Abstract
Abstract  750
750
Treatment remains a challenge for systemic light chain amyloidosis (AL). Autologous stem cell transplant (AutoSCT) has been associated with long term survival. However, a recent multicenter randomized study failed to show survival benefit for AutoSCT perhaps due to high non-relapse mortality (NRM). Here we present a comparison of AutoSCT to other conventional therapies in AL patients treated at our institution with a 14-year follow up.
A total of 2018 cases were identified upon pathology review from 1998–2012. AL was confirmed in 264 patients; primary amyloidosis (PA) in 147 pts and multiple myeloma with amyloidosis (AM) in 110 patients; solitary amyloidoma in 7 patients. AutoSCT was performed in 126 patients (PA=79 and AM=47).
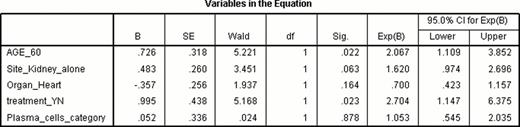
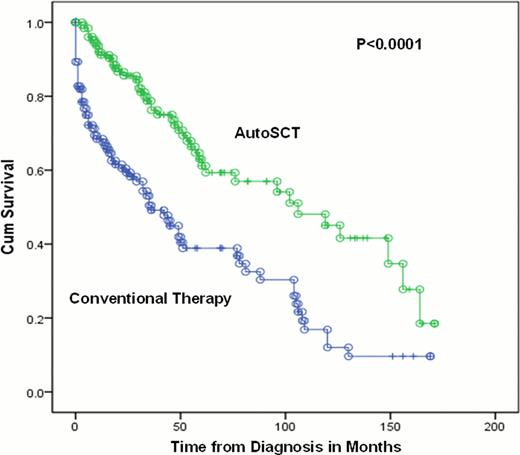
The day 100 NRM was 5% and 1-year NRM was 8%. With a follow up of 14 years in surviving patients, the 10-year overall survival (OS) of AL patients was significantly better in those undergoing AutoSCT (41% vs. 17%; p<0.0001; figure 1). Involvement of more than one organ (6-yr OS 36% vs. 55%; p=0.04) and cardiac involvement (2-yr OS of 57% vs. 78%; p=0.01) were associated with poor outcome. In the patients undergoing AutoSCT: PA vs. AM, Mayo staging, Boston University (BU) staging or bone marrow plasma cells >10 % at the time of autoSCT did not have an impact on OS. Cardiac biomarkers including NT-ProBNP and Troponin-I and T levels were available in a limited number of patients and were not analyzed for survival outcomes. In multivariate analysis, superior OS was associated with: age <60yrs (HR 2.1, p=0.022); and induction treatment before AutoSCT (HR 2.7, p=0.02). Involvement of kidney as the only end organ showed a trend toward improved survival (HR 1.6, p=0.06) (Table 1). Specifically for PA patients (n=79); treatment before autoSCT was associated with improved 3-yr OS: 85% vs. 66%; p=0.02.
AL patients should be evaluated for AutoSCT and selected patients should undergo induction therapy to decrease amyloid burden prior to AutoSCT.
OS: AutoSCt vs. Conventional Therapy in AL Amyloidosis patient
OS: AutoSCt vs. Conventional Therapy in AL Amyloidosis patient
Multivariate Cox Regression Analysis to evaluate factors affecting OS in AL pts undergoing AutoSCT (n=126)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal