Abstract
Abstract 235
The RESORT trial (E4402) found comparable time to treatment failure (TTTF) and disease-related outcomes in previously untreated, indolent, follicular lymphoma randomized to maintenance rituximab (MR) versus rituximab retreatment (RR), and possible benefit of MR for patients with non-follicular lymphoma. The effects of MR versus RR on patient anxiety and health-related quality of life has not previously been examined.
Pt received R 375 mg/m2 weekly × 4 and responders were randomized to MR (single dose R q 3 mo) or RR (R weekly × 4 at disease progression). Each strategy was continued until treatment failure. Participants enrolled after 5/2005 completed a patient-reported outcomes (PRO) assessment. Patient preferences regarding treatment were measured at randomization using 4 patient self-report items developed for this trial. These 4 items asked patients to rate the extent to which medical visits and cancer treatment reduces their anxiety and increases perceived control, and the extent to which they prefer to avoid medical care due to an increase in anxiety in response to reminders of illness. Participants were categorized based on their responses as using “active coping” (medical care decreases anxiety) or “avoidant coping” (prefer to avoid medical care). Participants completed PRO assessment following R induction at randomization, 3, 6, 12, 24, 36, and 48 months post-randomization, and at R failure. PRO assessment included standardized, validated questionnaires to measure general anxiety and depression (Hospital Anxiety and Depression Scale, HADS), post-traumatic stress-type anxiety (Impact of Events Scale-Revised, IES-R), and health-related quality of life (Functional Assessment of Cancer Therapy–General, FACT-G). Individual items were selected from existing measures or were developed for this trial to assess illness-specific anxiety about the future (Illness Impact). Primary PRO analysis compared change scores from randomization-12 months between MR and RR treatment arms. Differences between participants categorized as using active or avoidant coping were also examined.
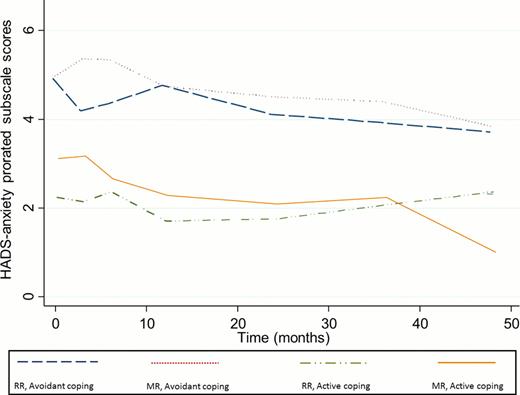
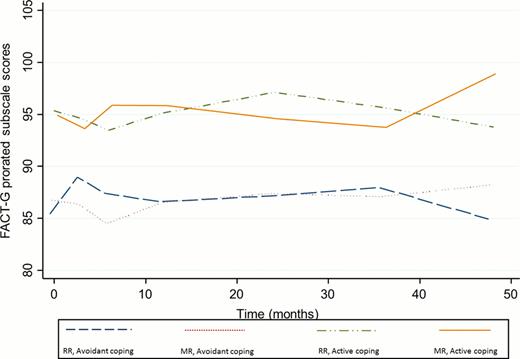
253 patients (92% of E4402 randomized sample) completed PROs at randomization. 125 patients were randomized to MR and 128 were randomized to RR. Demographic and disease characteristics were comparable between arms. Median age 60 years, 54% female, 95% White. All patients PS 0–1; 83% follicular lymphoma, 17% non-follicular. The study had 80% power to detect an effect size of 0.4 for the primary endpoint (change scores randomization to 12 months). There were no statistically significant differences between MR and RR on (1) any PRO measure and (2) PRO change scores from randomization to 12 month follow-up (p=NS). Figure 1 illustrates HADS Anxiety scores and Figure 2 shows FACT-G scores from randomization-48 months. The proportion of participants exceeding established clinical cut-off scores on the HADS Anxiety and IES-R did not differ between MR and RR. At randomization, 70% of participants were categorized as using an avoidant coping style and 30% as using active coping. Among participants using avoidant coping, 6–10% exceeded HADS Anxiety clinical cut-off at randomization, 3, 6, and 12 month assessments, and 16% at R failure. A lower proportion of those using active coping (0–3%) reported clinically significant anxiety at all time points (p<0.05). A higher proportion of avoidant coping patients exceeded IES-R clinical cut-off (10–18%), indicating greater post-traumatic anxiety than active coping patients (34%; p<0.01).
In previously untreated, indolent, non-Hodgkin's lymphoma, MR and RR are comparable with regard to patient-reported anxiety, post-traumatic anxiety, illness-specific anxiety about the future, and overall HRQL. MR did not result in reduced anxiety or better HRQL compared to RR, even among patients who report that medical visits and ongoing treatment reduce anxiety (“active coping”). RR did not result in lower anxiety or better HRQL among patients who reported a preference to avoid medical visits due to increased anxiety (“avoidant coping”). Administration of R q 3 months was not associated with functional improvements or detriments to HRQL, indicating R is well-tolerated. For MR and RR, avoidant coping was associated with a higher likelihood of clinically significant general anxiety and post-traumatic anxiety.
•••.
•••.
Williams:Genentech: Membership on an entity's Board of Directors or advisory committees, Research Funding. Horning:Genentech: Employment. Kahl:Genentech: Consultancy, Research Funding; Roche: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal