Abstract
The effectiveness of prophylactic platelets (plts) to prevent bleeding in patients with hematological malignancies remains unclear. The aim of this trial was to test the hypothesis that a policy of no-prophylactic plt transfusions (PltTx) is as effective and safe as a policy of prophylactic PltTx.
TOPPS was a randomized, parallel group, open-label, non-inferiority trial that recruited from 14 UK and Australian hospitals (ISRCTN08758735). The primary outcome was proportion of patients with a clinically significant bleed, defined as ≥WHO Grade 2, up to 30 days (d) from randomization. Non-inferiority margin was defined as a 15% difference in proportion of patients experiencing the primary outcome. Adult patients were eligible if they had a hematological malignancy, were receiving chemotherapy or stem cell transplant (SCT) and expected to be thrombocytopenic for at least 5 days. Patients were randomized by centralized computer system to receive either prophylactic PltTx if plt count was <10×109/L, or no prophylaxis. Allocated treatment policy applied for 30d from randomization, irrespective of in- or out-patient status. In both arms PltTx were given therapeutically (documented signs or symptoms of bleeding) or prior to invasive procedures or at physician discretion. Analysis was by intention to treat.
Recruitment began August 2006 and closed in August 2011. Of 1093 patients screened, 600 patients were randomized (301 no-prophylaxis, 299 prophylaxis). Baseline characteristics were well matched. 70% patients in both arms received autologous SCT (autoSCT). The majority of patients in both arms had complete bleeding data recorded [median 30d (IQR 29 to 30) no-prophylaxis arm, median 30d (IQR 30 to 30) prophylaxis arm]. Two patients (1 in each arm) withdrew prior to any data collection. Most PltTx in both arms were given according to protocol (no-prophylaxis 450/504 (89%) vs prophylaxis 810/894 (91%). Fewer patients in the no-prophylaxis group received PltTx (176/300, 59%) vs. prophylaxis group (266/298, 89%) [OR 0.14 (95% CI 0.09 to 0.23]; and they also received fewer PltTx overall [no-prophylaxis mean 1.7 PltTx (SD 2.6) vs. prophylaxis mean 3.0 PltTxs (SD 3.2); rate ratio 0.62, 95% CI 0.51 to 0.74]. Average number of days with plt count <10 and <20×109/L was significantly longer in no-prophylaxis arm.
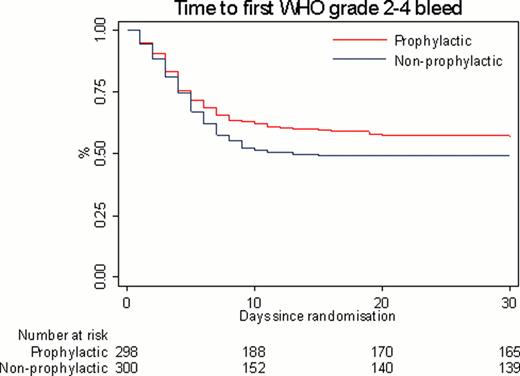
A WHO grade 2–4 bleed occurred in 151/300 patients (50%) in the no-prophylaxis group compared to 128/298 (43%) in the prophylaxis group (adjusted difference in proportions 8.4%, 90% CI 1.7 to 15.2%: p-value for non-inferiority 0.06). This study therefore did not prove its main aim, that a no-prophylaxis policy is non-inferior to prophylaxis. The time to the first grade 2–4 bleed was significantly shorter in the no-prophylaxis group (Fig. 1). Patients in the no-prophylaxis group averaged 1.7d (SD 2.9) with a WHO grade 2–4 bleed during follow-up, vs. 1.2d (SD 2.0) in the prophylactic group [rate ratio 1.52, 95% CI 1.14 to 2.03]. Whilst there were more grade 3–4 bleeds in the no-prophylaxis group (6/300) compared to the prophylaxis group (1/298) this did not reach statistical significance (OR 6.05, 95% CI 0.73 to 279.72, p = 0.13). Only 2 of these 7 patients had a plt count <10×109/L at onset of grade 3–4 bleeding (median plt count 16, range 3–42 x109/L); both patients were receiving induction chemotherapy for AML. Pre-defined subgroup analysis between autoSCT vs other treatments for the primary outcome found a significant interaction (p-value 0.04). In the autoSCT group, WHO grade 2–4 bleed grade occurred in 99/210 patients (47%) in the no-prophylaxis group vs 95/210 (45%) in the prophylaxis group (difference in proportions 2.3%, 90% CI −5.7 to 10.3%).
For all patients, there was no significant difference between treatment groups in period of thrombocytopenia, number of days in hospital, or number of SAEsexperienced.
This multicenter study has not shown that a no-prophylaxis PltTx policy is non-inferior to prophylaxis. Patients in the no-prophylaxis group had more days with a WHO grade 2 or above bleed, and a shorter time to first bleed. Further analysis is needed to determine whether these findings apply to all subgroups of patients. Despite a role for prophylactic platelet transfusions, rates of bleeding in patients remain high.
NHS Blood and Transplant & Australian Red Cross Blood Service
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal