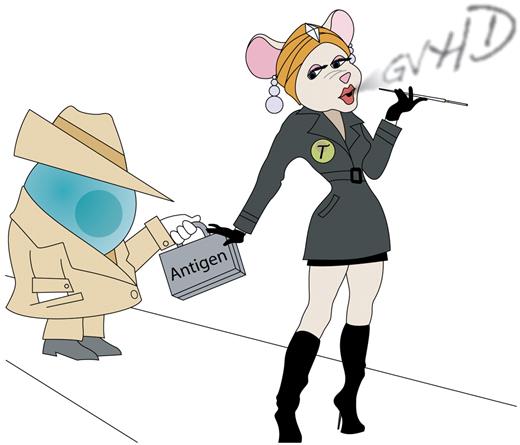
The name Mata Hari is synonymous with espionage and secrecy, and in this issue of Blood the “MataHari” mouse has helped Toubai and colleagues reveal the role that nonhematopoietic antigen presentation plays in initiating graft-versus-host disease (GVHD).1
Since the seminal study of Shlomchik et al demonstrated the importance of recipient-derived antigen presenting cells (APCs) in initiating GVHD,2 a significant body of work has detailed the relative contributions of donor and host APC in major versus minor histocompatibility antigen-mismatched transplantation for both GVH and graft-versus-tumor (GVT) responses.3-6 Still, there has been an enduring dogmatic assumption that dendritic cells, the “professional” hematopoietic APC population whose discovery recently earned the late Ralph Steinman a Nobel prize, were the sole population necessary and sufficient for activation of GVHD-mediating alloreactive donor T cells. Using a cadre of transplantation models involving both polyclonal and transgenic donor T-cell responses, Toubai et al demonstrate the fallacy of this assumption (see figure).
Host dendritic cells are thought to be critical for the initial activation of alloreactive donor T cells and initiation of GVHD after allogeneic hematopoietic transplantation. Toubai et al use a series of experimental models, including transplantation with H-Y antigen-specific Mata Hari T cells, to demonstrate that host hematopoietic antigen-presenting cells may not be essential for initiation of GVHD. Professional illustration by Kenneth X. Probst.
Host dendritic cells are thought to be critical for the initial activation of alloreactive donor T cells and initiation of GVHD after allogeneic hematopoietic transplantation. Toubai et al use a series of experimental models, including transplantation with H-Y antigen-specific Mata Hari T cells, to demonstrate that host hematopoietic antigen-presenting cells may not be essential for initiation of GVHD. Professional illustration by Kenneth X. Probst.
The authors first demonstrate that, in addition to polyclonal anti–H-Y responses, recognition of single H-Y antigenic epitopes is sufficient for initiating GVHD mediated by CD8 T cells from MataHari TCR transgeneic mice or by CD4 T cells from “Marilyn” and “Rachel” TCR transgenic mice. They then identified that H-Y expression on recipient stroma was critical for GVHD severity from Marilyn CD4 T cells; however, antigen presentation by recipient hematopoietic cells was not necessary. Furthermore, CD8 MataHari T cells were able to mediate GVHD even in the absence of both donor and recipient hematopoietic MHC class I. Toubai et al's study focuses on clinically relevant minor histocompatibility antigen-mismatched GVHD models, assessing GVHD lethality and pathology, as well as sensitive cytokine readouts of alloreactivity. The authors employ an array of experimental models, including transgenic T cells or pretransplant priming, which is similar to the pretransplant priming that may occur clinically in parous females. Interestingly, across their multiple models, the finding of a nonhematopoietic contribution to antigen presentation and alloreactivity remained robust.
Along with a recent paper from Koyama et al,7 Toubai and colleagues provide compelling evidence to indicate that hematopoietic APCs may not be essential for induction of acute GVHD, although they clearly do contribute to it. This study provides pathophysiologic insight and serves as a cautionary tale, indicating that the systemic complexity of in vivo GVH reactions continues to surprise despite decades of intensive research. Given the multiple routes that can lead to the activation of alloreactive responses, efforts to translate the findings of experimental transplantation into clinical management are fighting an uphill battle to prevent GVHD. Future design of clinical trials aiming to block GVHD by preventing the activation of donor T cells against APCs must thus account for nonhematopoietic as well as dendritic cell–mediated antigen presentation. Furthermore, the capacity of nonhematopoietic APCs to initiate GVHD potentially explains the clinical conundrum of acute GVHD development well after the initial tissue damage of pretransplant conditioning. If nonhematopoietic APCs are sufficient for inducing alloreactive GVH responses, then any episode of tissue damage, whether mediated by infection or other environmental factors, could potentially trigger the cascade of GVHD well after donor hematopoietic engraftment. Daunting as that may sound, the identification of multiple routes to alloreactivity may be sufficient for inducing optimism among experimentalists and clinicians for the dissociation of GVH and GVT responses.
Nonhematopoietic MHC class II expression has been known for some time, particularly within the gastrointestinal tract and thymus.8,9 Now that we have learned that nonhematopoietic antigen presentation may be sufficient for initiating GVHD, the challenge has been put forth to determine which cell populations are performing this function and how it is accomplished. Toubai and colleagues propose endothelial and epithelial cells as putative nonhematopietic APCs in GVHD, while Koyoma et al offer myofibroblasts as another potential culprit. It is presently unclear if this nonhematopoietic antigen presentation and alloactivation are actually occurring within target tissues, or if they are mediated by stromal cells within secondary lymphoid organs. The latter process would be consistent with the current paradigm of alloreactive donor T cells undergoing their initial activation within the lymph nodes and Peyer patches before their destructive tissue infiltration.10 Furthermore, a recent study by Wang et al suggests that donor dendritic cells could actually mediate the presentation of nonhematopoietic antigen by incorporating recipient MHC into their own cell membranes.11 Similar to the mystery surrounding Mata Hari, the sources and mechanisms of GVHD-inducing nonhematopoietic antigen presentation are thus still unknown. The dynamic work presented here represents a major step toward uncovering this clandestine GVHD pathophysiology.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal