Abstract
Abstract  421
421
There are few therapies for thrombocytopenia in MDS, which is found in ∼50% of pts with low/int-1 MDS and is associated with shortened survival. In a June 2011 analysis of a 58-wk study (2:1 romiplostim:PBO), romiplostim reduced clinically significant bleeding events (HR 0.83, 95% CI: 0.66, 1.05, P = 0.13) and platelet transfusions (RR 0.77, 95% CI: 0.66, 0.88), and increased HI-P rates (OR 15.6, 95% CI: 4.7, 51.8). Increases in peripheral blast counts to >10% were more frequent with romiplostim (25/167, 15%) than PBO (3/83, 3.6%), and in most cases resolved after discontinuation. Through 58 wk, acute myeloid leukemia (AML) was diagnosed in 10 romiplostim pts (6.0%) and 2 PBO pts (2.4%) (HR 2.51, 95% CI: 0.55, 11.47); the differences for romiplostim vs. PBO 58-wk overall survival (OS) and AML-free survival were not statistically significant. This report updates the previous results, with a particular emphasis on AML incidence.
Eligible pts had IPSS low/int-1 MDS and were receiving supportive care, with platelets 1) ≤20×109/L or 2) ≤ 50×109/L with a history of bleeding. AML progression was defined as: 1) ≥20% blasts in the bone marrow or peripheral blood after 4 wk off romiplostim, 2) pathology consistent with leukemia (eg, chloroma or leukemia cutis), or 3) anti-leukemic treatment initiation. Due to data monitoring committee concerns that the potential small benefit seen in the reduction of bleeding did not outweigh the potential risk for disease progression to AML and that transient increases in blast cell counts may put pts at risk for diagnosis of and treatment for AML, study drug was stopped in February 2011. Pts were then moved into the long-term follow-up (LTFU) portion of the study. At the time of the 2011 analysis, not all pts had been on study 58 wk, thus the 58-wk data have been updated with LTFU data.
Results are presented by randomization group, although study drug was stopped in February 2011. Of 250 pts in the study (randomized 2:1 romiplostim:PBO), 224 entered LTFU, and 134 remained on study as of July 2012; the median (Q1, Q3) follow-up was 17.8 (10.8, 25.1) months. Through 58 wk, the proportions of deaths were romiplostim: 18.0% (30 pts), PBO: 20.5% (17 pts), for an OS HR of 0.86 (95% CI: 0.48, 1.56). Since June 2011, 2 additional AML cases were reported in the PBO arm which occurred within the 58-wk study period, but were not recorded in time for the primary analysis in 2011. Updated 58-wk AML rates were romiplostim: 6.0% (10 pts), PBO: 4.9% (4 pts), for an HR of 1.20 (95% CI: 0.38, 3.84). The resulting AML-free survival rates were romiplostim: 19.8% (33 pts), PBO: 22.9% (19 pts), for an HR of 0.86 (95% CI: 0.49, 1.51).
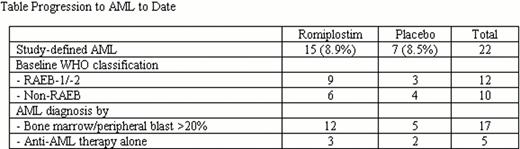
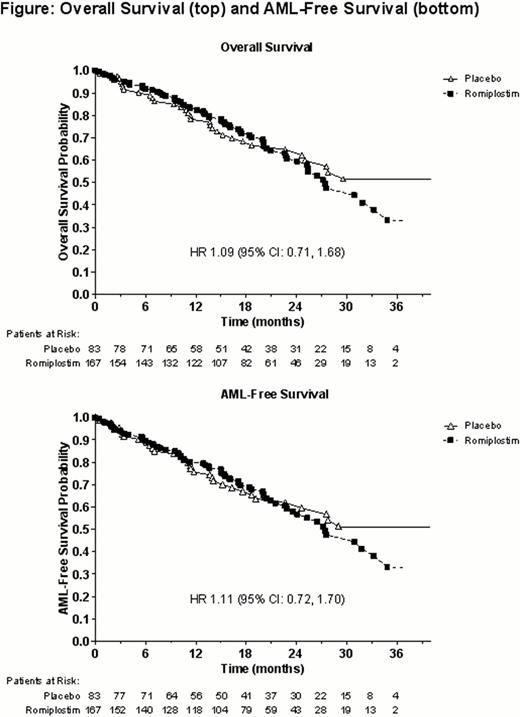
For data to date (beyond 58 wk), proportions of deaths were romiplostim: 38.3% (64 pts), PBO: 37.3% (31 pts), for an OS HR of 1.09 (95% CI: 0.71, 1.68). AML rates were romiplostim: 8.9% (15 pts), PBO: 8.5% (7 pts), for an HR of 1.15 (95% CI: 0.47, 2.85). The resulting AML-free survival rates were romiplostim: 39.5% (66 pts), PBO: 38.6% (32 pts), for an HR of 1.11 (95% CI: 0.72, 1.70) (Figure). Twelve of the 22 AML cases occurred in pts who were RAEB-1 and 5 cases were diagnosed by anti-AML treatment alone (Table). In LTFU, pt-reported rates of MDS therapy use (e.g., azacitidine, cyclosporine, and romiplostim) were romiplostim: 31.1%, PBO: 23.2%. Reported rates of AML therapy use (e.g., azacitidine and chemotherapy) were romiplostim: 6.0%, PBO: 7.2%.
A retrospective review of all available bone marrow aspirates and biopsies, including samples from pts diagnosed as having progressed to AML, was conducted by an independent hematopathologist; analyses are ongoing.
Following the 2011 decision to stop study drug, study results have been updated with more time on study. Specifically, with the additional AML cases in the PBO arm during the 58-wk study period and data from the LTFU period, the HRs for progression to AML were 1.20 and 1.15, respectively, in contrast with the finding of a year ago (HR of 2.51 for 58-wk). As LTFU continues, additional data will be evaluated. Safety concerns regarding risk of disease progression to AML are still being investigated.
Kantarjian:Amgen: Research Funding. Off Label Use: The use of romiplostim in MDS was examined in this trial. Mufti:Celgene: Consultancy, Research Funding. Fenaux:GlaxoSmithKline: Honoraria, Research Funding; Roche: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Membership on an entity's Board of Directors or advisory committees. Platzbecker:Amgen: Consultancy; GlaxoSmithKline: Consultancy; Celgene: Consultancy; Novartis: Consultancy. Kuendgen:Celgene: Honoraria. Gaidano:Amgen: Honoraria. Wiktor-Jedrzejczak:Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Bayer: Consultancy; Pfizer: Consultancy; Novartis: Consultancy, Speakers Bureau; Amgen: Consultancy; Janssen-Cilag: Consultancy; Celgene: Speakers Bureau; Genzyme: Speakers Bureau; Genopharm: Speakers Bureau. Bennett:Onconova: Consultancy; Amgen: Consultancy; GlaxoSmithKline: Consultancy; Ambit: Consultancy; Pfizer: Consultancy; Celgene: Consultancy. Meibohm:Merck: Employment, Equity Ownership; Amgen: Consultancy; Ockham: Employment. Yang:Amgen: Employment, Equity Ownership. Giagounidis:GlaxoSmithKline: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal