Abstract
Abstract 3673
Very elderly pts (age > 75) with diffuse large B-cell lymphoma will increasingly be considered for cancer treatment as the population of the United States ages. However, such pts are under-represented in clinical trials, and standardized therapeutic algorithms are lacking. The impact of proliferation index (Ki67) and cell-of-origin are not well-studied in this group. For these reasons, and to inform the development of clinical trials, we retrospectively studied very elderly DLBCL pts since 2002.
The Oregon Health and Science University Tumor Registry was queried for all DLBCL cases treated since 2002. Those over 75 years of age were selected for in-depth study under IRB approval. Primary CNS lymphoma, unconfirmed diagnoses, and inadequate follow-up for survival were excluded. Baseline clinical and pathologic features (immunohistochemical, EBV [EBV-encoded RNA, EBER] staining, and translocations involving MYC and BCL2) were recorded. Outcomes including relapse/progression, treatment failure, and death (with cause of death), were analyzed using Kaplan-Meier modeling. Relapse-free survival (RFS) and disease-specific survival (DSS) were measured from diagnosis, censoring deaths not related to lymphoma or immediate therapy complications. Stage, LDH, performance status, disease bulk <10cm, renal failure at diagnosis, initial treatment (RCHOP vs. non-anthracycline), and IPI risk factors were assessed for an impact on outcome using JMP statistical software (SAS) and log-rank testing.
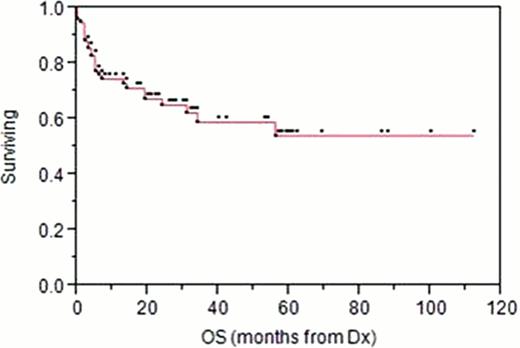
109 pts over the age of 75 were identified, 76 of whom fit above criteria. Median follow-up is 27 months. Pt characteristics are summarized in Table 1. Extra-nodal involvement was present in 57% of pts; sinus/orbit/ENT disease was seen in 26%. IPI factors were available for a fraction of pts, but an age-adjusted IPI (AA-IPI) of High-Int (2) or High (3) was identified in 15/32.
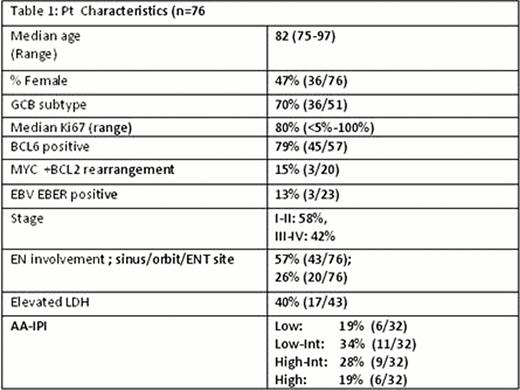
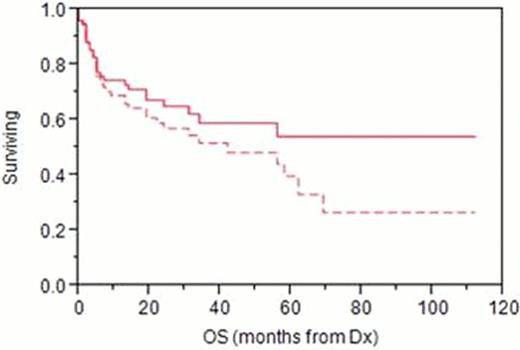
DSS/OS and RFS curves are shown in Figures 1 and 2. AA-IPI predicted DSS (p=.01). Neither Ki67 index (>80% vs. less) nor BCL6 positivity impacted DSS or RFS. Non-GCB cell-of-origin showed a trend toward poorer RFS (p=.09). > 1 extra-nodal site predicted poor DSS (p=.003) and RFS (p=.005); individually, stage, performance status, LDH, or renal failure at presentation were not prognostic.
RCHOP-like therapy (RCHOP, or REPOCH in 2 pts) was given to 59% (45/76), achieving a 5 year RFS of 60% (censoring non-lymphoma deaths) and OS of 50%. 14 RCHOP pts required a change in regimen due to toxicity, and 4 of these pts died during therapy. Non-anthracycline systemic therapy was administered to 14 (18%) pts, and included RCVP, RCEOP, RCOPP, and single agent R; though not statistically different from RCHOP in DSS or RFS, no evident plateau on the RFS curve was observed with such therapies. Finally, 8% (6) pts were treated palliatively; all died of lymphoma complications at a median of 4 months.
Salvage therapies included R+ chemo (4 pts), prednisone alone (1), rituximab alone (1), radiotherapy (4); median time from relapse to death was 8 months. Overall, 37 deaths have occurred, 27 due to lymphoma or immediate therapy complications.
Despite 4/45 treatment-related deaths and frequent changes to therapy, RCHOP affords long-term disease control in a proportion of very elderly pts. This suggests a regimen alternating RCHOP with other active agents can be tolerated and may produce the ideal balance of efficacy and safety in this pt population. High AA-IPI pts should be targeted for novel approaches, as pathologic biomarkers (Ki67, cell-of-origin by IHC) do not predict relapse or disease-specific survival outcomes. Further trials in this under-studied population are warranted.
Overall (Dashed line) and Disease-Specific Survival in 76 Very Elderly DLBCL Pts
Overall (Dashed line) and Disease-Specific Survival in 76 Very Elderly DLBCL Pts
Relapse-Free Survival among 76 Very Elderly DLBCL Pts
Spurgeon:Gilead: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal