Abstract
Significant improvements have been made in the treatment of acute lymphoblastic leukemia (ALL) during the past 2 decades, and measurement of submicroscopic (minimal) levels of residual disease (MRD) is increasingly used to monitor treatment efficacy. For a better comparability of MRD data, there are ongoing efforts to standardize MRD quantification using real-time quantitative PCR of clonal immunoglobulin and T-cell receptor gene rearrangements, real-time quantitative-based detection of fusion gene transcripts or breakpoints, and multiparameter flow cytometric immunophenotyping. Several studies have demonstrated that MRD assessment in childhood and adult ALL significantly correlates with clinical outcome. MRD detection is particularly useful for evaluation of treatment response, but also for early assessment of an impending relapse. Therefore, MRD has gained a prominent position in many ALL treatment studies as a tool for tailoring therapy with growing evidence that MRD supersedes most conventional stratification criteria at least for Ph-negative ALL. Most study protocols on adult ALL follow a 2-step approach with a first classic pretherapeutic and a second MRD-based risk stratification. Here we discuss whether and how MRD is ready to be used as main decisive marker and whether pretherapeutic factors and MRD are really competing or complementary tools to individualize treatment.
Introduction
Treatment outcome in acute lymphoblastic leukemia (ALL) patients depends on a combination of multiple factors, such as properties of the leukemic cells (eg, proliferative capacity, susceptibility to drugs, and other escape mechanisms), host factors (eg, general fitness and concomitant diseases, treatment compliance, host pharmacodynamics and pharmacogenetics), and treatment given to eradicate the disease. Many of intrinsic leukemia cell and host factors have already been elucidated with immunologic and molecular methods and are ongoing translated into providing prognostic information (Table 1). Based on retrospective analyses of large cohorts of patients, conventional pretherapeutic risk criteria, including age, elevated white blood cell count at diagnosis, adverse immunophenotypic features, and cytogenetic as well as molecular aberrations provide the basis for upfront risk stratification in current treatment protocols. It has to be acknowledged, however, that these advances in our understanding of ALL biology in the past have only to a limited extent been accompanied by improved survival of adult ALL patients with relapse still being the main clinical problem. The source of these relapses is the persistence of minimal residual disease (MRD) that is undetectable by standard diagnostic techniques. Several studies have shown that detection of MRD in childhood and adult ALL is an independent risk parameter of high clinical relevance, both in de novo and relapsed ALL as well as in ALL patients undergoing stem cell transplantation (SCT).1-14 Consequently, an increasing number of treatment protocols use MRD as a tool for treatment stratification. In addition, postremission MRD monitoring is also used to predict an impending relapse and to start preemptive salvage treatment in time. Therefore, MRD is not only a prognostic factor but challenges the traditional concept of defining remission and relapse. Prerequisite for application of MRD for treatment tailoring is an adequate, sensitive, and standardized MRD methodology. The focus of this Perspective is therefore to highlight pros and cons of the different MRD techniques, to present the published experience of MRD analysis and MRD-guided treatment in adult ALL, and to discuss the value of MRD in different clinical settings compared with other prognostic factors.
Pretherapeutic factors associated with outcome in adult ALL81-83
| Factor . | Category . | Prognostic impact . | Potential impact on targeted therapy . |
|---|---|---|---|
| Age | — | Worse outcome with advancing age84,85 | — |
| White blood cell count at diagnosis | B: > 30 × 109/L (B) | High WBC associated with poor prognosis84,85 | — |
| T: > 100 × 109/L (T) | |||
| Immunophenotype | CD20 expression | Conflicting data concerning prognosis74,75 | Monoclonal antibodies |
| T versus B | Independent prognostic significance (T-ALL with better prognosis) mainly in early studies84,85 | Monoclonal antibodies Bispecific T-cell engager nelarabine | |
| Cytogenetics | t(9;22)/BCR-ABL | Poor prognosis86,87 | TKI |
| t(4;11)/MLL-AF4 | Poor prognosis86,87 | — | |
| t(8;14) | |||
| Hypodiploidy* | |||
| Near triploidy | |||
| Complex karyotype† | |||
| t(1;19) | Conflicting data concerning prognosis88,89 | — | |
| High hyperdiploidy‡ | Better prognosis86 | — | |
| del(9p) | |||
| Specific molecular alterations | JAK mutations | Emerging significance of poor prognosis90 | JAK inhibitors |
| IKZF Deletions/sequence mutations | Emerging significance of poor prognosis91,92 | ||
| CRLF2 overexpression | Emerging significance (mainly childhood ALL) of poor prognosis92 | CRLF antibodies | |
| ERG/BAALC expression | Conflicting data concerning prognosis93,94 | ||
| NOTCH1 mutations | Conflicting data concerning prognosis95,96 | NOTCH1 targeting |
| Factor . | Category . | Prognostic impact . | Potential impact on targeted therapy . |
|---|---|---|---|
| Age | — | Worse outcome with advancing age84,85 | — |
| White blood cell count at diagnosis | B: > 30 × 109/L (B) | High WBC associated with poor prognosis84,85 | — |
| T: > 100 × 109/L (T) | |||
| Immunophenotype | CD20 expression | Conflicting data concerning prognosis74,75 | Monoclonal antibodies |
| T versus B | Independent prognostic significance (T-ALL with better prognosis) mainly in early studies84,85 | Monoclonal antibodies Bispecific T-cell engager nelarabine | |
| Cytogenetics | t(9;22)/BCR-ABL | Poor prognosis86,87 | TKI |
| t(4;11)/MLL-AF4 | Poor prognosis86,87 | — | |
| t(8;14) | |||
| Hypodiploidy* | |||
| Near triploidy | |||
| Complex karyotype† | |||
| t(1;19) | Conflicting data concerning prognosis88,89 | — | |
| High hyperdiploidy‡ | Better prognosis86 | — | |
| del(9p) | |||
| Specific molecular alterations | JAK mutations | Emerging significance of poor prognosis90 | JAK inhibitors |
| IKZF Deletions/sequence mutations | Emerging significance of poor prognosis91,92 | ||
| CRLF2 overexpression | Emerging significance (mainly childhood ALL) of poor prognosis92 | CRLF antibodies | |
| ERG/BAALC expression | Conflicting data concerning prognosis93,94 | ||
| NOTCH1 mutations | Conflicting data concerning prognosis95,96 | NOTCH1 targeting |
— indicates not applicable; CRLF2, cytokine receptor-like factor 2; ERG, v-ets erythroblastosis virus E26 oncogene homolog (avian); BAALC, brain and acute leukemia, cytoplasmic; IKZF, IKAROS family zinc finger; JAK, Janus kinase; TKI, tyrosine kinase inhibitors; and WBC, white blood cell count.
< 44 chromosomes/leukemic cell.
> 5 abnormalities.
> 50 chromosomes/leukemic cell.
Does methodology of MRD detection matter? Pros and cons of different techniques
MRD assessment relies on the identification of specific molecular or immunophenotypic markers on the leukemia cells. Flow cytometry (FCM) is applied to detect combinations of cell markers that are present on the leukemic but not on normal bone marrow cells. PCR is used to detect leukemia-specific fusion transcripts (eg, BCR-ABL) or clone specific immunoglobulin (Ig) or T-cell receptor (TCR) genes.
Each of these techniques has its own strengths and limitations, which are summarized in Table 2 and are described in more detail within the next 3 sections.
Features of techniques currently employed for MRD detection in ALL
| . | General statements . | Pros . | Cons . |
|---|---|---|---|
| Flow cytometry | Aberrant antigene expression | Applicable for almost all ALL patients | Immunophenotypic shifts of leukemic cells |
| Sensitivity depends on technology (number of colors) and on cell input | Availability of methodology in many laboratories | Expanded and altered precursor-B-cell compartment during regeneration | |
| Rapid | Low cellularity during/after induction | ||
| Quantitative | Relatively high costs (depends on cell input, number of markers/colors and ulterior cytometer use) | ||
| Additional information on benign cells | Limited sensitivity/applicability using 3- to 4-color flow cytometry | ||
| Additional information on malignant cells | ≥ 6-color flow cytometry: extensive knowledge and experience for sensitive and standardized analysis needed | ||
| Identification and monitoring of treatment targets possible | No sample asservation and retrospective analysis possible (on-site availability of expert operators necessary) | ||
| Growing standardization (mainly throughout Europe) | |||
| DNA-based RQ-PCR | Targets mainly Ig and TCR gene rearrangements but also MLL gene rearrangements or SIL-TAL-deletions | Applicable for almost all ALL patients | Time-consuming marker characterization |
| High sensitivity | Potential instability of targets (clonal evolution phenomena, therefore need for preferably 2 targets/patient) | ||
| High degree of standardization | Extensive knowledge and experience needed | ||
| Accepted and uniformly used definition of quantitative range and sensitivity | Relatively expensive | ||
| Well-established stratification tool in various clinical protocols | |||
| Most published data for evidence-based treatment decisions | |||
| Stability of DNA (multicenter setting, shipment time) | |||
| Possibility of sample storage and retrospective/batch analysis | |||
| Quantitative RT-PCR of fusion transcripts | Targets mainly BCR-ABL transcripts (∼ 35% of adult B-cell precursor ALL) | High sensitivity | Useful only in a minority of patients |
| Unequivocal link with leukemic/preleukemic clone | Instability of RNA | ||
| Stability of target during course of treatment | Uncertain quantitation because of unknown number of RNA transcripts/cell (potential differences during course of treatment) | ||
| Fast | False positivity resulting from cross-contamination | ||
| Relatively cheap | Standardization necessary |
| . | General statements . | Pros . | Cons . |
|---|---|---|---|
| Flow cytometry | Aberrant antigene expression | Applicable for almost all ALL patients | Immunophenotypic shifts of leukemic cells |
| Sensitivity depends on technology (number of colors) and on cell input | Availability of methodology in many laboratories | Expanded and altered precursor-B-cell compartment during regeneration | |
| Rapid | Low cellularity during/after induction | ||
| Quantitative | Relatively high costs (depends on cell input, number of markers/colors and ulterior cytometer use) | ||
| Additional information on benign cells | Limited sensitivity/applicability using 3- to 4-color flow cytometry | ||
| Additional information on malignant cells | ≥ 6-color flow cytometry: extensive knowledge and experience for sensitive and standardized analysis needed | ||
| Identification and monitoring of treatment targets possible | No sample asservation and retrospective analysis possible (on-site availability of expert operators necessary) | ||
| Growing standardization (mainly throughout Europe) | |||
| DNA-based RQ-PCR | Targets mainly Ig and TCR gene rearrangements but also MLL gene rearrangements or SIL-TAL-deletions | Applicable for almost all ALL patients | Time-consuming marker characterization |
| High sensitivity | Potential instability of targets (clonal evolution phenomena, therefore need for preferably 2 targets/patient) | ||
| High degree of standardization | Extensive knowledge and experience needed | ||
| Accepted and uniformly used definition of quantitative range and sensitivity | Relatively expensive | ||
| Well-established stratification tool in various clinical protocols | |||
| Most published data for evidence-based treatment decisions | |||
| Stability of DNA (multicenter setting, shipment time) | |||
| Possibility of sample storage and retrospective/batch analysis | |||
| Quantitative RT-PCR of fusion transcripts | Targets mainly BCR-ABL transcripts (∼ 35% of adult B-cell precursor ALL) | High sensitivity | Useful only in a minority of patients |
| Unequivocal link with leukemic/preleukemic clone | Instability of RNA | ||
| Stability of target during course of treatment | Uncertain quantitation because of unknown number of RNA transcripts/cell (potential differences during course of treatment) | ||
| Fast | False positivity resulting from cross-contamination | ||
| Relatively cheap | Standardization necessary |
Multiparameter flow cytometry
MRD measurement by FCM is based on the detection of leukemia-associated immunophenotypes that can be used to distinguish them from normal hematopoietic cells. Leukemia-associated immunophenotypes usually describe a subpopulation of cells of a given lineage at a particular differentiation stage with aberrant molecular expression patterns, asynchrony, and/or profound overexpression or underexpression of molecules.15 Therefore, unlike molecular methods, FCM needs the identification of a cluster of events for definition of MRD positivity. Using 4-color flow cytometry, leukemia-associated immunophenotypes can be identified in ∼ 90% of B-precursor and > 95% of all T-ALL patients reaching detection limits of 10−3-10−4.5,16-22
The major advantage of FCM is its rapidity, which allows reporting of quantitative results within 1 day. This is specifically useful when MRD results are needed quickly to guide therapy. In addition, FCM allows the simultaneous assessment of cell qualities requisite for emerging targeted therapies in ALL.23,24 A potential pitfall of the method results from similarities between leukemic lymphoblasts and nonmalignant lymphoid precursors in various phases of regeneration or chemotherapy-induced alterations that may lead to false positivity.18,25 In addition, phenotypic shifts frequently occur in leukemic cells during induction among others because of steroid-induced gene expression modulation.23-28 In times of targeted therapies (eg, anti-CD19, anti-CD20, anti-CD22, or anti-CD33 treatment), also completely unknown marker shifts may occur potentially influencing detectability of residual leukemic cells. Therefore, interpretation of MRD FCM data requires a deep understanding of the expression patterns of benign hematogones and leukemic cells within different treatment phases and should be restricted to reference laboratories, even if FCM is broadly available in many hematolgoy centers.16
In addition, careful standardization of experimental setup and interpretation is needed to obtain comparable MRD results in multicenter studies, which is one topic of international study groups.29-33 Additional efforts focus on improving the method and its sensitivity through usage of more colors (≥ 8), inclusion of new markers, possibly more specific for leukemic cells, and development of new software for fast and easy automated data analysis.
PCR analysis of Ig and TCR gene rearrangements
Ig and TCR gene rearrangements represent fingerprint-like DNA regions of individual lymphoid cells and its descendants, making them attractive targets for clone specific PCR. Prerequisite is the molecular characterization of leukemia-specific Ig/TCR gene rearrangements for each individual patient, which is possible for the majority (> 95%) of B- and T-lineage ALL. Quantification of these target genes is nowadays performed with quantitative real-time quantitative (RQ)–PCR that allows for a higher degree of automation and sample throughput without the need of post-PCR manipulation of samples.34-37 Similarly to rearranged immune genes, also some leukemia specific translocations (in particular MLL rearrangements) can be used as targets for DNA-based quantitative RQ-PCR analysis after the rearrangement break point at the DNA level has been characterized.38,39 Sensitivity is determined exactly for each assay and generally reaches 1:104-1:105, which is ∼ 0.5-1.0 log higher than for published FCM-based MRD assays.19,21,40
Right from the start, DNA-based MRD diagnostics has been highly standardized through the efforts of the EuroMRD Group. Guidelines are published for determination of linearity, sensitivity, specificity, and reproducibility for each clone-specific assay.36 Usage of DNA as analytical sample allows long shipping times, sample storage, and retrospective cumulative PCR analyses of sample batches. Nevertheless, there are some caveats, including clonal evolution of Ig/TCR genes, which may lead to false negativity. It is therefore recommended to use at least 2 independent targets. On the other hand, false-positive MRD results cannot be completely excluded as massive regeneration of normal lymphoid progenitors might lead to low levels of nonspecific amplification.41,42 In addition, the method needs the time-consuming initial characterization of the leukemic Ig/TCR rearrangements with a panel of different PCR and sequencing reactions. However, recent advances in sequencing technology (next-generation sequencing) will probably accelerate this process in the near future and even add a new molecular technology for MRD assessment.43
PCR analysis of fusion transcripts
Leukemia-specific gene fusions represent ideal targets for MRD detection because they are linked to the oncogenic process and are therefore highly specific. Only few translocations (mainly MLL rearrangements38 and SIL-TAL1 translocations) are analyzed on DNA level, the broadest routine clinical use is the quantification of aberrant BCR-ABL mRNA transcripts in Philadelphia (Ph)–positive ALL.
Advantages of quantitative reverse transcriptase-PCR (RT-PCR) to evaluate fusion transcripts in Ph-positive ALL include the high sensitivity of up to 10−6 because of presence of multiple specific mRNA-transcripts per cell. Furthermore, these transcripts allow the usage of the same primer/probe-combinations for quantitative RT-PCR of many patients, thus keeping the costs for the individual analyses low. In addition, there is a broad experience in BCR-ABL PCR assays because it is widely used for MRD monitoring in CML. However, methodologies are not fully comparable for both entities (dominance of minor break-point transcript in Ph-positive ALL compared with major breakpoint cluster region in CML, differences in relevant MRD thresholds with higher sensitivities being required in Ph-positive ALL).
A crucial point for BCR-ABL PCR is the sample quality, which is adversely influenced by long transport times resulting in degradation of RNA. In addition, lack of standardization of RNA extraction, cDNA synthesis, selection of housekeeping genes, and variation in the way quantitative RT-PCR analyses are carried out lead to substantial differences in results and carry the risk of false negativity. In addition, false positivity cannot be ruled out (eg, because of cross-contamination) and is observed in external quality controls even among experienced laboratories. There are ongoing efforts to standardize methodology and interpretation to allow a better comparability of PCR results within different clinical trials.44
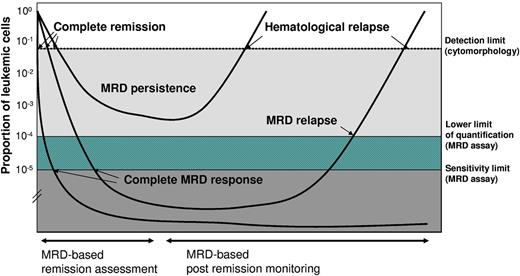
Proposal for a uniform description of MRD results
An important step toward a better comparability of MRD data are the standardized and uniform description of MRD results. Irrespective of the methodology used a testing result may be (1) negative, (2) positive without being quantifiable because of the rarity of the event, and (3) positive at a quantifiable level (Figure 1).
Proposals for definition of MRD terms in ALL. Data from Brüggemann et al16 with permission.
Proposals for definition of MRD terms in ALL. Data from Brüggemann et al16 with permission.
Concerning Ig/TCR-PCR, these results are defined by the EuroMRD Group based on the general performance, linearity, reproducibility, and background of the individual assay.36 In addition, for BCR-ABL and FCM MRD, there are ongoing international efforts to define generally accepted guidelines for standardized analysis and interpretation of results.30,33,44
MRD for assessment of remission and relapse compared with other prognostic factors
The 2 major applications of MRD in adult ALL are (1) the assessment of response to initial therapy for definition of MRD-based risk groups and (2) the subsequent monitoring of remission patients to detect MRD reoccurrence and allow a preemptive salvage treatment.
MRD for initial remission assessment
The most significant application of MRD for de novo ALL is the sensitive assessment of treatment efficacy in patients reaching a complete morphological remission, thereby refining initial risk stratification. Compared with childhood ALL with reports on several thousand patients,2,45 MRD in adult ALL has been studied less extensively. Nevertheless, also in adult ALL large studies have shown that initial MRD kinetics is highly predictive for outcome (Table 3).
Selected MRD studies for assessment of treatment response in adult ALL
| Study . | No. and risk group of patients . | Treatment . | MRD assessment/prognostic significance of MRD/conclusions . | Retaining prognostic significance of classic risk factors/comments . |
|---|---|---|---|---|
| Ph-negative ALL* | ||||
| Vidriales22 (2003) | 102 patients | According to clinical risk factors: | FCM (3 colors) during (d+14) and after (d+35) induction: | MRD most relevant independent prognostic factor |
| B- and T-lineage | Chemo (n = 65) | Prognostic influence of MRD at both time points | Additional independent prognostic factors: age, WBC, Ph positivity | |
| CR after induction | Plus auto-SCT (n = 14) | Poor prognosis in patients with MRD persistence ≥ 5 × 10−3 d+14 and/or ≥ 5 × 10−4 d+35 Excellent prognosis in small subgroup of patients with early MRD clearance (< 3 × 10−4, d+14) | ||
| Plus allo-SCT (n = 23) | ||||
| Brüggemann3 (2006) | 196 patients B- and T-lineage SR ALL | Chemo† | RQ-PCR (Ig/TCR) at 9 time points (d+11, d+24, d+44, d+71, wk+16, wk+22, wk+30, wk+41, wk+52) | Study population homogeneous concerning other prognostic factors MRD only variable with significant impact on outcome No prognostic impact of remaining variables (age, WBC, T- vs B-lineage) |
| Prognostic influence of MRD at all time points Excellent prognosis in small subgroup of patients with early MRD clearance (MRD negativity at d+14) Poor prognosis in patients with MRD persistence (MRD > 1 × 10−4 from d+71 onwards) | ||||
| Holowiecki48 (2008) | 116 patients B- and T-lineage SR (n = 34) and HR (n = 82) ALL | Chemo (n = 54) Auto-SCT (n = 27) Allo-SCT (n = 35) | FCM (3 colors) after induction and Cons Poor prognosis in SR and HR patients with MRD > 10−3 after induction and being treated with Chemo alone Higher proportion of patients with MRD > 10−3 in HR patients than in SR patients No prognostic impact of MRD on T-ALL No significant impact of MRD after Cons | MRD after induction most relevant independent prognostic factor Additional independent prognostic factors: age and WBC |
| Bassan1 (2009) | 112 patients B- and T-lineage All risk groups | According to MRD and clinical risk factors‡ Chemo (n = 51) Allo-SCT (n = 25) Auto-SCT (n = 21) No additional treatment (relapse, toxicity: (n = 15) | RQ-PCR (Ig/TCR and/or fusion genes) at 3 time points (wk+10, wk+16, wk+22) | Combined MRD information at wk+16 and wk+22 most relevant independent prognostic factor |
| Good prognosis in patients with MRD < 10−4 (wk+16) and any MRD negativity (wk+22) irrespective of classic risk group Poor outcome in patients with MRD persistence without differences related to original clinical risk class Early MRD (wk+10) predicted late MRD (wk+16/wk+22) | Additional independent prognostic factor: WBC Allo-SCT not needed in HR patients with MRD LR profile | |||
| Patel47 (2010)§ | 159 patients B-lineage ALL | Irrespective of risk group Chemotherapy (n = 94) Auto-SCT (n = 25) Allo-SCT (n = 40) | DNA fingerprinting/RQ-PCR (Ig/TCR) at 3(-5) time points (wk+5, wk+10, wk+17, for patients without SCT: also wk+28, wk+39): Prognostic influence of MRD in patients receiving Chemo or auto-SCT as postremission treatment Most discriminative time points: wk+10, wk+17 No significant impact of MRD in patients with allo-SCT | No multivariate analysis performed |
| Gökbuget46 (2012) | 580 patients B- and T-lineage ALL SR (n = 434) and HR (n = 146) patients) | According to MRD (only SR ALL) and clinical risk factors: Chemo (n = 425) Allo-SCT (n = 155) | RQ-PCR (Ig/TCR) at 2 time points (d+71, wk+16) Prognostic influence of MRD at d+71 and wk+16 Complete MRD response rate higher in SR vs HR patients (d+71: 77% vs 51%), clinical benefit of complete response comparable for SR and HR patients | Multivariate analysis: MRD only parameter with significant prognostic impact |
| MRD-based allo-SCT in MRD-HR patients | ||||
| SCT performed in half of the patients | ||||
| Improved DFS and OS for patients with SCT | ||||
| Ph-positive ALL | ||||
| Pane10 (2005) | 45 Ph+ patients | Chemo followed by allo-SCT (in case of available donor, n = 20) | RT-PCR (BCR-ABL) at 2 time points (end of induction, end of first Cons) | Age and WBC did not differ between both MRD groups |
| No TKI | Heterogeneous sensitivity to treatment | |||
| Better DFS and OS in good molecular responders ( > 2 log reduction after induction + > 3 log reduction after Cons 1) compared with poor molecular responders | ||||
| Ottmann97 (2007) | 49 Ph+ patients | Randomized induction: Chemo vs TKI | RT- and qualitative nested PCR (BCR-ABL) after end of induction, each Cons/reinduction cycle | Lower WBC at diagnosis in MRD negative patients |
| Elderly patients (54-79 y) | Cons: Chemo + TKI | Heterogeneous sensitivity to treatment | ||
| MRD response in patients with TKI induction compared to Chemo: | ||||
| Better initial MRD response in TKI group | ||||
| No difference in median MRD level after Cons | ||||
| MRD negativity at any time associated with more favorable outcome | ||||
| Yanada53 (2008) | 100 Ph+ patients‖ | Induction Chemo + TKI | RT-PCR (BCR-ABL) at d+28, d+63 (end of induction), | |
| Donor: allo-SCT in CR1 (n = 60) | end of Cons 1 (+later time points) | |||
| No donor: Cons Chemo + TKI (n = 37) | No impact of rapid MRD clearance (MRD negativity at d+28, d+62 or after Cons 1) on relapse-free survival | |||
| Lee51 (2009) | 52 Ph+ patients | Treatment sequence: Induction Chemo 4 wk TKI Cons Chemo 4 wk TKI Allo-SCT in CR1 (n = 48) or non-CR (n = 4) | RT-PCR (BCR-ABL) after induction Chemo, first TKI, after Cons Chemo, after second course TKI No prognostic impact of MRD after induction Chemo before TKI Better DFS and lower relapse rate in patients with ≥ 3 log reduction after first imatinib course | MRD after TKI most significant independent prognostic factor Chronic GVHD only additional variable with an independent prognostic impact |
| Study . | No. and risk group of patients . | Treatment . | MRD assessment/prognostic significance of MRD/conclusions . | Retaining prognostic significance of classic risk factors/comments . |
|---|---|---|---|---|
| Ph-negative ALL* | ||||
| Vidriales22 (2003) | 102 patients | According to clinical risk factors: | FCM (3 colors) during (d+14) and after (d+35) induction: | MRD most relevant independent prognostic factor |
| B- and T-lineage | Chemo (n = 65) | Prognostic influence of MRD at both time points | Additional independent prognostic factors: age, WBC, Ph positivity | |
| CR after induction | Plus auto-SCT (n = 14) | Poor prognosis in patients with MRD persistence ≥ 5 × 10−3 d+14 and/or ≥ 5 × 10−4 d+35 Excellent prognosis in small subgroup of patients with early MRD clearance (< 3 × 10−4, d+14) | ||
| Plus allo-SCT (n = 23) | ||||
| Brüggemann3 (2006) | 196 patients B- and T-lineage SR ALL | Chemo† | RQ-PCR (Ig/TCR) at 9 time points (d+11, d+24, d+44, d+71, wk+16, wk+22, wk+30, wk+41, wk+52) | Study population homogeneous concerning other prognostic factors MRD only variable with significant impact on outcome No prognostic impact of remaining variables (age, WBC, T- vs B-lineage) |
| Prognostic influence of MRD at all time points Excellent prognosis in small subgroup of patients with early MRD clearance (MRD negativity at d+14) Poor prognosis in patients with MRD persistence (MRD > 1 × 10−4 from d+71 onwards) | ||||
| Holowiecki48 (2008) | 116 patients B- and T-lineage SR (n = 34) and HR (n = 82) ALL | Chemo (n = 54) Auto-SCT (n = 27) Allo-SCT (n = 35) | FCM (3 colors) after induction and Cons Poor prognosis in SR and HR patients with MRD > 10−3 after induction and being treated with Chemo alone Higher proportion of patients with MRD > 10−3 in HR patients than in SR patients No prognostic impact of MRD on T-ALL No significant impact of MRD after Cons | MRD after induction most relevant independent prognostic factor Additional independent prognostic factors: age and WBC |
| Bassan1 (2009) | 112 patients B- and T-lineage All risk groups | According to MRD and clinical risk factors‡ Chemo (n = 51) Allo-SCT (n = 25) Auto-SCT (n = 21) No additional treatment (relapse, toxicity: (n = 15) | RQ-PCR (Ig/TCR and/or fusion genes) at 3 time points (wk+10, wk+16, wk+22) | Combined MRD information at wk+16 and wk+22 most relevant independent prognostic factor |
| Good prognosis in patients with MRD < 10−4 (wk+16) and any MRD negativity (wk+22) irrespective of classic risk group Poor outcome in patients with MRD persistence without differences related to original clinical risk class Early MRD (wk+10) predicted late MRD (wk+16/wk+22) | Additional independent prognostic factor: WBC Allo-SCT not needed in HR patients with MRD LR profile | |||
| Patel47 (2010)§ | 159 patients B-lineage ALL | Irrespective of risk group Chemotherapy (n = 94) Auto-SCT (n = 25) Allo-SCT (n = 40) | DNA fingerprinting/RQ-PCR (Ig/TCR) at 3(-5) time points (wk+5, wk+10, wk+17, for patients without SCT: also wk+28, wk+39): Prognostic influence of MRD in patients receiving Chemo or auto-SCT as postremission treatment Most discriminative time points: wk+10, wk+17 No significant impact of MRD in patients with allo-SCT | No multivariate analysis performed |
| Gökbuget46 (2012) | 580 patients B- and T-lineage ALL SR (n = 434) and HR (n = 146) patients) | According to MRD (only SR ALL) and clinical risk factors: Chemo (n = 425) Allo-SCT (n = 155) | RQ-PCR (Ig/TCR) at 2 time points (d+71, wk+16) Prognostic influence of MRD at d+71 and wk+16 Complete MRD response rate higher in SR vs HR patients (d+71: 77% vs 51%), clinical benefit of complete response comparable for SR and HR patients | Multivariate analysis: MRD only parameter with significant prognostic impact |
| MRD-based allo-SCT in MRD-HR patients | ||||
| SCT performed in half of the patients | ||||
| Improved DFS and OS for patients with SCT | ||||
| Ph-positive ALL | ||||
| Pane10 (2005) | 45 Ph+ patients | Chemo followed by allo-SCT (in case of available donor, n = 20) | RT-PCR (BCR-ABL) at 2 time points (end of induction, end of first Cons) | Age and WBC did not differ between both MRD groups |
| No TKI | Heterogeneous sensitivity to treatment | |||
| Better DFS and OS in good molecular responders ( > 2 log reduction after induction + > 3 log reduction after Cons 1) compared with poor molecular responders | ||||
| Ottmann97 (2007) | 49 Ph+ patients | Randomized induction: Chemo vs TKI | RT- and qualitative nested PCR (BCR-ABL) after end of induction, each Cons/reinduction cycle | Lower WBC at diagnosis in MRD negative patients |
| Elderly patients (54-79 y) | Cons: Chemo + TKI | Heterogeneous sensitivity to treatment | ||
| MRD response in patients with TKI induction compared to Chemo: | ||||
| Better initial MRD response in TKI group | ||||
| No difference in median MRD level after Cons | ||||
| MRD negativity at any time associated with more favorable outcome | ||||
| Yanada53 (2008) | 100 Ph+ patients‖ | Induction Chemo + TKI | RT-PCR (BCR-ABL) at d+28, d+63 (end of induction), | |
| Donor: allo-SCT in CR1 (n = 60) | end of Cons 1 (+later time points) | |||
| No donor: Cons Chemo + TKI (n = 37) | No impact of rapid MRD clearance (MRD negativity at d+28, d+62 or after Cons 1) on relapse-free survival | |||
| Lee51 (2009) | 52 Ph+ patients | Treatment sequence: Induction Chemo 4 wk TKI Cons Chemo 4 wk TKI Allo-SCT in CR1 (n = 48) or non-CR (n = 4) | RT-PCR (BCR-ABL) after induction Chemo, first TKI, after Cons Chemo, after second course TKI No prognostic impact of MRD after induction Chemo before TKI Better DFS and lower relapse rate in patients with ≥ 3 log reduction after first imatinib course | MRD after TKI most significant independent prognostic factor Chronic GVHD only additional variable with an independent prognostic impact |
Only MRD studies being published as peer reviewed papers are listed.
Chemo indicates chemotherapy; Cons, consolidation; CR, complete remission; D, day; DFS, disease free survival; FCM, flow cytometry; HR, high risk; Ind, induction; LR, low risk; OS, overall survival; Ph, Philadelphia chromosome; RQ-PCR, real-time quantitative PCR; RT-PCR, reverse transcriptase-PCR; SCT, stem cell transplantation; SR, standard risk; TKI, tyrosine kinase inhibitors; TP(s), time-point(s); Wk, week; and WBC, white blood cell count.
Only study of Bassan et al includes Ph-positive patients.1
Eleven patients with SCT censored at time of SCT.
Clinical risk factors for assignment to allo-SCT independent of MRD: presence of t(9;22) or t(4;11).
Update from an interim report of Mortuza et al.9
Ph-negative ALL.
Several studies reported on the independent prognostic value of MRD in adult Ph-negative ALL performing either Ig/TCR-quantitative RQ-PCR1,3,9,46,47 or FCM12,22,48 (Table 3). Concordantly, different European study groups demonstrated that MRD persistence measured at different time points 1-6 months after initial diagnosis is associated with a poor prognosis.1,3,9,22,46-48 Brüggemann et al3 and Vidriales et al22 additionally identified a small subset of patients with a very rapid tumor clearance (low-level/undetectable MRD after 2 weeks of therapy) and an excellent prognosis. The presently largest MRD study on adult ALL was recently published by Gökbuget et al and analyzed MRD in Ph-negative patients with standard risk (SR, n = 434) and high risk (HR, n = 146) features.46 A complete MRD response after induction 2 and/or consolidation 1 was associated with a comparable clinical benefit irrespective of pretherapeutic risk factors. MRD was the only parameter with significant prognostic impact in multivariate analysis. The biologic differences between SR and HR patients were reflected by the significant different proportion of patients reaching a complete MRD response between SR and HR patients with ∼ 20% point lower rates of MRD negativity in HR patients.
Whether or not rare factors, such as t(4;11), may retain their prognostic significance is hard to state as these patients are diluted within the whole population. Cimino et al analyzed a limited number of adult MLL-AF4–positive patients demonstrating the prognostic impact of MRD also for this rare biologic entity.49
Ph-positive ALL.
In Ph-positive ALL, most published studies focus on detection and quantification of BCR-ABL transcripts. In the pre-tyrosine kinase inhibitors (TKI) era, the level of MRD after induction and/or consolidation treatment turned out to be a powerful indicator of prognosis, although data differed concerning the discriminative value of different time points for MRD assessment10,50 (Table 3). Introduction of TKI substantially changed treatment outcome and MRD kinetics. In a study by Lee et al, MRD assessment after induction chemotherapy did not retain its prognostic significance when followed by imatinib treatment.51 Conversely, a reduction of BCR-ABL transcript levels of at least 3 log after the first 4-week imatinib therapy was identified as the most powerful predictor of a better disease free survival (DFS) and overall survival (OS) rate after SCT (4-year DFS 82.1% vs 41.7%, P = .009; 4-year OS 82.3 vs 48.6, P = .007). These findings indicate that poor response to chemotherapy may be compensated by subsequent administration of imatinib. Leguay et al presented data of the GRAAL AFR03 study that imatinib combined with high-dose chemotherapy improved molecular remission rate before transplantation and led to an improved outcome.52 In contrast, Yanada et al failed to establish an association between an early MRD response to imatinib combined chemotherapy and outcome and concluded that relapse risk may depend on factors unrelated to initial treatment response53 (eg, outgrowth of preexisting subclones with resistance mutations54 ).
Postremission MRD monitoring
A second important application of MRD is postremission monitoring of patients reaching complete MRD response for early detection of an impending relapse.
Ph-negative ALL.
Raff at al55 were the first to demonstrate within the German Multicenter ALL Study Group (GMALL) trials that molecular relapse defined as reconversion to quantifiable molecular MRD positivity was followed by a clinical relapse after a median time of 4.1 month in Ph-negative ALL. Remarkably, low-level, nonquantifiable MRD was not necessarily related to a subsequent relapse confirming this MRD value as a sort of gray area.16 A recent update of the Raff et al study55 by Gökbuget et al46 confirmed the close correlation between conversion to quantifiable MRD positivity and subsequent relapse: in 34 patients with conversion to quantifiable MRD positivity (“MRD relapse,” n = 13 during first year of treatment, n = 21 subsequently), the probability of continuous complete remission (CCR) was 21% ± 9% at 5 years. If patients with MRD-based SCT in first CR were excluded the probability of CCR was only 0% (5% ± 5% at 3 years).
Ph-positive ALL.
In Ph-positive ALL, several studies published already in the 1990s showed a significant relationship between conversion to MRD positivity and subsequent relapse in the pre-TKI era.10,56-59 Yanada et al confirmed these findings also for Ph-positive patients being treated with imatinib-combined chemotherapy.53 In a prospective study on 100 adult patients with Ph-positive ALL, 29 showed an MRD elevation in CR. Of these, 12 of 13 who had not undergone allogeneic (allo) SCT experienced a relapse, whereas only 3 of 16 patients who underwent allo-SCT relapsed. The authors concluded that an increase in MRD is predictive of a subsequent relapse, but such patients can be successfully treated with allo-SCT.
MRD-based treatment intervention
Treatment stratification according to initial MRD response
The objective of measuring MRD response to initial therapy is to adjust treatment with the ultimate goal to improve outcome of MRD-HR patients and to reduce toxicity in MRD-LR patients without worsening their prognosis.
Several clinical trials on adult ALL implemented MRD into their treatment stratification16 : The PETHEMA ALL-AR-03 trial12,60 focuses on HR Ph-negative ALL and passes on SCT in first complete remission in case of standard cytologic response (< 10% blasts in BM on day 14) and MRD < 5 × 10−4 after early consolidation. In contrast, patients with a slow cytologic response and/or MRD > 5 × 10−4 after early consolidation receive allo-SCT further on. Preliminary results indicate that the prognosis of HR patients with adequate response to induction and adequate clearance of MRD is not worsened by avoiding allo-SCT. The combined MRD level after induction and consolidation therapy was the main prognostic factor for CR, DFS, and OS, although a part of MRD-LR patients received a MRD-based de-escalated therapy.
Within the GMALL 07/03 trial, patients with persistent MRD > 10−4 after induction (day 71) and/or first consolidation (week 16) were allocated to the MRD-HR group61 and qualified for allo-SCT. Gökbuget et al recently showed the first results of MRD-based treatment intensification in these patients: 120 of 504 evaluated patients (24%) were allocated to the MRD-HR group (89 SR and 31 HR patients defined by conventional criteria).46 In 47% of these patients, SCT was realized in first CR, with the SCT rate being significantly higher in HR compared with SR patients (71% vs 39%, P < .002). The probability of CCR after 5 years was significantly higher for patients receiving an MRD-directed SCT in first CR compared with those without SCT in first CR (66% ± 7% vs 12% ± 5%, P < .0001). This also translated into a better OS at 5 years (54% ± 8% vs 33% ± 7%, P = .06).
Bassan et al described an MRD-oriented therapy for all t(4;11)−/t(9,22)− ALL patients within the Northern Italy Leukemia Group.1 MRD-positive patients (defined as MRD > 10−4 before induction-consolidation cycle 6 and MRD positivity before cycle 8) were allocated to allogeneic or autologous SCT, whereas MRD-negative patients received standard maintenance regardless of classic risk factors. Four-year DFS was 76% in MRD-LR patients versus only 24% in the MRD-HR group despite of treatment intensification.
The first phase 2 clinical study prospectively analyzing an MRD-based targeted therapy administered blinatumomab monotherapy in patients with MRD failure or MRD reappearance (defined as quantifiable MRD > 1 × 10−4 after end of first consolidation).62 Sixteen of 20 evaluable patients (15 patients with MRD failure, 5 patients with MRD relapse) became MRD negative after 1 cycle of blinatumomab treatment. Twelve of the 16 MRD responders had never achieved MRD negativity before. MRD negativity translated into an ongoing hematologic remission in all 16 MRD-negative patients within a median observation time of 405 days (1-year relapse free survival probability 78%). One patient was censored because of withdrawal of informed consent during second treatment cycle, 8 of these patients consecutively underwent allo-SCT without any treatment related mortality, and 7 patients did not receive any further consolidation treatment, indicating the possibility of an improved outcome with this MRD-guided treatment, even if data can only be compared with historical controls.
Preemptive treatment in case of MRD recurrence
MRD assessment is also used for preemptive treatment intervention in case of MRD recurrence. In the GMALL 07/03 trial, salvage treatment was intended to be started at time of reoccurrence of quantifiable MRD. In a recent publication,46 10 of 34 patients with MRD relapse underwent MRD triggered SCT in ongoing first CR. Three-year probability of CCR was 80% ± 18% compared with only 5% ± 5% in patients without transplantation. Other study groups also perform postremission MRD monitoring for selected patient subgroups, with some of them drawing clinical consequences in case of high-level MRD.16 Besides SCT, also targeted therapies are investigated to improve outcome in patients with an MRD relapse.
In Ph-positive ALL, postremission MRD monitoring is mainly used to tailor treatment after SCT. Wassmann et al investigated the effect of imatinib to decrease the relapse probability in case of reconversion to MRD positivity after SCT.63 BCR-ABL transcripts became undetectable by both quantitative and nested RT-PCR in 15 of 29 (52%) patients. This was associated with a sustained remission, whereas MRD persistence 6-10 weeks after start of imatinib treatment correlated with an almost certain relapse.
Proposal for selection of sampling time points and methodology
Optimal sampling time points and sampling frequency have to be defined according to the individual protocol depending on the treatment protocol and the stratification aim. In de novo Ph-negative ALL, postinduction MRD assessment (after 2-4 months of treatment) is considered to have the most important role for evaluation of initial treatment response and MRD-based risk-stratification. An MRD assessment during induction (after ∼ 2 weeks of treatment) additionally identifies patients with a rapid tumor clearance and a particular good outcome. Concerning postremission monitoring of MRD for early relapse identification, the GMALL proposes 3-monthly intervals for a total of 3 years as the majority of clinical relapses occur within this time64 and reconversion to MRD-positivity precedes a clinical relapse with a median time of 4.1 months between first quantifiable MRD positivity and relapse.
In Ph-positive ALL, the value of MRD for initial remission assessment is more limited in the era of TKI, whereas MRD assessment is frequently used for postremission monitoring. However, compared with Ph-negative ALL, relapse kinetics seem to be more rapid with median time between MRD elevation and relapse of only 2-3 months with53 or without59 application of TKI. Therefore, sampling frequency is recommended to be higher than in Ph-negative ALL.
Comparisons of MRD results obtained by different methodologies show that different techniques cannot be considered fully interchangeable. The main difference between FCM and Ig/TCR-PCR seems to be sensitivity,19,21,40 with both methods quantifying single signals/leukemic cell. In contrast, BCR-ABL-PCR measures multiple transcripts/cell with copy numbers potentially varying during the course of treatment. As there is evidence of multilineage involvement of Ph-positive cells, target cells also may not be fully concordant to other MRD techniques. Therefore, choice of the MRD method in a particular protocol should be guided by the question to be answered, the experience gained in former MRD trials, the available technical expertise, the logistics, and whether or not treatment intervention is planned according to MRD results.
Can pretherapeutic risk assessment be skipped in adult ALL?
The topic of this Perspective is to debate whether MRD superseded other risk factors. To answer this question, it is essential to illuminate the value of MRD within different clinical settings but also to discuss pretherapeutic factors that partly changed their meaning from prognostic to predictive classifiers.
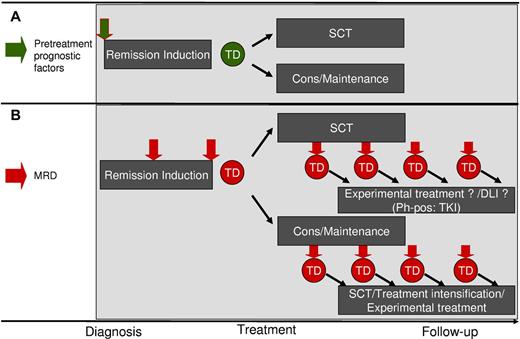
Classic risk factors versus MRD: the conventional concept of risk-oriented therapy
During the past 3 decades, treatment of adult ALL patients composed an induction/consolidation chemotherapy followed either by additional consolidation cycles and maintenance treatment (partly supported by auto SCT) or allo-SCT. Although there was also a discussion on optimization of chemotherapy elements, the main therapeutic decision was whether or not to apply allo-SCT, which on the one hand leads to a reduced relapse rate but on the other hand is accompanied by severe side effects and a considerable treatment-related mortality. Data exist for both treatment paradigms: Collaboration from the United Kingdom Medical Research Council and the Eastern Cooperative Oncology Group demonstrated the superiority of allo-SCT at least in younger patients.65 On the other hand, pediatric-inspired chemotherapy regimens show favorable outcomes in adolescents restraining indication of allo-SCT.66-68 Most protocols struck a balance between both approaches generally recommending SCT for patients with clinical risk factors and a high risk of postchemotherapy relapse. Risk assignment is conventionally based on indirect measures of leukemic burden and chemosensitivity, such as chromosome, molecular, and immunophenotypic analyses at diagnosis (Table 1; Figure 2A). Compared with all these pretherapeutic factors, MRD directly measures chemosensitivity for individual patients and integrates different host-, leukemia-, and treatment-related components of treatment outcome.
Prospective therapeutic shifts according to conventional pretreatment stratification criteria and MRD. (A) Potential treatment decisions based on pretreatment factors. (B) Potential treatment decisions based on MRD. Cons indicates consolidation; DLI, donor lymphocyte infusion; and TD, treatment decision.
Prospective therapeutic shifts according to conventional pretreatment stratification criteria and MRD. (A) Potential treatment decisions based on pretreatment factors. (B) Potential treatment decisions based on MRD. Cons indicates consolidation; DLI, donor lymphocyte infusion; and TD, treatment decision.
Indeed, most published data recognize MRD as most important independent prognostic factor in adult ALL that supersedes all other risk factors, at least for Ph-negative ALL. Prospective studies on MRD-oriented therapy also indicate that MRD-based treatment is safely possible, allo-SCT may be avoided in MRD-LR Ph-negative patients and seems to be particularly active in MRD-HR patients. In addition, MRD measurement helps to prevent the problem of stratifying patients with newly identified genetic risk factors that are too rare to allow a reasonable assignment to a special risk group.
However, available MRD data presented here are not fully consistent. Optimal sampling time points and MRD thresholds seem to differ between ALL subgroups, in particular in Ph-positive compared with Ph-negative ALL. In addition, multivariate analyses in published studies partially retain prognostic factors other than MRD as independent variables (interestingly, the “old-fashioned” factor elevated white blood cell count at diagnosis emerges repeatedly). As an additional restriction, as true also for all other prognostic factors, MRD assessment is not realizable in all patients because of technical limitations (eg, lack of identification of leukemia specific markers, missing follow-up samples). Depending on the minimum technical requirements, the MRD methodology, and the adherence to the protocol, MRD-based stratification using stringent criteria seems to be feasible in ∼ 80%-90% of patients.2,69
It also must be admitted that no published study on adult ALL performed a randomized comparison between action and no action on MRD but only compared the results of MRD-based treatment to historical outcome data or to groups of patients that did not receive an MRD guided therapy for whatever reasons. Therefore, as already started in childhood ALL, also in adult ALL randomized trials have to be done to confirm these encouraging data. MRD excellently qualifies for such an approach because it not only serves as marker for initial treatment stratification but also allows for an ongoing monitoring (Figure 2B). Thereby MRD can serve as “safety net” enabling early reintensification in case of MRD-based treatment de-escalation.
Targeted therapies: prognostic factors become predictive
Increased understanding of molecular mechanisms of cancer and availability of drugs targeting them is changing the meaning of particular leukemic markers from solely prognostic toward predictive factors (Table 1). In adult ALL, BCR-ABL positivity can serve as a model for this transformation: Formerly, the detection of the Ph chromosome during diagnostic workup of adult ALL prognosticated an extremely poor outcome with remission rates being at least 10% lower than in Ph-negative ALL and with a median survival of only 8 months.70 The sole curative option was an allo-SCT. but even in this setting Ph positivity formed the risk group with the poorest outcome, making Ph positivity a “poorly tractable therapeutic problem.”71 However, things changed with the implementation of TKIs as a targeted therapy: CR rates improved and also evidence of a survival benefit emerges. Now BCR-ABL is not only a prognostic marker but also predicts response to TKI. In addition, this new therapeutic approach changes MRD kinetics in Ph-positive ALL. Whereas in the pre-TKI era studies suggested a good correlation between MRD and outcome, MRD data in the TKI setting are more conflicting, and optimal time-points and thresholds are still a matter of debate. A potential reason for the discrepancy between initial MRD response and outcome is the existence of low-level BCR-ABL kinase domain mutations before treatment.54,72,73 Whereas the leukemic bulk may well respond to treatment the small-sized resistant subclone may be the origin of relapse potentially necessitating MRD analysis of subclones in the future.
Even though many of new potential predictive markers are not ready to be used as treatment targets in clinical routine because of issues related to reproducibility, statistical significance, and practical applications, the possibilities of targeted therapy are intriguing. However, when implementing new elements into treatment protocols, the sensitivity of leukemic cells to a particular drug is not known in advance. Traditional risk groups may well respond differently to targeted therapies than they do to classic chemotherapy, potentially leading to unpredictable treatment responses in different subgroups of ALL. For instance, CD20 expression in B-lineage ALL, which is under debate to be an adverse prognostic factor,74,75 is increasingly targeted by protocols including rituximab. Data from the MD Anderson Cancer Center indicate that addition of rituximab to polychemotherapy alters MRD kinetics and significantly improves MRD response.76 However, the effect of the same rituximab dose seems to be different in SR compared with HR patients.77 Therefore, it is particularly important to evaluate treatment success separately within the different subgroups to identify sensitive subpopulations. Ignoring baseline risk factors means obscuring a possibly relevant treatment effect in distinct biologic subsets by diluting in the whole population. Therefore, assessment of pretherapeutic markers cannot be skipped in diagnostic workup of ALL, even if MRD is closely monitored as pretherapeutic and MRD markers increasingly become complementary tools to tailor therapy.
MRD as new primary end point
In times of targeted and sequential therapies, definition of an adequate and discriminatory primary variable for judging treatment success and planning subsequent treatment steps becomes more and more important. OS, the classic gold standard for a primary end point, as reliable, objective, and easily determined parameter gets problematic in times of multimodal and sequential therapies, including SCT. The other endpoint, the CR rate, is less objective in particular in B-cell precursor ALL where the distinction between leukemic cells and hematogones is exceedingly difficult in bone marrow during recovery after chemotherapy or SCT. The value of CR assessment is also limited by the fact that current treatment protocols lead to CR rate of ∼ 90% in adult ALL. In contrast, MRD offers itself as an endpoint in this setting as it is a clinical parameter that integrates different leukemia, host, and treatment aspects into one highly sensitive parameter. As a prerequisite for a usage as primary endpoint, there has to be (1) a plausible biologic relationship between reduction of MRD and response of the disease to therapy, (2) the prognostic value of the surrogate for the clinical outcome has to be validated, and (3) the evidence from clinical trials has to exist that treatment effects on the surrogate correspond to effects on the clinical outcome.78 A necessary technical precondition is the availability of a standardized technology for MRD measurement regarding both standardized analysis and interpretation. This is currently primarily fulfilled for MRD assessment using DNA-based quantitative RQ-PCR analysis according to EuroMRD standards36 and related consensus definitions obtained at the second international symposium on MRD assessment.16 Ten years of international quality controls with > 40 participating laboratories demonstrated the robustness of the system with intra- and inter-assay variability of less than half a log. In addition, FCM-based MRD quantification and quantitative RT-PCR of BCR-ABL transcripts are increasingly standardized within different international collaborations. These analyses have to be performed in accredited specialized laboratories as tests used in decision-making in clinical trials generally have to conform to the Organisation for Economic Co-Operation and Development (OECD) Guidelines on Good Laboratory Practice79 or the Clinical Laboratory Improvement Amendments.80 As shown in large-scale pediatric trials, this does not hamper a broad application to all eligible ALL patients. Although not yet generally accepted as a primary endpoint of clinical trials by the European Medicines Agency and the Food and Drug Administration, MRD measurement in combination with adaptive trial designs may overcome part of the current difficulties in evaluating the efficiency of new agents in ALL.
In conclusion, published data on MRD assessment in adult ALL have shown a strong correlation between MRD response and outcome as well as the prognostic value of MRD reappearance for hematologic relapse. In times of individualized targeted therapies, MRD will not substitute baseline risk factors but evaluate their impact within different treatment regimens and will help to optimize treatment sequence. In this context, MRD has also to be considered as quantitative and objective extension of established endpoints of hematologic remission and relapse more than a substitute of pretherapeutic risk factors.
Acknowledgments
The authors thank Nicola Gökbuget, Dieter Hoelzer, and the participants of the German Multicenter Study Group for adult ALL for their close collaboration in the MRD studies.
This work was supported in part by the Wilhelm Sander Stiftung (2001-074.1 and 2001-074.2) and the Deutsche Krebshilfe (702657Ho2).
Authorship
Contribution: M.B. wrote the first draft of the manuscript; T.R. contributed to the writing and prepared figures; and M.B., T.R., and M.K. finalized the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Monika Brüggemann, Department of Hematology, University Hospital Schleswig-Holstein, Campus Kiel, Chemnitzstrasse 33, D-24116 Kiel, Germany; e-mail: m.brueggemann@med2.uni-kiel.de.