA | 1 | None | Resolved |
| MS | Hemophilia | 1 | Prednisone, cyclophosphamide, IVIg, RTX, novo 7 | Dead |
| MS | Hemophilia | 1 | Prednisone, cyclophosphamide, cyclosporine, IVIg, PE | Resolved |
| SLE | Hemophilia | 1 | Prednisone, cyclophosphamide, IVIg, PE, RTX | Resolved |
| SSc | ITP | 1 | Prednisone | Resolved |
| MS | ITP | 1 | Prednisone | Resolved |
| MS | ITP/AIHA | 1 | Prednisone, MMF, IVIg, rituximab | Ongoing with therapy until dead (HSCT related) |
| 1 SLE/1 SSc | Antiphospholipid syndrome | 2 | Steroids/none | Resolved/dead |
| 1 JIA | Thyroiditis | 1 | Unknown | Unknown |
| 1 JIA/1 IDD | Thyroiditis | 2 | None/L-thyroxine | Ongoing without treatment |
| 1 SSc, 3 MS 1 JIA, 1 SLE | Thyroiditis | 6 | L-thyroxine or thyrostatic therapy | Ongoing with therapy |
| 1 MS | Thyroiditis | 1 | L-thyroxine | Resolved |
| SSc | Blocking TSHR antibody | 1 | None | Ongoing without therapy |
| SSc | Graves disease | 1 | Carbimazole | Ongoing with therapy |
| SLE | Graves disease | 1 | Thyroidectomy | Resolved |
| SSc | Myasthenia gravis | 1 | MMF | Ongoing with therapy |
| SSc | Rheumatoid arthritis | 1 | Methotrexate, abatacept | Ongoing with therapy |
| SSc | Rheumatoid arthritis | 1 | NSAIDs | Ongoing without therapy |
| JIA | Sarcoidosis | 1 | Prednisone, methotrexate | Ongoing with therapy |
| JIA | Sarcoidosis | 1 | Prednisone | Resolved |
| RA | Psoriasis | 1 | None | Ongoing without therapy |
| Original AD . | Secondary AD . | No. of patients . | Treatment of AD . | Status of secondary AD at last follow-up . |
|---|---|---|---|---|
| SLE | AIHA | 1 | Prednisone, cyclophosphamide, rituximab | Resolved |
| SSc | AIHA | 1 | None | Resolved |
| MS | Hemophilia | 1 | Prednisone, cyclophosphamide, IVIg, RTX, novo 7 | Dead |
| MS | Hemophilia | 1 | Prednisone, cyclophosphamide, cyclosporine, IVIg, PE | Resolved |
| SLE | Hemophilia | 1 | Prednisone, cyclophosphamide, IVIg, PE, RTX | Resolved |
| SSc | ITP | 1 | Prednisone | Resolved |
| MS | ITP | 1 | Prednisone | Resolved |
| MS | ITP/AIHA | 1 | Prednisone, MMF, IVIg, rituximab | Ongoing with therapy until dead (HSCT related) |
| 1 SLE/1 SSc | Antiphospholipid syndrome | 2 | Steroids/none | Resolved/dead |
| 1 JIA | Thyroiditis | 1 | Unknown | Unknown |
| 1 JIA/1 IDD | Thyroiditis | 2 | None/L-thyroxine | Ongoing without treatment |
| 1 SSc, 3 MS 1 JIA, 1 SLE | Thyroiditis | 6 | L-thyroxine or thyrostatic therapy | Ongoing with therapy |
| 1 MS | Thyroiditis | 1 | L-thyroxine | Resolved |
| SSc | Blocking TSHR antibody | 1 | None | Ongoing without therapy |
| SSc | Graves disease | 1 | Carbimazole | Ongoing with therapy |
| SLE | Graves disease | 1 | Thyroidectomy | Resolved |
| SSc | Myasthenia gravis | 1 | MMF | Ongoing with therapy |
| SSc | Rheumatoid arthritis | 1 | Methotrexate, abatacept | Ongoing with therapy |
| SSc | Rheumatoid arthritis | 1 | NSAIDs | Ongoing without therapy |
| JIA | Sarcoidosis | 1 | Prednisone, methotrexate | Ongoing with therapy |
| JIA | Sarcoidosis | 1 | Prednisone | Resolved |
| RA | Psoriasis | 1 | None | Ongoing without therapy |
MMF indicates mycophenolate mofetil; IVIg, intravenous immunoglobulin; PE, plasma exchange; NSAIDs, nonsteroidal anti-inflammatory drugs; RTX, rituximab; TSHR, thyroid stimulating hormone receptor; MS, multiple sclerosis; SSc, systemic sclerosis; and JIA, juvenile idiopathic arthritis.
Secondary AD after allogeneic HSCT for an AD
Three patients developed 4 secondary AD altogether after allogeneic HSCT and 13 patients did not. In short, a 17-year-old girl treated by allogeneic HSCT for SLE developed an autoimmune thyroiditis 3 months later. A 3-year-old boy originally treated for primary autoinflammatory syndrome by allogeneic HSCT developed new onset of simultaneous autoimmune thyroiditis and psoriatic arthritis after 17 months. The third patient first treated for ITP developed antineutrophil cytoplasmic antibody-associated vasculitis within 9 months after allogeneic HSCT. Whereas in the SLE patient, secondary thyroiditis resolved without treatment, the second case required thyroxin replacement therapy and a course of anti-CD20 therapy (rituximab) for both thyroiditis and psoriatic arthritis, and these 2 coexisting diseases were still ongoing at last follow-up 6 years after allogeneic HSCT. The third patient with secondary vasculitis died of nonvasculitic myocarditis 4 years after the allogeneic HSCT.
Discussion
Within our study population, secondary AD occurred in > 9% of patients from 3 weeks up to 4 years after autologous HSCT for a primary AD. This higher rate of secondary AD than previously reported7 may be explained by longer patient follow-up in this multicenter EBMT study. Because de novo thymic development of T lymphocytes can be delayed up to years after T cell-depleting conditioning for autologous HSCT,12,13 secondary AD may be diagnosed later throughout follow-up after transplantation.
In our study, diseases thought to be predominantly caused by autoantibodies to specific tissues (eg, thyroid tissue, platelets, erythrocytes) were by far the most commonly identified secondary AD. Among these, secondary autoimmune thyroiditis was the most frequently diagnosed secondary AD, with 2 cases showing spontaneous remission. However, more serious diseases occurred, such as AIHA, acquired hemophilia, and ITP, necessitating further intense, even cytostatic therapy after HSCT. Eventually, 2 patients died during the course of their secondary AD. Most of the patients included in this study had received autologous HSCT for their primary AD. The low number of patients treated by allogeneic HSCT for their autoimmune disease within our cohort did not allow statistical analysis with sufficient power. However, the 3 described cases allowed confirming that secondary AD can also occur after allogeneic HSCT.
Primary diagnosis of SLE as the indication for HSCT appeared as a significant risk factor for secondary AD after autologous HSCT. SLE per se is a paradigm of autoimmune disease, characterized by the presence of many pathogenic autoantibodies (eg, antinuclear, anti-DNA, anticardiolipin antibodies, or antibodies directed against various blood cell components).14 These autoantibodies may be the product of the bone marrow long-lived plasma cells and may have been present at low titers before HSCT, without associated pathogenicity. Plasma cells can survive vigorous lympho-depletion by HSCT,15 if regulatory cells, controlling these autoreactive plasma cells are suppressed by conditioning; clinically significant manifestations of autoimmunity may develop.16 De novo emergence of autoreactive B or T cells after HSCT may also contribute to autoimmunity in these patients.
Intense immunosuppression during conditioning aims to treat severe primary AD and to reinduce tolerance during the immune reconstitution process after HSCT. The whole procedure interferes with the balance between tolerance and autoimmunity; and in this setting, new onset of secondary AD after HSCT is an unwanted side effect. Mechanisms for development of secondary AD may be related to loss of peripheral tolerance after conditioning (eg, by deletion of regulatory cells),8 proliferation of autoreactive cells after HSCT by homeostatic expansion,17 failure of negative selection during de novo thymic ontogenesis of T lymphocytes,18 or accumulation of mutations during increased proliferation of lymphocytes after HSCT.19 This may explain why a more intense T-cell depletion with the combination of ATG for conditioning and CD34+ selection of the graft is associated with an increased incidence of secondary AD after autologous HSCT. Our findings are in line with the association of the use of ATG or alemtuzumab for conditioning7 with the development of secondary AD in the single-center study on 155 primary AD patients having received autologous HSCT. In our cohort, only one patient treated for primary AD had received alemtuzumab, which does not allow statistical analysis. The trend to a higher rate of secondary AD in younger patients observed in the present study remains unexplained, knowing the decline of thymic function with age and its role in inducing tolerance. However, our findings are supported by one single-center study that reported a very high incidence of secondary AD in newborns after cord blood transplantation for metabolic diseases.20
Earlier autologous HSCT after diagnosis of AD may increase the risk for subsequent secondary AD. The decision for HSCT in these patients depends on many factors and may differ substantially between caring physicians. These potential factors contributing to this effect were not assessed in our study.
Results from this first multicenter study on the risk factors for secondary AD after HSCT cannot be extended to patients having received HSCT for diagnoses other than primary AD. However, new onset of autoimmune diseases has been previously reported in patients having received autologous HSCT for other indications than autoimmune diseases.1 Most often hematologic autoimmune diseases, such as ITP or AIHA, have been observed in published cases.21 To our knowledge, data on incidence and risk factors for secondary AD in this population are not available.
In conclusion, patients with SLE, younger age at HSCT, or receiving severe T cell-depleting conditioning (ATG, alemtuzumab, CD34+ selection) need close monitoring for secondary AD after autologous HSCT. Further prospective studies analyzing patients treated for primary AD or for other hematologic indications will help to delineate the various patterns and mechanisms of autoimmunity before and after HSCT.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
T.D. is supported by an EULAR grant and by the Freiwillige Akademische Gesellschaft Basel.
Authorship
Contribution: T.D. and D.F. designed the study, analyzed the data, and prepared the manuscript; M.L. performed statistical analysis; M.B. collected data; and M.D.G., M.A., T.A., I.M., F.G., A. Fassas, T.M., C.P.S., N.W., M.B., A.S., E.C., B.D., B.G., T.G., D.P., A.S., E.S., J.S., P.V., A. Fasth, S.L., C.M., J.V., J.H., D.L., A.T., and E.G. contributed data and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A list of EMBTWP members can be found in the supplemental Appendix (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Correspondence: Thomas Daikeler, Department of Rheumatology, University Hospital Basel, 4031 Basel, Switzerland, e-mail: tdaikeler@uhbs.ch.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal