Abstract
Abstract 4206
Relapse is the primary cause of treatment failure post alloHCT. We sought to identify risk factors that predict relapse of hematologic malignancies post-alloHCT to identify those at highest risk of relapse and help guide who may benefit from novel approaches to reduce relapse risk.
This was a single institution, retrospective cohort study of children with acute lymphoblastic leukemia, acute myelogenous leukemia, mixed phenotypic acute leukemia or myelodysplastic syndrome who had undergone alloHCT between 1/1/2003 and 12/31/2010. Relapse was defined as any evidence of increasing disease post-alloHCT, including minimal residual disease (MRD). Relapse-free survival (RFS) and associations with various characteristics were determined by the Kaplan-Meier method and log-rank test. The Cox proportional hazards model was used to identify factors that may jointly associate with RFS.
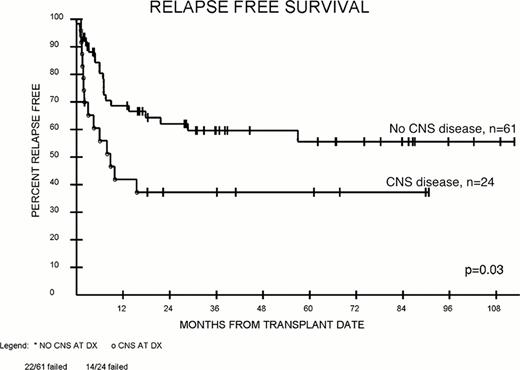
40 of 93 patients (43%) undergoing alloHCT experienced relapse at a median of 144 days (range 1 day – 58 months) post-HCT. Univariate actuarial analysis demonstrated that Black race (Figure 1), high white blood cell (WBC) count at diagnosis, central nervous system (CNS) disease at diagnosis (Figure 2), short first complete remission (CR1) duration (limited to those attaining CR1 with subsequent pre-HCT relapse), greater number of regimens given to induce remission, poorer performance status, non-myeloablative (NMA) preparative regimen, lack of remission and MRD pre-HCT were associated with higher relapse probability (Table 1). These factors were considered for inclusion in a Cox model; CNS disease at diagnosis (p=0.009), lack of morphologic remission (p=0.01) and a NMA HCT (p=0.04) were factors independently associated with worse RFS. 84 patients surviving to day 45 without relapse were included in a subset analysis to allow for incorporation of post-alloHCT factors that may modify relapse risk (i.e., graft-versus-host disease). When factors were considered jointly, only WBC at diagnosis was significantly associated with RFS. For patients in a morphologic remission who underwent a myeloablative HCT, MRD detection approximately doubled relapse risk. (Table 2).
The association of CNS disease at diagnosis with higher post-HCT relapse risk has not previously been reported. As a sanctuary site, the CNS may be less amenable to an allogeneic effect and CNS involvement might reflect higher-risk disease. Those with CNS disease may benefit from earlier or more intensive CNS-directed therapy to reduce relapse risk. The association of black race with increased relapse risk in the univariate analysis is also notable. For these patients, increased utilization of alternative donor sources or distinct biological differences may lead to higher relapse risk. Validation of these risk factors in a larger population and development of a prognostic score to identify those at highest risk of relapse is planned with possible prospective use of this prognostic tool in the development of relapse prevention trials.
Pre-HCT Patient Characteristics Associated with Post-HCT Relapse
| . | All (n) . | Patients without relapse during follow-up (n) . | Patients with relapse during follow-up (n) . | Log-rank p-value for comparison of Relapse Free Survival . | ||
|---|---|---|---|---|---|---|
| Total (n) | 93 | 53 | 40 | — | ||
| Race | Non-black | 76 | 47 | 29 | 0.03 | |
| Black | 17 | 6 | 11 | |||
| Disease | Acute lymphoblastic leukemia | 34 | 18 | 16 | Not significant | |
| Acute myelogenous leukemia | 41 | 23 | 18 | |||
| Mixed phenotypic acute leukemia | 10 | 6 | 4 | |||
| Myelodysplastic syndrome | 8 | 6 | 2 | |||
| At Diagnosis | White Blood Cell count | >65,000 | 18 | 7 | 11 | 0.04 |
| < 65,000 | 54 | 34 | 20 | |||
| Central nervous system disease | Yes | 24 | 10 | 14 | 0.03 | |
| No | 61 | 39 | 22 | |||
| Duration of first complete remission* | > 450 days | 19 | 12 | 7 | 0.06 | |
| < 450 days | 19 | 6 | 13 | |||
| # of induction regimens given to induce remission | 0 (MDS only) | 7 | 6 | 1 | 0.02 | |
| 1 | 27 | 19 | 8 | |||
| 2 | 36 | 18 | 18 | |||
| 3+ | 23 | 10 | 13 | |||
| At HCT | Morphologic Remission | Yes | 74 | 44 | 30 | 0.006 |
| No | 11 | 3 | 8 | |||
| Minimal residual disease | >0.01% | 34 | 14 | 20 | 0.015 | |
| < 0.01% | 50 | 32 | 18 | |||
| Performance status | 80–100% | 84 | 51 | 33 | 0.02 | |
| 40–70% | 8 | 2 | 6 | |||
| HCT Type | Myeloablative | 79 | 49 | 30 | 0.004 | |
| Non-Myeloablative | 14 | 4 | 10 | |||
| . | All (n) . | Patients without relapse during follow-up (n) . | Patients with relapse during follow-up (n) . | Log-rank p-value for comparison of Relapse Free Survival . | ||
|---|---|---|---|---|---|---|
| Total (n) | 93 | 53 | 40 | — | ||
| Race | Non-black | 76 | 47 | 29 | 0.03 | |
| Black | 17 | 6 | 11 | |||
| Disease | Acute lymphoblastic leukemia | 34 | 18 | 16 | Not significant | |
| Acute myelogenous leukemia | 41 | 23 | 18 | |||
| Mixed phenotypic acute leukemia | 10 | 6 | 4 | |||
| Myelodysplastic syndrome | 8 | 6 | 2 | |||
| At Diagnosis | White Blood Cell count | >65,000 | 18 | 7 | 11 | 0.04 |
| < 65,000 | 54 | 34 | 20 | |||
| Central nervous system disease | Yes | 24 | 10 | 14 | 0.03 | |
| No | 61 | 39 | 22 | |||
| Duration of first complete remission* | > 450 days | 19 | 12 | 7 | 0.06 | |
| < 450 days | 19 | 6 | 13 | |||
| # of induction regimens given to induce remission | 0 (MDS only) | 7 | 6 | 1 | 0.02 | |
| 1 | 27 | 19 | 8 | |||
| 2 | 36 | 18 | 18 | |||
| 3+ | 23 | 10 | 13 | |||
| At HCT | Morphologic Remission | Yes | 74 | 44 | 30 | 0.006 |
| No | 11 | 3 | 8 | |||
| Minimal residual disease | >0.01% | 34 | 14 | 20 | 0.015 | |
| < 0.01% | 50 | 32 | 18 | |||
| Performance status | 80–100% | 84 | 51 | 33 | 0.02 | |
| 40–70% | 8 | 2 | 6 | |||
| HCT Type | Myeloablative | 79 | 49 | 30 | 0.004 | |
| Non-Myeloablative | 14 | 4 | 10 | |||
Limited to those attaining a CR1 with subsequent pre-HCT relapse.
Relapse rates, by MRD, for those in a complete remission undergoing a myeloablative HCT
| Disease . | MRD >0.01% . | Total (n) . | Relapse (n) . | Relapse Rates . |
|---|---|---|---|---|
| Acute lymphoblastic leukemia | No | 20 | 7 | 35% |
| Yes | 11 | 7 | 64% | |
| Acute myelogenous leukemia | No | 16 | 3 | 19% |
| Yes | 11 | 4 | 36% | |
| Mixed phenotype acute leukemia | No | 8 | 3 | 38% |
| Yes | 1 | 0 | 0% |
| Disease . | MRD >0.01% . | Total (n) . | Relapse (n) . | Relapse Rates . |
|---|---|---|---|---|
| Acute lymphoblastic leukemia | No | 20 | 7 | 35% |
| Yes | 11 | 7 | 64% | |
| Acute myelogenous leukemia | No | 16 | 3 | 19% |
| Yes | 11 | 4 | 36% | |
| Mixed phenotype acute leukemia | No | 8 | 3 | 38% |
| Yes | 1 | 0 | 0% |
RFS by Race
RFS by CNS Disease at Diagnosis
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal