Abstract
Abstract 3319
An unpredictable subset of patients (∼20–30%) with pediatric immune thrombocytopenia (ITP) progress to chronic ITP; this increases the risk of morbidity and mortality from bleeding, long-term immunomodulation, and/or splenectomy. Furthermore, treatments such as chronic steroid therapy often result in intolerable side effects, raising the need for targeted therapies. We previously tested a novel list of genes that might predict progression to chronic ITP (Zhang et al Blood 2011). Oxidative stress (OS)-related pathways were among those most significantly perturbed in chronic ITP. For further evaluation of the role of OS in ITP, we measured glutathione as a marker of redox capacity and protein carbonyl content as a marker of oxidative cell damage.
Pediatric patients with primary ITP were included, with exclusion of subjects with secondary thrombocytopenia, other autoimmune disorders (ie, lupus), or other chronic illnesses. Healthy pediatric volunteers were recruited as controls. Patients had blood draws within 1 month from ITP diagnosis. Reduced (GSH) to oxidized (GSSG) glutathione ratios were measured from whole blood by tandem mass-spectrometry. Protein carbonyl content (PCC) levels were measured from platelet-rich plasma by enzyme-linked immunosorbent assay (ELISA). Subjects were followed up to 15 months from diagnosis and monitored for disease resolution or progression. Chronic ITP was defined as thrombocytopenia (platelets <100,000/μL) lasting at least 12 months from diagnosis (Rodegheiro et al Blood 2009). Acute ITP was defined as thrombocytopenia resolving within 12 months from diagnosis. Statistical significance was defined as p<0.05.
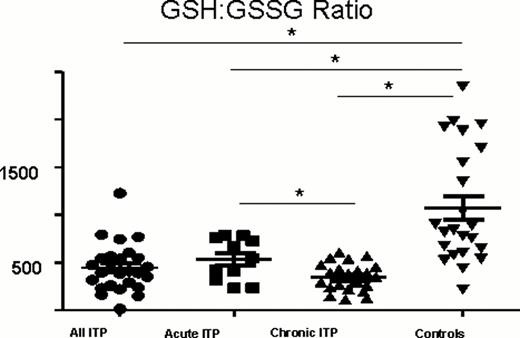
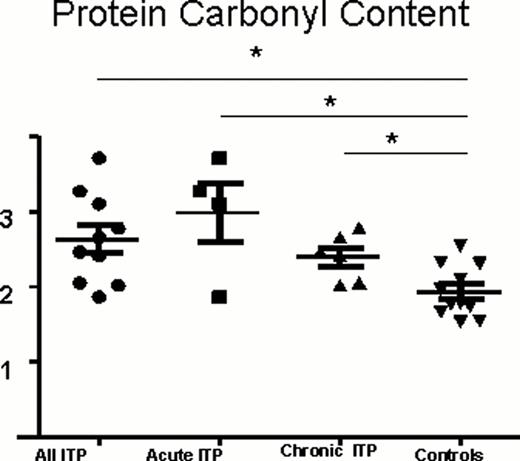
Between July 2009 and December 2011, 67 pediatric patients with ITP were recruited. Thirty-four patients had acute ITP, and 33 patients progressed to chronic ITP. The median age of patients was 7 years (range 18 months – 17 years). Sixty-three percent were female, 37% were male. Twenty-four pediatric controls were also recruited (46% female, 54% male). The median age of controls was 8 years (range 5 years – 17 years). Patients with ITP had significantly lower GSH:GSSG ratios compared to controls, and patients with chronic ITP had lower GSH:GSSG ratios compared to those with acute ITP (Figure 1). Furthermore, patients with ITP had significantly higher PCC levels compared to controls (Figure 2).
Glutathione ratios (GSH:GSSG) of ITP patients and normal controls. GSH and GSSG concentrations were measured in patients with acute ITP (Acute ITP, n=34), chronic ITP (Chronic ITP, n=33), and pediatric controls (n=24). GSH:GSSG ratios were calculated for each sample (mean + SEM). GSH:GSSG ratios are significantly lower in all ITP patients (All ITP= Acute ITP + Chronic ITP, p<0.0001) compared to controls. Furthermore, GSH:GSSG ratios are significantly lower in patients with chronic ITP compared to controls (p=0.0002), in patients with acute ITP compared to controls (p=0.0018), and in patients with chronic ITP compared to patients with acute ITP (p=0.0192).
Glutathione ratios (GSH:GSSG) of ITP patients and normal controls. GSH and GSSG concentrations were measured in patients with acute ITP (Acute ITP, n=34), chronic ITP (Chronic ITP, n=33), and pediatric controls (n=24). GSH:GSSG ratios were calculated for each sample (mean + SEM). GSH:GSSG ratios are significantly lower in all ITP patients (All ITP= Acute ITP + Chronic ITP, p<0.0001) compared to controls. Furthermore, GSH:GSSG ratios are significantly lower in patients with chronic ITP compared to controls (p=0.0002), in patients with acute ITP compared to controls (p=0.0018), and in patients with chronic ITP compared to patients with acute ITP (p=0.0192).
Protein carbonyl content (PCC) measurements of ITP patients and controls. PCC measurements were performed in patients with acute ITP (Acute ITP, n=7), chronic ITP (Chronic ITP, n=10), and pediatric controls (n=15). PCC levels are significantly higher in all ITP patients (All ITP= Acute ITP + Chronic ITP, p=0.0052) compared to controls. Furthermore, PCC levels are significantly higher in patients with chronic ITP compared to controls (p=0.0424), as well as in patients with acute ITP compared to controls (p=0.0261).
Protein carbonyl content (PCC) measurements of ITP patients and controls. PCC measurements were performed in patients with acute ITP (Acute ITP, n=7), chronic ITP (Chronic ITP, n=10), and pediatric controls (n=15). PCC levels are significantly higher in all ITP patients (All ITP= Acute ITP + Chronic ITP, p=0.0052) compared to controls. Furthermore, PCC levels are significantly higher in patients with chronic ITP compared to controls (p=0.0424), as well as in patients with acute ITP compared to controls (p=0.0261).
This data provides further evidence for a role of oxidative stress (OS) in the pathophysiology of ITP. Furthermore, decreased redox capacity, as evidenced by the decreased glutathione ratios, may be associated with progression to chronic ITP. Reactive oxidative species (ROS) may be important in the pathogenesis of autoimmunity in ITP; oxidatively altered cellular by-products induce pathogenic antibodies and become immunogenic. This also raises a potential anti-oxidant mechanism of therapy, which may play a greater role in chronic ITP treatment. Increased understanding of OS in pediatric ITP may reveal markers of disease progression, highlighting those at greatest risk for chronic ITP and creating a role for targeted therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal