Abstract
Over the past 20 years, allogeneic hematopoietic cell transplantation (HCT) has been increasingly performed with peripheral blood stem cells (PB) and gained benefit from better HLA-typing. Similar long-term survival has been suggested after HLA-matched related and unrelated donor HCT. Till now, the optimal strategy for donor selection is still controversial. We evaluated the impact of donor type (10/10 HLA-matched unrelated (MUD) vs. matched related (MRD)) and other donor traits on long term outcomes of patients with hematologic malignancies after PB HCT.
We analyzed outcomes of 442 consecutive patients with hematologic malignancies who were transplanted with PB either from MUD (n= 164) or MRD (n=278) at our center from 01/2000 to 12/2010. Median patient age was 48 years (range 7–68). Diseases included 122 acute myelogenous leukemias, 62 non-Hodgkin lymphomas, 60 myelodysplastic syndromes, 57 multiple myelomas, 40 acute lymphoblastic leukemias, 37 myeloproliferative disorders, 29 Hodgkin diseases, 20 chronic myeloid leukemias and 15 chronic lymphocytic leukemias. Two-third of patients underwent HCT following reduced intensity conditioning. Graft-versus-host disease (GVHD) prophylaxis consisted mostly in cyclosporine plus MMF or methotrexate. ATG was used in 19% of HCT. We assessed the impact of donor factors (type, age, gender, CMV serologic status and ABO group) on chronic GVHD (cGVHD), relapse, non relapse mortality (NRM) and overall survival (OS). Concerning donor age, as the upper age limit for voluntary PB donation was usually 60 years, we completed our analysis by performing 3 groups according to donor type and age (MUD, MRD<60y and MRD≥60y) and evaluated their influence on outcomes.
Median donor age was 40 years (range 18–72). Most young donors were MUD (<30y: 70%) while older were mainly MRD (≥50y: 98%). Thirty-six patients were transplanted with MRD≥60y. The proportion of female donors was 42% and 113 HCT were performed from female donor to male recipient. Half of patients were transplanted from CMV seronegative donors. Donor/recipient pairs (D/R) were CMV status mismatched in 38% of cases. D/R were ABO matched, minor and major mismatched in 57%, 19% and 24% of cases. Considering donor type, MUD and MRD HCT were balanced for patient age, disease risk and conditioning. MUD received ATG more frequently than MRD (29% MUD vs. 14% MRD [10% MRD<60y and 25% MRD≥60y], P <.0001).
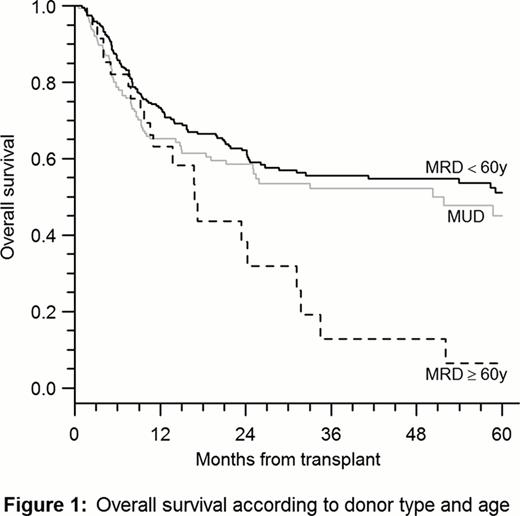
The median follow-up (FU) was 36 months (range 2–133) and 25% of patients had a FU of at least 60 months. The cumulative incidence (CIf) of cGVHD at 2 years was 58%. In multivariate analysis, sex mismatch (female > male) increased risk of cGVHD (HR: 1.41 [95% CI 1.05–1.88], P=.02) while MRD≥60y resulted in lower risk (HR: 0.48 [0.25–0.94], P=.031). Donor type by itself did not impact on cGVHD (58% with MRD and 59% with MUD). At 5 years, the CIf of relapse was 34% and was higher with MRD than MUD (39% vs. 24%, P=.038). Adjusted for disease risk, conditioning and infused cells count, only MRD≥60y resulted in significant higher risk of relapse than MUD (HR 2.41[1.26–4.62], P=.008) while MRD <60y had similar risk. The 5 years NRM was 26%. MUD vs. MRD was associated with higher NRM (HR: 1.84 [1.20–2.83], P=.005). Adjusted for recipient age, conditioning, and infused cells count, only MRD<60y were associated with lower risk of NRM than MUD (0.55 [0.35 to 0.86], P=.008) while MRD≥60y had similar NRM. OS was 46% at 5 years and was similar with MUD and MRD. Considering age, MRD≥60y appeared to have notable low OS at 5 years (6%, SE 6%). Adjusted for recipient age, disease risk and infused cells count, HCT from MRD≥60y was associated with higher risk of late (≥18 months) mortality (HR: 4.44 [1.53–12.9], P=.006) than MUD (Fig. 1).
Donor/recipient gender parity, donor type and age appeared as significant predictive factors of long term outcomes after HLA-matched PB HCT. Nor donor CMV status nor ABO group seemed to impact on outcomes in our cohort. The selection of a sex mismatched donor (female>male) was associated with significant higher risk of cGVHD. Using PB as graft source, HLA 10/10 MUD provided higher NRM but better disease control and similar OS than MRD. Having combined donor type and age, we observed notable poor outcome (high relapse rate and low OS) for patients transplanted with MRD≥60y in our cohort. Given those results, one may question HCT with old MRD when a younger MUD is available.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal