Abstract
Abstract  643
643
Occurrence of Acquired Aplastic Anemia (AAA) in childhood is lower than in older ages so it is not easy to perform large studies on this rare disease in this particular age. Since the database of the SAA of the EBMT contains data on a relevant number of children with AAA we investigated the outcome of this disease in the age group 0 – 12 years. To this end we looked into the SAAWP EBMT database and evaluated overall survival (OS) and event free survival (EFS) in 563 patients aged 0–12 years (median follow-up 2.7, min 0- max 11.1 years) in terms of period of diagnosis (1990–1999, vs 2000–2009) and treatment (first line immunosuppressive therapy (IS) vs first line matched family donor (MFD) HSCT vs HSCT performed after failure of IS which is a miscellaneous group including transplants from mismatched unrelated (39%), matched unrelated (36%), matched family (19%) and mismatched family (6%) donors.
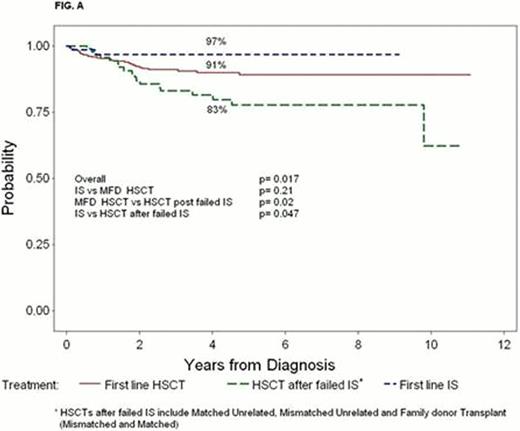
The 3 year probability OS and EFS for all patients were 90% and 86%, which was similar to results seen in period 1990–1990 (87% OS and 85% EFS). In the post-2000 period, 3 year OS after first line IS therapy was 97% vs 91 % for first line HSCT from MFD vs 83% of HSCT performed after having failed IS (p 0.017). The difference was not significant between front line IS and MFD HSCT (p 0.21) whereas MFD HSCT did significantly better than HSCT after failed IS (p 0.02). As expected OS for first line IS was significantly higher than that of HSCT after failed IS (p 0.047) (Fig A). Interval diagnosis-treatment ≤ or >2 months did neither affect OS nor EFS in the whole group.
EFS at 3 years after first line IS was 85 % vs 87 % for HSCT from MFD vs 81% of HSCT after failed IS (p ns).
Ac GVHD III-IV occurred in 26 % of MFD and in 26% of HSCT after failed IS. Chronic GVHD occurred in 4% of MFD and in 18% of HSCT after failed IS. BM as source of cells provided a significant advantage in OS and EFS over PB and CB. OS and EFS, were not significantly different in adolescents transplanted in adult centres vs mixed vs pediatric centres.
A total of 4 late tumors (0.7%) occurred at a follow-up of 2.7 years. One occurred after HSCT from MFD and 3 after HSCT for failed IS. In the whole cohort, Cox regression analysis did not show any impact of the type of treatment (IS, MFD HSCT and HSCT after failed IS) on either OS or EFS. In the group of transplanted patients BM as source of cells was associated with a better OS in both univariate and Cox regression analysis but had no significant effect on EFS.
Taken together these data indicate that front line IS is an excellent therapy for children with AAA, and that in case of failure of this treatment HCST is a very good salvage option. Given that HSCT is able to restore haematopoiesis more completely and more durably than IS, if a matched family donor is available the preference of front line HSCT over front line IS can be justified.
Dufour:Pfizer: Consultancy. Risitano:Alexion: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal