Abstract
Abstract 1140
Current estimates on mortality after venous thromboembolism (VTE) are limited and are based largely on randomized clinical studies with select populations of relatively health patient groups.
We estimated the mortality following a first VTE event in the general population, and compared survival rates among patients with idiopathic, cancer-associated, and secondary non-cancer associated VTE.
This retrospective, observational study used the linked administrative healthcare databases of the province of Québec, Canada, including the province-wide hospitalization database (MED-ÉCHO), the healthcare services database of RAMQ which is a governmental agency that administers the Québec universal healthcare program and oversees all physician reimbursement claims, and the vital statistics database of the Institut de la Statistique du Québec (ISQ). From a source population of all RAMQ beneficiaries with a physician visit or a hospitalization associated with an ICD-9-CM or ICD-10-CA diagnosis code for deep vein thrombosis (DVT) or pulmonary embolism (PE) recorded between January 1, 2000 and December 31, 2009 and without a DVT or PE code prior to January 1, 2000, we identified a cohort of Québec residents with definite incident VTE and a cohort with definite or probable incident VTE. We used a priori determined diagnostic algorithms using RAMQ and MED-ÉCHO data to identify definite and probable cases of VTE. Subjects were followed forward in time from fist-time VTE occurrence until the earliest of either death or end of study period (December 31, 2009). Death was identified from MED-ÉCHO and ISQ. Thirty-day and 1-year case-fatality rates and associated 95% confidence intervals (CI) for VTE, DVT alone, and PE with or without DVT were calculated using all-cause deaths as the numerator and the number of patients with VTE as the denominator. Kaplan Meier curves were used to represent crude survival following a VTE episode, stratified by VTE risk factor group (idiopathic, cancer-associated, and secondary). The log-rank test was used to determine the significance of differences in the survival curves.
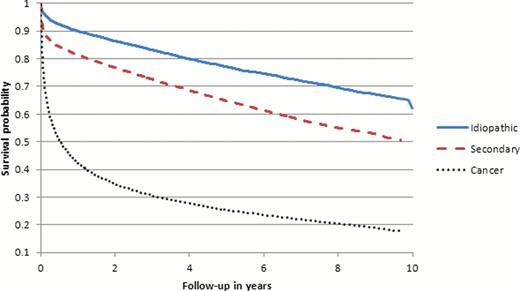
From the 245 452 Québec residents between 2000 and 2009 with at least 1 VTE diagnosis in RAMQ or MED-ÉCHO, we identified 67 410 cases with definite VTE, and an additional 35 123 cases with probable VTE. The cohort of definite VTE included 56% women, 46.5% patients aged 70 years or older, and 28.3% idiopathic VTE cases. The cohort of definite or probable VTE also included 56% women, 42.3% patients aged 70 years or older, and 34% idiopathic VTE cases. In the year following the VTE event, 14 407 (30%) deaths occurred in the definite VTE cohort, and 15 395 (25%) in the definite or probable VTE cohort. Among definite VTE cases, the 30-day case fatality rate was 14.1% (95% CI: 13.9–14.4), and the 1-year case fatality rate was 29.2% (95% CI: 28.9–29.6). The corresponding rates in the definite or probable VTE cohort were lower with a 30-day and 1-year case-fatality rate of 10.61% (95% CI: 10.41–10.81) and 23.04% (95% CI: 22.77–23.31), respectively. The 30-day case fatality was almost 2-fold higher in patients with PE with or without DVT vs. patients with DVT alone (RR 1.92, 95% CI: 1.85–1.99), and this difference in mortality was less at 1 year (RR 1.20, 95% CI: 1.17–1.23). The Kaplan-Meier overall survival plot showed a 1-year survival rate of 42% (95% CI: 41–43%) among definite VTE cases with cancer (Figure 1). The 1-year survival rates following definite VTE in patients with idiopathic and secondary VTE were different (90% vs. 81%, respectively; p<0.0001). Similar survival rates were observed in the definite or probable VTE cohort.
In a large unselected general population, VTE is associated with a high mortality and patients with PE are at a higher risk of death than patients with DVT alone. Among cancer patients with VTE, long-term survival remains poor. The observed lower survival in patients with secondary VTE as opposed to idiopathic VTE may be explained by the advanced age of our patient population. These data highlight the need for optimization of current VTE treatment strategies, especially in cancer patients.
Kaplan-Meier overall survival probability after first definite venous thromboembolism (VTE) in the risk groups of idiopathic VTE, secondary non-cancer VTE (secondary), and secondary to cancer VTE (cancer)
Kaplan-Meier overall survival probability after first definite venous thromboembolism (VTE) in the risk groups of idiopathic VTE, secondary non-cancer VTE (secondary), and secondary to cancer VTE (cancer)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal