Abstract
Previous studies have documented the underrepresentation of women and elderly patients in American clinical trials of leukemia. If, characteristics of patients included in clinical protocols differ markedly from the characteristics of the majority of patients treated outside protocols the external validity of clinical trials may be threatened.
The Danish National Acute Leukaemia Database (ALDB) includes detailed data on a large well-defined non-selected population of 2729 AML patients (covering >95% of AML patients diagnosed since Jan 2000). Since 2000 Danish AML patients have been included in 3 different British protocols (AML15, 16 and 17).
We analysed a cohort of 2624 patients diagnosed with AML in Denmark since Jan. 2000 (105 APL-patients were excluded). We compared patients treated with curative intent according to the British protocols with patients treated with curative intent off-protocol with regard to characteristics, possible prognostic factors, CR-rate, and survival. For comparable groups we divided patients into 2 age groups (<60 and ≥60 years) and further excluded patients diagnosed before protocol inclusion was possible for the given age group.
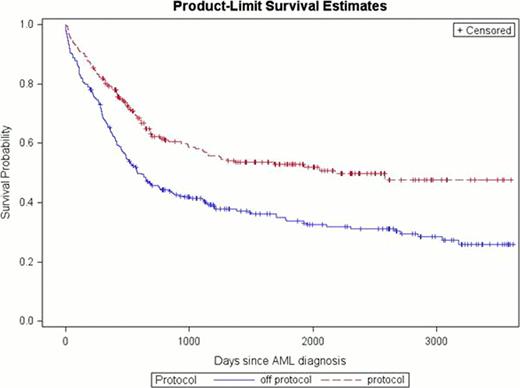
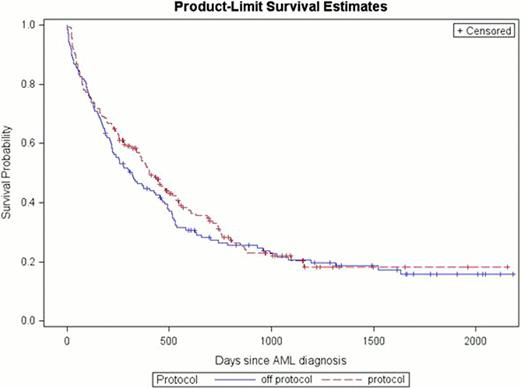
813 patients were treated with curative intent (517 pts < 60 years (96% of all patients <60y) vs. 296 pts ≥60 year, (35 % of all patients >60y). Of these, 391 pts (232 pts <60 years, 44.9 % vs. 159 pts ≥60 years, 53.7 %) were treated according to protocols. For both age groups WHO performance status score (WHO PS) was found to be significantly lower in the on-protocol group. Presence of secondary AML (sAML) was found more frequent in the off-protocol groups, but was only statistically significant in the group under 60 years. In patients 60 years or older, a significantly higher LDH-level and WBC was found in the on-protocol groups. We did not find any difference in distribution of sex, age, cytogenetic changes, presence of extra medullary leukemia (EML) or blast counts. Allogeneic transplantation (alloHCT) was significantly more often performed in the protocol groups (table 1). For patients under 60 years of age overall survival (OS) was superior in the on-protocol group (fig. 1). For the older age group OS was similar in the on- and off-protocol group (fig. 2). After controlling for possible prognostic factors protocol participation seemed to be associated with longer OS in patients under 60 years (HR 0.66, 95%CI 0.48–0.99, p=0.02), but not in patients 60 years or older (HR 1.17, 95%CI 0.87–1.57). The unevenly distributed characteristics; LDH-level, sAML, WHO PS, performance of alloHCT were all found to be of significant importance to OS.
AML patients included in the British AML trials in Denmark had a more favorable profile than patients treated with standard regimens. We found a superior survival in on-protocol patients under 60 years. This could not be fully explained by an uneven distribution of prognostic factors. A beneficial effect of the protocol treatments and confounding by co-morbidity are suggested. Population-based studies may thus have an important role in examining some aspects of prognosis in AML. In this context the Danish ALDB has proven to be a valuable data source.
Clinical and demographic characteristics of 813 AML patients
| . | . | Age < 60 years n =517 . | . | Age ≥60 years n = 296 . | ||
|---|---|---|---|---|---|---|
| . | Protocol n=232 . | Off-protocol n = 285 . | p-value* . | Protocol n = 159 . | Off-protocol n= 137 . | p-value* . |
| Age, median (range) | 47 (18–59) | 49 (15–59) | NS | 67 (60–78) | 66 (60–83) | NS |
| Sex, male % | 51.7 | 49.5 | NS | 59.8 | 60.6 | NS |
| sAML (%) | 18 (7.7) | 71 (24.9) | <.0001 | 42 (26.4) | 49 (35.8) | 0.08 |
| Cytogenetics, (%) | 0.096 | 0.14 | ||||
| Favorable | 18 (8.3) | 14 (5.5) | 2 (1.3) | 0 (0) | ||
| Intermediate | 164 (75.9) | 185 (73.1) | 113 (74.3) | 102 (81.0) | ||
| Adverse | 34 (15.7) | 54 (21.3) | 37 (24.3) | 24 (19.1) | ||
| WHO PS (%) | <0.001 | 0.04 | ||||
| 0 | 118 (51.3) | 98 (34.8) | 68 (42.8) | 48 (35.0) | ||
| 1 | 91(39.6) | 124 (44.0) | 73 (45.9) | 59 (43.1) | ||
| 2 | 16 (7.0) | 43 (15.3) | 9 (5.7) | 20 (14.6) | ||
| 3 | 3 (1.3) | 11 (3.9) | 5 (3.1) | 6 (4.4) | ||
| 4 | 2 (0.9) | 6 (2.1) | 4 (2.5) | 4 (3.0) | ||
| EML (%) | 33 (14.2) | 44 (15.4) | NS | 18 (11.3) | 12 (8.8) | NS |
| Median WBC (%) | 11 (0.6–269) | 12.2 (0.1–359) | NS | 7.38 (0.2–355) | 19.1 (0.40–507) | <0.002 |
| Median blast Count, bone marrow (range) | 60 (0-100) | 62 (0-100) | NS | 51 (2-98) | 51(1-100) | NS |
| Median LDH (range) | 399 (63-12742) | 410 (105-10596) | NS | 299 (93-2500) | 496 (116-15900) | <0.001 |
| CR-rate (%) | 78.9 | 75.4 | NS | 57.9 | 60.6 | NS |
| AlloHCT (%) | 32.3 | 22.1 | 0.009 | 14.5 | 4.4 | 0.003 |
| . | . | Age < 60 years n =517 . | . | Age ≥60 years n = 296 . | ||
|---|---|---|---|---|---|---|
| . | Protocol n=232 . | Off-protocol n = 285 . | p-value* . | Protocol n = 159 . | Off-protocol n= 137 . | p-value* . |
| Age, median (range) | 47 (18–59) | 49 (15–59) | NS | 67 (60–78) | 66 (60–83) | NS |
| Sex, male % | 51.7 | 49.5 | NS | 59.8 | 60.6 | NS |
| sAML (%) | 18 (7.7) | 71 (24.9) | <.0001 | 42 (26.4) | 49 (35.8) | 0.08 |
| Cytogenetics, (%) | 0.096 | 0.14 | ||||
| Favorable | 18 (8.3) | 14 (5.5) | 2 (1.3) | 0 (0) | ||
| Intermediate | 164 (75.9) | 185 (73.1) | 113 (74.3) | 102 (81.0) | ||
| Adverse | 34 (15.7) | 54 (21.3) | 37 (24.3) | 24 (19.1) | ||
| WHO PS (%) | <0.001 | 0.04 | ||||
| 0 | 118 (51.3) | 98 (34.8) | 68 (42.8) | 48 (35.0) | ||
| 1 | 91(39.6) | 124 (44.0) | 73 (45.9) | 59 (43.1) | ||
| 2 | 16 (7.0) | 43 (15.3) | 9 (5.7) | 20 (14.6) | ||
| 3 | 3 (1.3) | 11 (3.9) | 5 (3.1) | 6 (4.4) | ||
| 4 | 2 (0.9) | 6 (2.1) | 4 (2.5) | 4 (3.0) | ||
| EML (%) | 33 (14.2) | 44 (15.4) | NS | 18 (11.3) | 12 (8.8) | NS |
| Median WBC (%) | 11 (0.6–269) | 12.2 (0.1–359) | NS | 7.38 (0.2–355) | 19.1 (0.40–507) | <0.002 |
| Median blast Count, bone marrow (range) | 60 (0-100) | 62 (0-100) | NS | 51 (2-98) | 51(1-100) | NS |
| Median LDH (range) | 399 (63-12742) | 410 (105-10596) | NS | 299 (93-2500) | 496 (116-15900) | <0.001 |
| CR-rate (%) | 78.9 | 75.4 | NS | 57.9 | 60.6 | NS |
| AlloHCT (%) | 32.3 | 22.1 | 0.009 | 14.5 | 4.4 | 0.003 |
Overall survival in patients under 60 years by protocol status
Overall survival in patients under 60 years by protocol status
Overall survival in patients 60 years or older by protocol status
Overall survival in patients 60 years or older by protocol status
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal