Abstract
Abstract 3241
Loss of cardiac beat to beat variability reflected by high frequency power (HFP) is a strong predictor of death in patients with cardiovascular disease. Similar autonomic dysfunction is found in patients with Sickle Cell Anemia (SCA) and can be induced by a 30 second period of hypoxia during five breath nitrogen exposure (1,2). Some data suggest that Sickle Cell Trait (SCT) carriers also exhibit autonomic dysfunction. In light of the recent attention to sudden death in young athletes with SCT we examined the autonomic response to transient hypoxia and isometric exercise in subjects with SCT and matched controls.
Autonomic responses to hypoxia induced by a five-breath nitrogen exposure and intense isometric exercise resulting from handgrip to exhaustion were measured. Autonomic parasympathetic tone and sympathetic-vagal balance were measured using respiratory-adjusted time-varying heart rate variability (HRV). High frequency power (HFP) reflects parasympathetic tone and low-high ratio (LHR), sympathetic-vagal balance (1,2).
Ten African American SCT carriers (7 female, 35.7 yrs + 2.8) and 11 age, and ethnicity matched controls (CTRL, 8 female, 30.5 yrs + 2.8) were studied. No difference in resting heart rate (HR, SCT 67.1 + 5.1, CTRL 65.9 + 5.5), cardiac output (CO, SCT 6.17 + .57, CTRL 7.31 + .52), mean arterial pressure (MAP, SCT 101.49 + 4.61, CTRL 101.49 + 4.96) or LHR (SCT, 1.16 + .38, SCT 1.44 + .37) was observed.
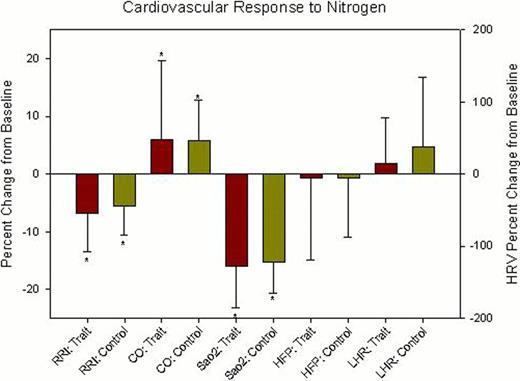
Five-breath nitrogen exposure produced nearly identical minimal arterial saturation (SaO2, SCT 84.1% ± 1.3%, CTRL 83.1% ± 1.3%) with compensatory tachycardia (DRRI, SCT −6.5% ± 1.2%, CTRL −4.79 ± 1.15%) and increased cardiac output (DCO, SCT 4.7% ± 1.7, CTRL 6.0% ± 1.6%). No change from baseline was observed in the population means of HFP or LHR for CTRLs or SCT subjects.
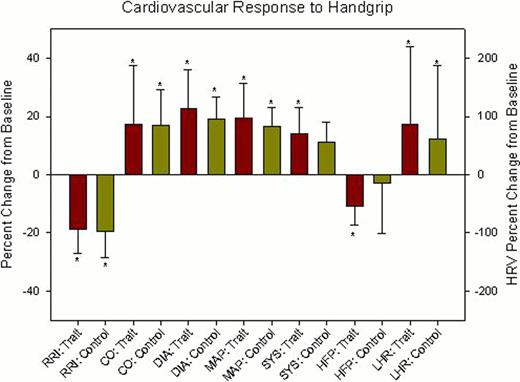
Following ten minutes of recovery, handgrip to exhaustion was performed at 60% maximum voluntary contraction. No differences were observed in maximum handgrip or duration between SCT and CTRL. Men produced higher maximal response but women maintained contraction nearly twice as long, independent of diagnosis. Handgrip exercise increased heart rate, cardiac output (SCT +13.4% ± 5.4%, CTRL +13.9% ± 5.0%), mean arterial pressure (SCT +19.6% ± 2.5%, CTRL +16.0% ± 2.3%), systolic pressure (SCT +14.6% ± 2.2%, CTRL +10.7% ± 2.1%), and diastolic pressure (SCT +22.5% ± 2.9%, CTRL +18.5% ± 2.6%). No population differences were observed in these responses. LHR increased similarly in both populations as well (SCT +78.9% ± 35.7%, CTRL +68.5% ± 32.9%), but SCT carriers had a much larger drop in HFP that was significantly different from baseline and trended lower than the control population (SCT −58% ± 18%, CTRL −9% ± 17%, p<.063).
Our laboratory has previously demonstrated hyper-reflexic parasympathetic withdrawal in response to transient hypoxia in patients with SCA (1,2). SCT subjects did not demonstrate parasympathetic withdrawal to hypoxia. However, we found exaggerated parasympathetic withdrawal in response to handgrip exercise in SCT subject and not in matched controls. Even though the biophysical properties of the sickle trait red cell are not sufficient to result in major hemolysis or vaso-occlusion, they are sufficient to alter autonomic balance. It will be important to determine whether this response impacts the distribution of ventricular repolarization, potentially increasing risk of arrhythmia, or is reproduced in other autonomic axes such as mental stress.
Cardiovascular and autonomic response to five breath nitrogen protocol. *statistically significant change from baseline (p<.05).
Cardiovascular and autonomic response to five breath nitrogen protocol. *statistically significant change from baseline (p<.05).
Cardiovascular and autonomic response to handgrip exercise to exhaustion. *statistically significant change from baseline (p<.05).
Cardiovascular and autonomic response to handgrip exercise to exhaustion. *statistically significant change from baseline (p<.05).
Coates:Apopharma: Consultancy; Novartis: Speakers Bureau. Wood:Novartis: Honoraria, Research Funding; Apotex: Consultancy, Honoraria; Shire: Consultancy; Ferrokin Biosciences: Consultancy.
References
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal