Abstract
Abstract 722
Very little is known about the cellular or molecular nature of pro-survival interactions between multiple myeloma (MM) and their bone marrow stromal hosts. CD28, the prototypical co-stimulatory molecule on T cells is overexpressed on MM relative to their normal counterparts. Clinical studies have independently shown that expression of CD28 or its ligand CD86 on myeloma cells portends poor survival in patients. We and others have shown that CD28 activation increases MM survival via NFkB accompanied by increased PI3K activity. Previously (ASH2010 and 2011), and since published, we have shown that myeloid dendritic cells (DC) form a vital part of the myeloma microenvironment, and myeloma cells interact with DC via a CD28-CD80/CD86 (B7) interaction. On the myeloma side, this interaction drives a CD28 mediated pro-survival signal, while on the DC side, it drives a B7 mediated induction of growth and immunosuppressive factors that modulate the MM survival niches in the bone marrow. In this work, we delineated key molecules downstream of CD28 that transduce the pro survival signal on the myeloma side as well as explored agents and strategies to target DC that help MM survive in the microenvironment. We also studied the role of DC IL-6 for MM survival in cocultures.
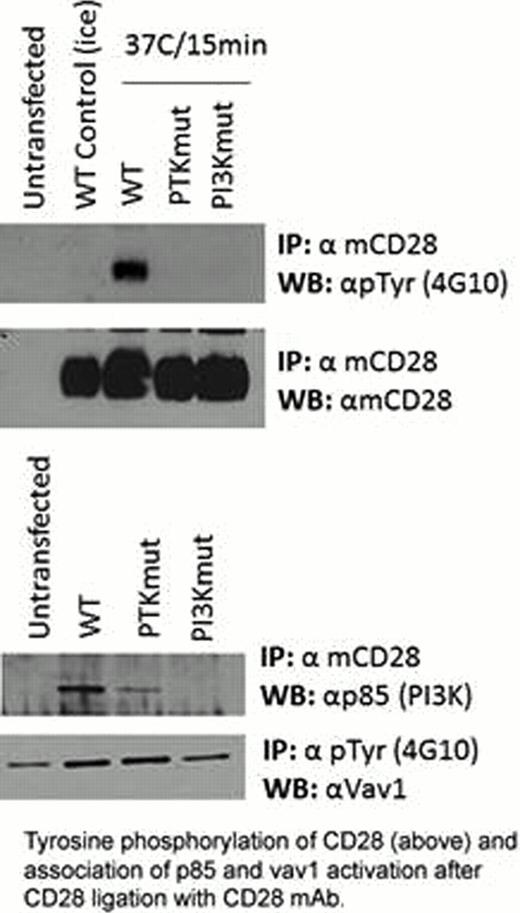
We have previously shown that CD28 activation by anti-CD28 mAb involves activation of the multifunctional pro-survival transcription factor NFkB accompanied by increased PI3K activity. Through immunoassays and radioactivity assays, using myeloma cell lines that were transfected with wild type murine CD28 (mCD28 differs only by 3 amino acids from human hCD28) and mutants for PI3K binding site YMNM, we show that the CD28 ligation with anti-mCD28 antibodies induces immediate tyrosine phosphorylation of mCD28 (just as observed by others in T cells), followed by binding of p85, the catalytic subunit of PI3K and activation of VAV1 (Fig 1). Association of p85 and VAV1 activation depended on an intact PI3K binding site on CD28's cytoplasmic tail. Our studies on how this signal is transduced show no involvement of GRB2 or SLP76 more traditionally associated with CD28 signaling. Moreover, silencing SLP76 using siRNA did not affect antibody mediated protection of MM cells against serum starvation. Activation of human CD28 with anti-CD28 mAb also up-regulated the basal tyrosine phosphorylation of human CD28 further just as observed in murine CD28.
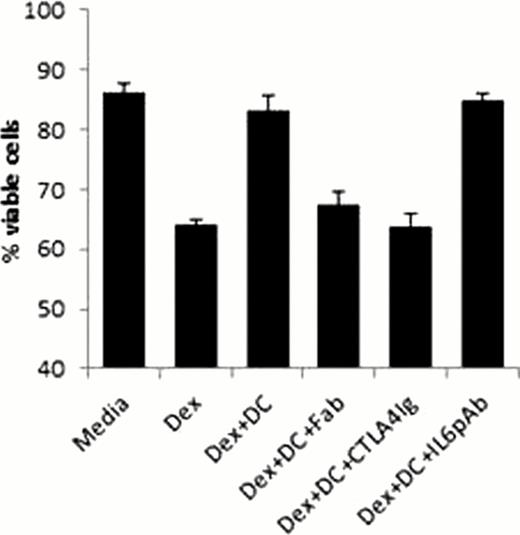
Through EMSAs, we also show that similar to what we have previously seen with activating antibodies, increase in NFkB activity was observed in myeloma cells when they were cocultured with DCs while being exposed to melphalan, but this spike did not dissipate in the presence of B7 blocking reagents such as CTLA4Ig (Abatacept®) suggesting a low threshold of CD28 activation. Next we tried using agents that have been known to modulate microenvironment such as lenalidomide, a novel drug that is currently used in combination with other chemotherapeutic agents such as dexamethasone and Bortezomib (Velcade®). Survival assays using flow cytometry, show that lenalidomide treated DCs provided significantly lower protection against cell death compared to wild type DC. Lenalidomide DCs also show lower levels of B7 receptors which might be a contributing factor to this phenomenon. Blocking CD28-B7 interaction with CTLA4Ig or CD28(Fab) molecules reduced the pro-survival effect of DC on MM against dexamethasone (Fig 2) melphalan or bortezomib. In order to determine the role of IL-6 in an environment where myeloma cells derive pro-survival signals from their interaction with DC, we used neutralizing antibodies against human IL-6 in cocultures of MM cells with DC. Surprisingly, IL-6 neutralization did not affect the protective effect of DC on MM in cocultures in the presence of chemotherapeutic drugs like melphalan or dexamethasone (Fig 2).
All these suggest that targeting DC might be a viable strategy towards augmenting chemotherapy, either by using agents that attenuate DC differentiation or agents that can block the CD28-B7 interaction between DC and MM. Moreover, MM cells do not seem to depend much on IL-6 as a survival factor when they are in contact with DC and its pro-survival effect is more visible when myeloma cells have to survive outside the microenvironment without DC (previous presentation at ASH 2011).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal