Abstract
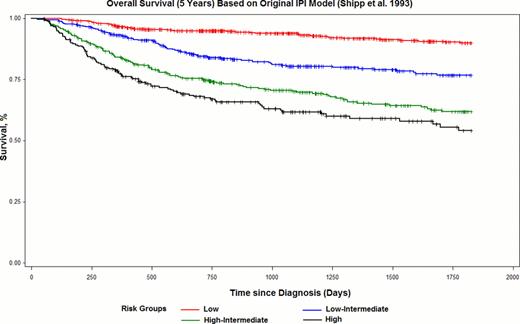
The International Prognostic Index (IPI) was first developed in 1993 to risk stratify patients with aggressive Non-Hodgkin's lymphoma (NHL) for outcome prediction (Shipp, NEJM, 1993). Since the addition of rituximab to conventional CHOP chemotherapy for the treatment of DLBCL, there have been many efforts to validate the IPI as well as to improve upon the model's capacity to distinguish subgroups with discrete clinical outcomes, especially high-risk patients. Previous studies have focused on adding clinical or biologic prognostic factor(s) to the original model or regrouping the original IPI score (R-IPI; Sehn, Blood, 2007). We, therefore, built anew a modern IPI based solely on clinical factors available in the real world NCCN clinical database.
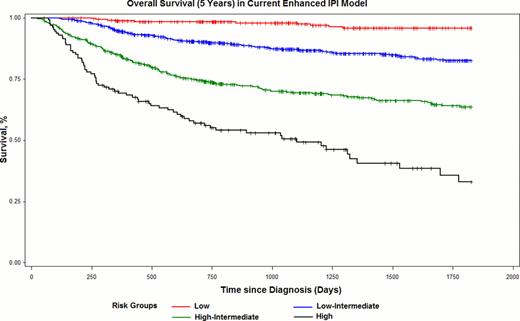
Using the nationwide population-based NHL lymphoma database from NCCN, patients with newly diagnosed DLBCL enrolled between June 2000 and Dec. 2010 at 7 NCCN cancer centers were included with at least 1 year and up to 5 years of follow-up. Clinical characteristics including age, Ann Arbor stage, ECOG performance status, disease in extranodal sites (including positivity in bone marrow, CNS, liver/GI tract, lung, other sites and spleen), LDH, presence of bulky disease (>10 cm) as well as B symptoms were studied as potential predictors for model development using COX proportional hazards regression. IPI scores were assigned proportionally based on parameter estimates of the statistically significant predictors in the final COX model. Model selection and its comparison to the original IPI model were made based on Akaike Criteria (AIC) and the likelihood ratio test. Categorization of age and LDH was decided by testing the linearity assumption and Martingale residuals. Kaplan-Meier curves were plotted for stratified risk groups per the new and original IPI. Finally, both IPI models were compared using the initial randomly selected 15% validation sample.
There were 1,650 DLBCL patients with complete clinical information included for model development. The new IPI model consisted of similar component predictors but used a maximum of 8 scoring points by further categorizing age group into >40–60 (score of 1), >60–75 (score of 2) and >75 yrs (score of 3), and normalized LDH between >1–3 times (score of 1) and 33 times (score of 2) upper limit of normal. These categorizations minimized the Martingale residuals. Age effect was linear and 20-year increments fit the model best, whereas the effect of normalized LDH was not linear and reached plateau at a ratio of 3. Lymphomatous involvement either of bone marrow, CNS, Liver/GI tract or lung appeared as a stronger predictor (p<0.001) than number of extranodal sites (p=0.91). Four risk groups (Low, Low-intermediate, High-intermediate and High) were identified using the current IPI (Table 1) with enhanced discrimination power when compared with the original IPI and better global model fitting statistics, i.e. smaller AIC and significant likelihood ratio test (p<0.001). It was possible to identify a high risk group (score 3 6) with 5-year overall survival of 33% (95% CI: 22%–45%). Better model prediction was also shown in the validation sample.
We were able to develop an enhanced IPI model for clinical prediction among previously untreated DLBCL cases by using patient level data from the NCCN NHL database. The NCCN-IPI demonstrates better risk stratification and identifies a poor risk subgroup with <50% 5-year overall survival in the current real-world clinical setting as compared to the original IPI model developed for aggressive lymphoma prior to the rituximab era.
An Enhanced IPI Score and Comparison of IPI Models Using Current NCCN DLBCL Data
| NCCN Prognostic Index (NCCN IPI) for DLBCL . | |||
|---|---|---|---|
| Score* . | Complete Response . | 5-y PFS . | 5-y OS . |
| 0–1 (19%)** | 93% | 91% | 96% |
| 2–3 (42%) | 88% | 74% | 82% |
| 4–5 (31%) | 75% | 51% | 64% |
| 3 6 (8%) | 65% | 30% | 33% |
| Original International Prognostic Index (IPI) for Aggressive NHL | |||
| 0–1 (38%) | 91% | 85% | 90% |
| 2 (26%) | 82% | 66% | 77% |
| 3 (22%) | 75% | 52% | 62% |
| 4–5 (14%) | 73% | 39% | 54% |
| * Calculation of Score: | |||
| Factors (NCCN IPI) | Score | ||
| Age | |||
| > 40 to £ 60 | 1 | ||
| > 60 to £ 75 | 2 | ||
| > 75 | 3 | ||
| LDH, normalized† | |||
| >1 to £ 3 | 1 | ||
| > 3 | 2 | ||
| Stage III/IV | 1 | ||
| Extranodal Site†† | 1 | ||
| Performance status 3 2 | 1 | ||
| NCCN Prognostic Index (NCCN IPI) for DLBCL . | |||
|---|---|---|---|
| Score* . | Complete Response . | 5-y PFS . | 5-y OS . |
| 0–1 (19%)** | 93% | 91% | 96% |
| 2–3 (42%) | 88% | 74% | 82% |
| 4–5 (31%) | 75% | 51% | 64% |
| 3 6 (8%) | 65% | 30% | 33% |
| Original International Prognostic Index (IPI) for Aggressive NHL | |||
| 0–1 (38%) | 91% | 85% | 90% |
| 2 (26%) | 82% | 66% | 77% |
| 3 (22%) | 75% | 52% | 62% |
| 4–5 (14%) | 73% | 39% | 54% |
| * Calculation of Score: | |||
| Factors (NCCN IPI) | Score | ||
| Age | |||
| > 40 to £ 60 | 1 | ||
| > 60 to £ 75 | 2 | ||
| > 75 | 3 | ||
| LDH, normalized† | |||
| >1 to £ 3 | 1 | ||
| > 3 | 2 | ||
| Stage III/IV | 1 | ||
| Extranodal Site†† | 1 | ||
| Performance status 3 2 | 1 | ||
LDH value divided by institutional upper limit of normal
Extranodal sites in either bone marrow, CNS, liver/GI or lung
Percent of cohort
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal