Abstract
Abstract 631
The antiphospholipid (aPL) syndrome (APS) is a diagnostic category that is defined by non-mechanistic empirically-derived assays - the lupus anticoagulant (LA) assay and aPL-antibody immunoassays for anticardiolipin and anti-ß2 glycoprotein-I antibodies. APS patients have heterogeneous antibodies and it is likely that several mechanisms are involved in the disease process. Annexin A5 (AnxA5) is a potent anticoagulant protein that forms 2-dimensional crystals over membranes that express phosphatidyl serine and shields the phospholipid from availability for phospholipid-depended coagulation reactions. We previously demonstrated that aPL antibodies can disrupt this crystallization and accelerate coagulation reactions. We therefore investigated whether disruption of AnxA5 anticoagulant activity might mark patients with histories for aPL antibody associated thrombosis.
We investigated samples from 966 adult patients from a large urban academic medical center with the following categories of histories: thrombosis, including venous thromboembolism (VTE) and stroke (n=433); pregnancy complications attributable to placental insufficiency (n=218); autoimmune disease (n=279); cancer (n=63); renal disease (n=101); liver disease (n=51); HIV (n=23); and free of known disease (n=140) (total >966 because of concurrent diagnosis). An assay that detects annexin A5 resistance (A5R) was performed on all samples. Results were expressed as “% AnxA5 anticoagulant activity”. A quintile analysis was performed to obtain cutoffs for A5R values. Values among groups were compared using student t-test, one way ANOVA and odds ratio analysis.
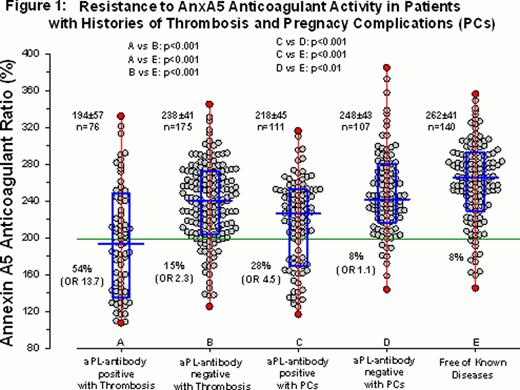
aPL-antibody positive patients with thrombosis (VTE and/or stroke) have significantly lower mean A5R values (194±57, n=76) than aPL-antibody negative patients with a thrombotic event (238±41, n=175; p<0.001) and from patients who are free of known disease (262±41, n=140; p<0.001, Figure 1). 54% (41/76) of patients in the aPL-antibody positive and thrombosis group had A5R values within the lowest quintile of results (<199%), in contrast to 15% (26/175) of the aPL-antibody negative and thrombosis patients and 8% (11/140) of the disease-free control. An AnxA5 anticoagulant activity of <199% was significantly associated with aPL-antibody positivity and thrombosis (OR: 13.7, p<0.001). aPL-antibody positive patients with pregnancy complications (PCs) have significantly lower A5R values (218±45, n=111) than aPL-negative patients with pregnancy complications (248±43, n=107; p<0.001) and from patients who are free of known disease (262±41, n=140; p<0.001, Figure 1). 28% (31/111) of patients in the aPL-antibody positive and pregnancy complication group had A5R values within the lowest quintile of results (<199%), in contrast to 8% (9/107) of the aPL-antibody negative and thrombosis patients and 8% (11/140) of the disease-free control. An AnxA5 anticoagulant activity of <199% was significantly associated with aPL-antibody positivity and pregnancy complications (OR: 4.6, p<0.001). There were no significant differences in AnxA5 anticoagulant activity in patients with cancer, HIV, and renal disease, however there were significantly lower A5R values in patients with autoimmune disease and liver disease. The latter appeared to correlate with severity of liver disease. Patients with triple aPL-antibody positivity or greater had significantly lower mean A5R values (155±48%, n=23, p<0.001), than patients with double positivity (193±55%, n=44, p<0.01), or single positivity (214±47, n=111, p<0.05). All aPL-positive groups had significantly lower A5R values than patients who were negative for aPL antibodies (240±43%, p<0.001).
A subset of ∼50% of aPL-antibody positive patients with thrombosis and ∼30% with pregnancy complications showed evidence for this mechanism - resistance to annexin A5 anticoagulant activity. The identification of specific mechanisms for aPL-antibody associated thrombosis and pregnancy complications offers the possibilities of improving diagnosis and developing targeted treatments for this enigmatic disorder.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal