Key Points
CXCR5, but not CXCR4 or CCR7, acts with LFA-1 to mediate random B-cell migration in the T-cell area and B-cell follicles.
In contrast, stromal guidance during B-cell migration is LFA-1 independent and CXCR5 independent.
It is not known how naive B cells compute divergent chemoattractant signals of the T-cell area and B-cell follicles during in vivo migration. Here, we used two-photon microscopy of peripheral lymph nodes (PLNs) to analyze the prototype G-protein–coupled receptors (GPCRs) CXCR4, CXCR5, and CCR7 during B-cell migration, as well as the integrin LFA-1 for stromal guidance. CXCR4 and CCR7 did not influence parenchymal B-cell motility and distribution, despite their role during B-cell arrest in venules. In contrast, CXCR5 played a nonredundant role in B-cell motility in follicles and in the T-cell area. B-cell migration in the T-cell area followed a random guided walk model, arguing against directed migration in vivo. LFA-1, but not α4 integrins, contributed to B-cell motility in PLNs. However, stromal network guidance was LFA-1 independent, uncoupling integrin-dependent migration from stromal attachment. Finally, we observed that despite a 20-fold reduction of chemokine expression in virus-challenged PLNs, CXCR5 remained essential for B-cell screening of antigen-presenting cells. Our data provide an overview of the contribution of prototype GPCRs and integrins during naive B-cell migration and shed light on the local chemokine availability that these cells compute.
Introduction
Chemokine receptors and other G-protein–coupled receptors (GPCRs) guide naive lymphocytes into and within lymphoid tissue. Thus, arrest of bloodborne B cells in high endothelial venules requires binding of the chemokine receptors CXCR4, CCR7, and, to a minor extent, CXCR5 to their respective ligands CXCL12, CCL19/CCL21, and CXCL13, leading to LFA-1 activation and binding to ICAM-1 and ICAM-2.1,-3 Studies in mice have shown that B cells accumulate from their entry point in the T-cell area in 1 of approximately 7-35 B-cell follicles located in the peripheral lymph node (PLN) cortex.4,5 During their migration inside lymphoid tissue, B cells use the ICAM-1–expressing fibroblastic reticular cell (FRC) network of the T-cell area and the follicular dendritic cell (FDC) network in follicles as guidance structures.6,7 Analysis of tissue sections has shown that B-cell accumulation inside follicles is critically dependent on CXCR5 and CXCL13 production by FDCs.8,-10 Naive B cells also express moderate levels of Ebi2 (ie, GPR183), a GPCR binding 7α,25-dihydroxycholesterol (7α,25-OHC) produced by the cholesterol 25-hydroxylase (CH25H) and that mediates accumulation of B cells to the outer rim of B-cell follicles.11,,-14
Despite these insights, there are remarkably few data that describe how chemokine receptors control active B-cell motility within lymphoid tissue. Since naive B cells express chemokine receptors for both the T-cell area and B-cell follicles, an attractive hypothesis is that the balanced responsiveness to CCR7 ligands of the T-cell area and CXCL13 in B-cell follicles shapes dynamic B-cell motility and restrains entry of CXCR5−/− B cells into follicles. Yet, how naive B cells compute the hierarchy and potential redundancy of divergent promigratory factors remains elusive. This is further complicated by technical limitations regarding assessment of the actual availability of chemokines on the stromal network. Thus, it remains unclear whether B cells follow a CXCL13 gradient from their point of arrival in the T-cell area to enter follicles or, alternatively, whether they display a chemokinetic behavior, which is an issue directly linked to the presence or absence of CXCL13 gradients attracting B cells to B-cell follicles. Also, while it is well established that LFA-1 and its ligand ICAM-1 expressed on stromal cell networks contribute to parenchymal B-cell motility,3 it remains unclear whether blocking of these interactions affects the guidance function of FRCs and FDCs during B-cell migration and their microenvironmental distribution. Finally, although homeostatic chemokine levels are strongly suppressed in inflamed PLNs,1,2,15,16 naive B cells retain the capacity to engage with antigen-presenting FDCs through unknown mechanisms.3,17
Here, we used live two-photon (2-P) microscopy and applied a combined genetic and pharmacologic approach to functionally address chemokine availability and evaluate the contribution of CXCR5, CCR7, and CXCR4 during dynamic B-cell motility, including gradient sensing within the T- and B-cell areas. In addition, we investigated the role of integrins during interactions of B cells with the stromal cell network. Our data support a nonredundant role for CXCR5 and LFA-1 in mediating rapid nondirected B-cell migration without affecting guidance by stromal networks. Despite their well-described role for B-cell attachment in HEV, CCR7 and CXCR4 played no role in parenchymal B-cell motility or distribution. The remarkably high in vivo sensitivity of CXCR5 on naive B cells allowed interactions with antigen-presenting FDCs even when CXCL13 levels were strongly depressed, thus ensuring effective participation of naive B cells in ongoing immune reactions.
Methods
Mice
Male and female 8- to 12-week-old CXCR5−/− mice,4,5,8 plt/plt mice,6,7,18 CCR7−/− mice,8,-10,19 and ICAM-1–deficient mice11,,-14,20 on the C57BL/6 background were bred at our animal facility (Bern, Switzerland); Ebi2−/− mice (C57BL/6 strain) and CH25H−/− mice3,21 on the C57BL/6 background were bred at Novartis (Basel, Switzerland). Sex- and age-matched C57BL/6 mice (Harlan, the Netherlands) were used as wild-type lymphocyte donor or recipient mice. For the generation of green fluorescent protein-expressing stromal bone marrow chimeras, C57BL/6-Tg(CAG-EGFP)1Osb/J (CAG-GFP) mice were irradiated with 1000 cGy and reconstituted with at least 10 Mio C57BL/6 bone marrow cells. Reconstitution rates after 8 weeks were >98%. All experiments were performed in accordance with local and federal animal experimentation regulations.
Reagents
CCL21 was from Peprotech (London, UK) and CXCL13 from R&D System (Minneapolis, MN). Fluorescent dyes for cell labeling (CFSE, CellTracker Blue and CellTracker Orange) were purchased from Molecular Probes (Eugene, OR). The CXCR4 antagonist NIBR1816 was synthesized as described.22 Anti–LFA-1 monoclonal antibody (mAb; clone FD441.8) and anti-α4 integrin mAb (clone PS/2) were produced by nanoTools (Freiburg, Germany).
Statistical analysis
The Student t test or analysis of variance was used to determine statistical significance (Prism, GraphPad). Statistical significance was set at P < .05.
All other methods are described in the supplemental data.
Results
CXCR5 controls B-cell follicle entry and migration speed in lymphoid tissue
First, we analyzed the importance of CXCR5 for B-cell homing and egress, as well as for entry from the HEV-containing T-cell area into B-cell follicles. We adoptively transferred fluorescently labeled wild type (WT) and CXCR5−/− B cells into WT hosts and analyzed their distribution inside entire PLNs using selective plane illumination microscopy, which preserves the three-dimensional organ structure (supplemental Figure 1A). CXCR5 was not required for B-cell homing to PLN (Figure 1A), which is in line with abundant CCL21 presentation on HEVs (supplemental Figure 1B-C). Similarly, CXCR5 had only a minor, nonsignificant effect on the dwell time of B cells inside lymphoid tissue, as determined by using Mel-14 to block further homing (Figure 1A). As reported,8 lack of CXCR5 prevented B-cell entry into follicles and retained the B cells close to the HEV vascular network in a distribution similar to that of T cells (Figure 1B-C). Thus, CXCR5 deficiency in B cells did not result in a homogeneous distribution pattern of random positions throughout T-cell areas and B-cell follicles but consistently excluded mutant B cells from follicles where CXCL13 is produced (supplemental Figure 1D).
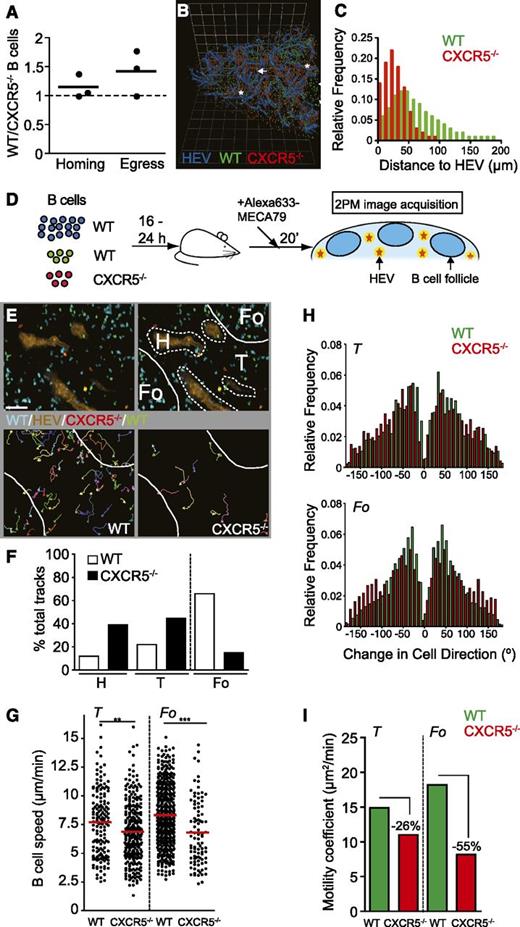
CXCR5 determines localization and migration speed in B-cell follicles and T-cell area. (A) PLN homing and egress of WT and CXCR5−/− B cells. Each dot represents the ratio of WT and CXCR5−/− B cells from pooled PLNs of 1 recipient mouse before and 12 hours after Mel-14 treatment. (B) Three-dimensional reconstruction of a part of the selective plane illumination microscopy–scanned PLN shown in supplemental Figure 1. Asterisks depict accumulation of WT B cells in areas lacking HEV-representing B-cell follicles, arrows highlight the close association of CXCR5−/− B cells with HEV. Grid length, 123 µm. (C) Euclidian distance analysis of WT and CXCR5−/− B cells to the nearest HEV. CXCR5−/− B cells are, on average, closer to HEV located in the T-cell area (31 µm vs 61 µm), similar to adoptively transferred T cells (39 µm; not shown). (D) Schematic outline of the 2-P microscopy experiments with anatomical landmarking. WT B cells (blue) and MECA-79-Alexa633 were used to delineate the B-cell follicle and HEV of the T-cell area, respectively. Low numbers of WT and CXCR5−/− B cells were transferred for cell tracking. (E) Example of 2-P microscopy image (top left panel) and microenvironmental classification (top right panel). Individual WT (bottom left panel) and CXCR5−/− (bottom right panel) B-cell tracks are depicted. Scale bar, 40 µm. (F) Percentage of microenvironmental track distribution as determined by 2-P microscopy. (G) Track speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle. Each dot represents an individual track. The red bar represents the mean. (H) Turning angle distribution of WT and CXCR5−/− B cells in T-cell area and B-cell follicle. (I) Motility coefficients of WT and CXCR5−/− B cells in T-cell area and B-cell follicles. Data in F through I are pooled from 7 mice, 12 image sequences, and 697 WT and 591 CXCR5−/− B-cell tracks. Fo, B-cell follicle; H, HEV; T, T-cell area. **P < .01, ***P < .001.
CXCR5 determines localization and migration speed in B-cell follicles and T-cell area. (A) PLN homing and egress of WT and CXCR5−/− B cells. Each dot represents the ratio of WT and CXCR5−/− B cells from pooled PLNs of 1 recipient mouse before and 12 hours after Mel-14 treatment. (B) Three-dimensional reconstruction of a part of the selective plane illumination microscopy–scanned PLN shown in supplemental Figure 1. Asterisks depict accumulation of WT B cells in areas lacking HEV-representing B-cell follicles, arrows highlight the close association of CXCR5−/− B cells with HEV. Grid length, 123 µm. (C) Euclidian distance analysis of WT and CXCR5−/− B cells to the nearest HEV. CXCR5−/− B cells are, on average, closer to HEV located in the T-cell area (31 µm vs 61 µm), similar to adoptively transferred T cells (39 µm; not shown). (D) Schematic outline of the 2-P microscopy experiments with anatomical landmarking. WT B cells (blue) and MECA-79-Alexa633 were used to delineate the B-cell follicle and HEV of the T-cell area, respectively. Low numbers of WT and CXCR5−/− B cells were transferred for cell tracking. (E) Example of 2-P microscopy image (top left panel) and microenvironmental classification (top right panel). Individual WT (bottom left panel) and CXCR5−/− (bottom right panel) B-cell tracks are depicted. Scale bar, 40 µm. (F) Percentage of microenvironmental track distribution as determined by 2-P microscopy. (G) Track speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle. Each dot represents an individual track. The red bar represents the mean. (H) Turning angle distribution of WT and CXCR5−/− B cells in T-cell area and B-cell follicle. (I) Motility coefficients of WT and CXCR5−/− B cells in T-cell area and B-cell follicles. Data in F through I are pooled from 7 mice, 12 image sequences, and 697 WT and 591 CXCR5−/− B-cell tracks. Fo, B-cell follicle; H, HEV; T, T-cell area. **P < .01, ***P < .001.
Next, we investigated the degree to which a lack of CXCR5 impaired dynamic B-cell motility and, as a consequence, entry into follicles. This was done using 2-P microscopy and anatomical landmarks for HEV (= T-cell area) and B-cell follicles, respectively (Figure 1D and supplemental movie 1). The labeling for HEV allowed us to discard tracks in the perivascular space where migration is lower than in the parenchyma.3,5 While the track distribution analysis confirmed that CXCR5 was required for efficient entry into the follicular microenvironment, CXCR5−/− B cells were observed inside follicles occasionally (Figure 1E-F). There, CXCR5 contributed to B-cell migration speed (8.3 ± 2.6 µm/min for WT B cells vs 6.8 ± 2.8 µm/min for CXCR5−/− B cells; P < .0001) and low turning angles (Figure 1G-H). Accordingly, the motility coefficient was reduced by more than 50%, from 18.2 µm2/min for WT B cells to 8.2 µm2/min for CXCR5−/− B cells (Figure 1I).
WT and CXCR5−/− B cells moving in the T-cell area showed a robust motility and moved only marginally slower than in B-cell follicles. Unexpectedly, we again found WT B cells to move with increased speed and directionality compared with CXCR5−/− B cells (7.7 ± 2.9 µm/min for WT B cells vs 6.9 ± 2.6 µm/min for CXCR5−/− B cells; P < .003; Figure 1G-H), resulting in a 26% decrease in the motility coefficient in the absence of CXCR5 (14.9 µm2/min vs 11.0 µm2/min, respectively; Figure 1I). In summary, CXCR5 contributes not only to B-cell entry into the follicular microenvironment but also to the migration speed and narrow turning angles inside the T-cell area.
Lack of CCR7 and CXCR4 signaling does not alter dynamic B-cell behavior within lymphoid tissue
The robust migration of CXCR5−/− B cells inside the T-cell area pointed to additional factors that drive B-cell motility. B cells express CCR723 and show a strong chemotactic response in vitro to CCL21 (Figure 2A), which promotes LFA-1 activation in HEV.1,5 Similarly, B cells respond to CXCL12 with strong migration, which can be blocked by the CXCR4 antagonist NIBR1816 (Figure 2B).22 We first determined whether CCR7 propels B cells within the T-cell area and retains B cells in this microenvironment, thereby inhibiting random entry of CXCR5−/− B cells into follicles. We used plt/plt mice, which lack expression of CCL19 and CCL21 in the T-cell area of PLNs,7,24 as recipients and followed the dynamic migration of adoptively transferred WT and CXCR5−/− B cells using 2-P microscopy (Figure 1). Despite the lack of CCR7 ligands in the T-cell area, we observed a similar distribution of WT and CXCR5−/− B cell as in WT PLNs (Figure 2C-D). Furthermore, the speed of WT and CXCR5−/− B cells was comparable to speeds observed in WT PLNs, with CXCR5−/− B cells showing a robust but slower migration than WT B cells (T-cell area: WT, 8.4 ± 2.9 µm/min vs CXCR5−/−, 7.3 ± 2.7 µm/min, P < .0001; B-cell follicle: WT, 7.8 ± 2.7 µm/min vs CXCR5−/−, 6.3 ± 2.2 µm/min; P < .01; supplemental movie 2). We confirmed the lack of a detectable influence of CCR7 on B-cell accumulation in follicles or on migration parameters using CCR7−/− B cells in WT PLNs (supplemental Figure 2 and data not shown).
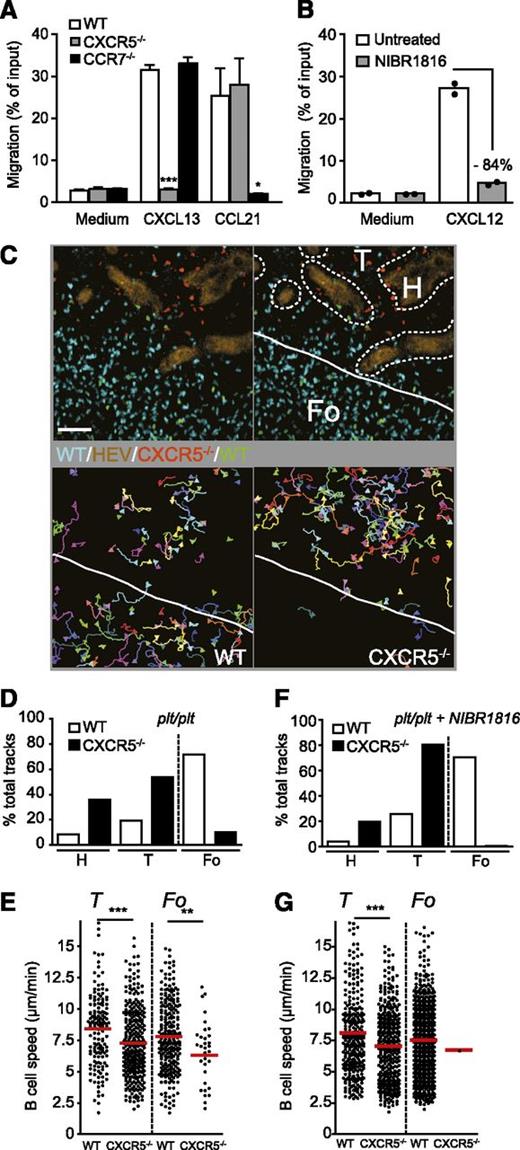
Normal B-cell motility and distribution in the absence of CCR7 and CXCR4 signaling. (A) Chemotaxis of WT, CXCR5−/−, and CCR7−/− B cells toward CXCL13 and CCL21 (100 nM). Data are pooled from duplicates of 2 independent experiments and shown as mean ± standard error of the mean. *P < .05; ***P < .001 (analysis of variance). (B) Chemotaxis of WT B cells to 100 nM CXCL12 in the presence or absence of NIBR1816 (10 µM). Data are from 1 experiment in duplicates. (C) Example of 2-P microscopy image (top left panel) and microenvironmental classification (top right panel) in a plt/plt PLN. Individual WT (bottom left panel) and CXCR5−/− (bottom right panel) B-cell tracks are depicted. Scale bar, 50 µm. (D) Percentage of microenvironmental track distribution in plt/plt PLNs as determined by 2-P microscopy. (E) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicles in plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. (F) Percentage of microenvironmental track distribution in NIBR1816-treated plt/plt PLNs as determined by 2-P microscopy. (G) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicles in NIBR1816-treated plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. Data in D and E are pooled from 3 mice, 10 image sequences, and 558 WT and 263 CXCR5−/− B-cell tracks. Data in F and G are from 3 mice, 5 image sequences, and 1168 WT and 414 CXCR5−/− B-cell tracks. Fo, B-cell follicle; H, HEV; T, T-cell area. **P < .01, ***P < .001.
Normal B-cell motility and distribution in the absence of CCR7 and CXCR4 signaling. (A) Chemotaxis of WT, CXCR5−/−, and CCR7−/− B cells toward CXCL13 and CCL21 (100 nM). Data are pooled from duplicates of 2 independent experiments and shown as mean ± standard error of the mean. *P < .05; ***P < .001 (analysis of variance). (B) Chemotaxis of WT B cells to 100 nM CXCL12 in the presence or absence of NIBR1816 (10 µM). Data are from 1 experiment in duplicates. (C) Example of 2-P microscopy image (top left panel) and microenvironmental classification (top right panel) in a plt/plt PLN. Individual WT (bottom left panel) and CXCR5−/− (bottom right panel) B-cell tracks are depicted. Scale bar, 50 µm. (D) Percentage of microenvironmental track distribution in plt/plt PLNs as determined by 2-P microscopy. (E) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicles in plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. (F) Percentage of microenvironmental track distribution in NIBR1816-treated plt/plt PLNs as determined by 2-P microscopy. (G) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicles in NIBR1816-treated plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. Data in D and E are pooled from 3 mice, 10 image sequences, and 558 WT and 263 CXCR5−/− B-cell tracks. Data in F and G are from 3 mice, 5 image sequences, and 1168 WT and 414 CXCR5−/− B-cell tracks. Fo, B-cell follicle; H, HEV; T, T-cell area. **P < .01, ***P < .001.
Next, we investigated potential redundancy of CXCR5, CCR7, and CXCR4 for B-cell motility by treating plt/plt mice with NIBR1816. Experiments were timed such that high levels of NIBR1816 were present at the time of imaging inside PLNs: the compound levels achieved were 771 ± 42 nM in blood and 33.1 ± 7.2 μg/g tissue in lymph nodes. These are levels at which marked inhibition of CXCR4 is expected.22 Nonetheless, the dynamic migration parameters of WT and CXCR5−/− B cells, as well as their microenvironmental distribution, were not altered through the combined lack of CCR7 and CXCR4 signals. However, we did observe fewer CXCR5−/− B cells in B-cell follicles in this set of experiments (Figure 2F-G). In summary, our 2-P microscopy data do not support a role for CXCR4 or CCR7 ligands during parenchymal B-cell migration or retention in this microenvironment, which suggests a limited availability of these chemokines for migrating B cells. This either points to an inherent capacity of B cells to be motile on stromal support in the absence of such signals or to additional chemokinetic signals for B cells in lymphoid organs.
To address the latter point, we analyzed the role of the recently described GPCR Ebi2 during naive B-cell migration in WT PLNs. As predicted from previous data from histological sections,11,12 2-P microscopy data showed that Ebi2−/− B cells interact efficiently with the CD35+ FDC network, while a higher percentage of WT B-cell tracks were located in the outer rim of B-cell follicles (supplemental Figure 3A-B). Since CH25H is involved in the production of the major Ebi2 ligand 7α,25-OHC, we transferred WT and Ebi2−/− B cells into CH25H−/− hosts expecting to observe a comparable association of both cell populations with the CD35+ FDC network. Instead, WT B cells were found in larger numbers in the outer B-cell follicle rim as compared with Ebi2−/− B cells (supplemental Figure 3C-D), which migrated faster in B-cell follicles as compared with WT B cells (8.3 ± 2.7 µm/min for WT B cells vs 9.4 ± 4.0 µm/min for Ebi2−/− B cells; P < .0001). Our data suggest therefore that under steady-state conditions, Ebi2 controls dynamic naive B-cell distribution to the outer B-cell follicle rim without acting as a promigratory factor. Our data also suggest that in the absence of an inflammatory signal, there is a second source of 7α,25-OHC independent of CH25H (supplemental Figure 3E).
Nondirectional B-cell migration within the T-cell area results in delayed entry into follicles
The faster migration of WT B cells into the T-cell area as compared with CXCR5−/− B cells (Figures 1G, 2E, and 2G) pointed to the presence of functional CXCL13 inside the T-cell area. We therefore determined whether after entering the T-cell area through HEV, B cells migrated in a directed manner toward adjacent follicles, that is, areas that express high levels of CXCL13. In the individual 2-P microscopy recordings, the number of analyzable B-cell tracks inside the T-cell area was too low for a meaningful statistical evaluation of directionality, while the relative position of B-cell follicles and T-cell area varied between recordings. Consequently, we developed a method to normalize B-cell tracks from different image sequences. For each B-cell track in the T-cell area, we determined the closest (x,y) coordinates of adjacent B-cell follicles relative to the starting position of the track (Figure 3A). Normalizing these (x,y) coordinates to the 12 o’clock position allowed alignment of tracks from numerous movies for detection of subtle chemotactic effects. However, within the limits of the observation period and tissue volume, we did not detect evidence of directional B-cell migration from the T-cell area toward adjacent B-cell follicles (Figure 3B and supplemental Figure 4). The percentage of B cells migrating within a 120° angle from their track origin toward the closest follicle intersection was 23.5% for WT B cells and 25.5% for CXCR5−/− B cells as negative control. These data suggest that a long-range CXCL13 gradient in the T-cell area is not detectable.
Absence of a long- or short-range CXCL13-mediated directional B-cell migration into B-cell follicles. (A) Schematic outline of the normalization protocol to pool tracks from various 2-P microscopy image sequences. (B) Normalized tracks of WT (left panel) and CXCR5−/− (right panel) B cells migrating in the T-cell area. A total of 162 WT and 106 CXCR5−/− B-cell tracks are pooled and presented such that the closest intersection point with the nearest B-cell follicle at the onset of cell tracking is at the 12 o’clock position. The percentage of tracks falling into a 120° angle toward B-cell follicles (dashed lines) is indicated. (C) Example of 2-P microscopy image at indicated times post B-cell transfer. Lines define B-cell follicles. The dotted squares are shown enlarged in D and E. Scale bar, 50 µm. (D) A 2-P microscopy image of B cells migrating parallel to and away from an adjacent B-cell follicle taken from the dotted outline from the left panel in C. The top panel shows the starting point of the B cells at the onset of the recording, adjacent to a B-cell follicle. Time in minutes and seconds. (E) A 2-P microscopy image of a B-cell track migrating into an adjacent B-cell follicle taken from the dotted outline from the middle panel in C. (F) Frequency of WT B-cell tracks either entering or moving parallel to/away from adjacent B-cell follicles. All tracks (n = 23) were recorded within the first 150 minutes after B-cell transfer between 20-µm and 130-µm depth. Fo, B-cell follicle.
Absence of a long- or short-range CXCL13-mediated directional B-cell migration into B-cell follicles. (A) Schematic outline of the normalization protocol to pool tracks from various 2-P microscopy image sequences. (B) Normalized tracks of WT (left panel) and CXCR5−/− (right panel) B cells migrating in the T-cell area. A total of 162 WT and 106 CXCR5−/− B-cell tracks are pooled and presented such that the closest intersection point with the nearest B-cell follicle at the onset of cell tracking is at the 12 o’clock position. The percentage of tracks falling into a 120° angle toward B-cell follicles (dashed lines) is indicated. (C) Example of 2-P microscopy image at indicated times post B-cell transfer. Lines define B-cell follicles. The dotted squares are shown enlarged in D and E. Scale bar, 50 µm. (D) A 2-P microscopy image of B cells migrating parallel to and away from an adjacent B-cell follicle taken from the dotted outline from the left panel in C. The top panel shows the starting point of the B cells at the onset of the recording, adjacent to a B-cell follicle. Time in minutes and seconds. (E) A 2-P microscopy image of a B-cell track migrating into an adjacent B-cell follicle taken from the dotted outline from the middle panel in C. (F) Frequency of WT B-cell tracks either entering or moving parallel to/away from adjacent B-cell follicles. All tracks (n = 23) were recorded within the first 150 minutes after B-cell transfer between 20-µm and 130-µm depth. Fo, B-cell follicle.
Next, we determined whether recent B-cell immigrants to PLNs located in close proximity to B-cell follicles experienced a short-range chemotactic CXCL13 gradient for efficient follicle entry. GFP-expressing B cells were transferred into mice that had received both WT B cells and anti-CD35 mAb to outline entire B-cell follicles and the inner FDC network, respectively. B cells accumulated over a period of 2 to 3 hours post transfer in B-cell follicles (Figure 3C). When we analyzed B-cell behavior in close proximity to B-cell follicles, we found that a majority of B cells turned back to the T-cell area, instead of readily entering B-cell follicles (Figure 3D and supplemental movies 3 and 4). On average, only 1 of 4 B cells in close proximity to follicles was observed to directly enter from the T-cell area (Figure 3F), suggesting additional molecular or anatomical constraints for cell entry into follicles. Taken together, although B cells eventually accumulate in follicles, we were unable to detect preferential migration toward follicles.
LFA-1 and CXCR5 cooperate during B-cell motility without affecting guidance by the lymphoid stromal network
In addition to chemokine receptors, integrins are involved in dynamic B-cell migration within lymphoid tissue.3 Consequently, we investigated the role of the B-cell–expressed adhesion molecules LFA-1 and α4 integrins during B cell–stromal network interactions in vivo. As reported,3 LFA-1 blocking resulted in decreased WT B-cell speed within B-cell follicles, from 8.3 ± 2.6 µm/min (Figure 1G) to 6.0 ± 2.6 µm/min (Figure 4A). Similarly, B-cell speed within the T-cell area was decreased from 7.7 ± 2.9 µm/min to 5.8 ± 2.4 µm/min for WT B cells and from 6.9 ± 2.6 µm/min to 5.2 ± 2.0 µm/min for CXCR5−/− B cells after LFA-1 blockade (Figure 4A). Although this decrease seems modest, breathing and tissue deformability artifacts make the in vivo measurements of lymphocyte speeds below 5 µm/min difficult.25,26 A more robust readout is the motility coefficient, which dropped to 3.3 µm2/min for CXCR5−/− B cells in the T-cell area after LFA-1 blocking. Additional blocking of α4 integrins in combination with CXCR4 antagonist treatment in plt/plt mice did not result in a further decrease of B-cell migration speeds (Figure 4B), supporting a nonredundant role for LFA-1 and CXCR5 in controlling naive B-cell migration. In contrast, we did not observe an effect of the functional absence of LFA-1 or its main ligand ICAM-1 on WT, CCR7−/−, and CXCR5−/− B-cell distribution, arguing against a role for integrins and T-cell zone chemokines during B-cell follicle compartmentalization (supplemental Figure 5).
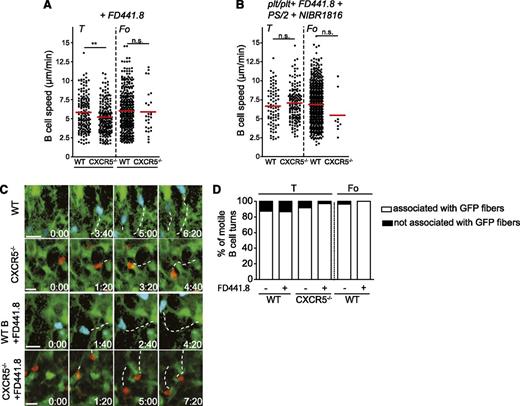
CXCR5 and functional LFA-1 control B cell speed but are dispensable for B-cell guidance by the stromal network. (A) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle of FD441.8-treated PLNs. Each dot represents an individual track. The red bar represents the mean. Data in A are from 3 mice, 3 image sequences, and 534 WT and 227 CXCR5−/− B-cell tracks. (B) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle of FD441.8-, PS/2-, and NIBR1816-treated plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. Data in B are from 2 mice, 5 image sequences, and 773 WT and 155 CXCR5−/− B cell tracks. (C) Example of 2-P microscopy images at indicated times post B-cell transfer. WT and CXCR5−/− B cells with or without FD441.8 treatment migrate in close association with GFP fibers of the T-cell area. The tracks are represented by the dotted line in each frame. Scale bar, 10 µm. (D) Percentage of motile B cell turn of WT and CXCR5−/− B cells in T-cell area and WT B cell in B-cell follicle with and without FD441.8 treatment. Data are pooled from 29 to 63 individual cell tracks. **P < .01. n.s., not significant.
CXCR5 and functional LFA-1 control B cell speed but are dispensable for B-cell guidance by the stromal network. (A) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle of FD441.8-treated PLNs. Each dot represents an individual track. The red bar represents the mean. Data in A are from 3 mice, 3 image sequences, and 534 WT and 227 CXCR5−/− B-cell tracks. (B) Speeds of WT and CXCR5−/− B cells in T-cell area and B-cell follicle of FD441.8-, PS/2-, and NIBR1816-treated plt/plt PLNs. Each dot represents an individual track. The red bar represents the mean. Data in B are from 2 mice, 5 image sequences, and 773 WT and 155 CXCR5−/− B cell tracks. (C) Example of 2-P microscopy images at indicated times post B-cell transfer. WT and CXCR5−/− B cells with or without FD441.8 treatment migrate in close association with GFP fibers of the T-cell area. The tracks are represented by the dotted line in each frame. Scale bar, 10 µm. (D) Percentage of motile B cell turn of WT and CXCR5−/− B cells in T-cell area and WT B cell in B-cell follicle with and without FD441.8 treatment. Data are pooled from 29 to 63 individual cell tracks. **P < .01. n.s., not significant.
Since stromal cells express high levels of ICAM-1,6 the decreased migration speed observed in the absence of functional LFA-1 may be due to defective adhesion of B cells to the underlying stromal network. We tested this hypothesis using bone marrow chimeras expressing GFP in the stromal compartment as recipients for fluorescently labeled WT and CXCR5−/− B cells, followed by 2-P microscopy analysis as described.7 We found that adoptively transferred WT and CXCR5−/− B cells remained attached during their migration to the stromal network and that the vast majority of turns was in association with GFP+ fibers (Figure 4C-D; supplemental movies 5 and 6). Yet, B-cell guidance by the stromal network was unaffected by LFA-1 blockade, both for WT and CXCR5−/− B cells in the T-cell area and for WT B cells migrating along the FDC network (Figure 4C-D; supplemental movies 7 and 8). In summary, LFA-1–ICAM-1 interactions cooperate with CXCR5 signaling to warrant efficient B-cell motility but are not required for guidance by the lymphoid stromal network.
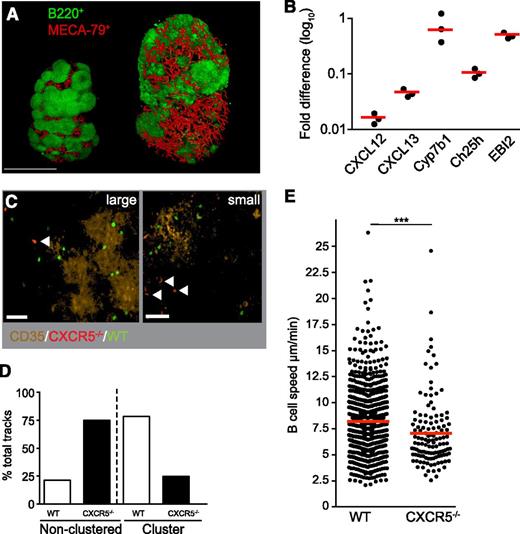
CXCR5-dependent naive B-cell accumulation in dispersed B-cell clusters during viral infection
Our data support a model in which CXCR5 is the predominant GPCR accelerating B cells under homeostatic conditions, while Ebi2 directs B-cell localization to the outer rim and CCR7 and CXCR4 are irrelevant for parenchymal B cell motility or compartmentalization. Infection of mice with lymphocytic choriomeningitis virus (LCMV) results in a strong disruption of the normal lymphoid architecture, with a concomitant decrease in the expression of homeostatic chemokines including CXCL13.15,16 Using optical projection tomography4 and quantitative polymerase chain reaction analysis, we confirmed the LCMV-induced severe disruption of B-cell follicles into small or large, unevenly shaped B-cell clusters. This was accompanied by strongly decreased expression levels of CXCL12, CXCL13, and CH25H but not Ebi2 and Cyp7b1, an enzyme involved in production of oxysterols (Figure 5A-B). We then investigated how this altered chemokine landscape affects motility parameters and FDC interactions of nonactivated B cells. Using 2-P microscopy at day 11 post infection, we observed a preferential WT B-cell migration on small and large B-cell clusters, as identified by CD35+ FDCs, which likely represent the light zones of ongoing germinal center reactions (Figure 5C). In contrast, CXCR5−/− B cells were, for the most part, excluded from B-cell clusters and rarely interacted with FDC despite a 95% reduction of CXCL13 mRNA levels (Figure 5C-D). The ability of naive B cells to screen FDC for cognate antigen and to engage in ongoing immune reactions therefore depends on CXCL13 sensing over a wide range of expression levels. Similar to noninflamed PLN, the rare CXCR5−/− B cells in B-cell clusters migrated more slowly than WT B cells (Figure 5E). Taken together, our data uncover an unexpectedly high CXCR5-dependent sensitivity to enable B-cell accumulation in B-cell clusters in severely disrupted PLNs, thus ensuring continuous scanning of antigen-presenting FDCs by naive B cells.
Residual CXCL13 expression suffices for naive B cell screening of FDCs in virus-challenged PLNs. (A) Example of optical projection tomography images of WT (control, left) and -infected (right) PLN on day 8 post infection. The MECA-79+ HEV network is in red, and B220+ B follicles are green. Scale bar, 1 mm. (B) CXCL12, CXCL13, Cyb7b1, CH25H, and Ebi2 mRNA levels determined by quantitative polymerase chain reaction on day 8 post infection. Each dot represents an individual PLN. The red bar represents the mean. Levels of CXCL12, CXCL13, and CH25H mRNA are significantly reduced as compared with day 0 (P < .0001), as well as with mRNA levels of Ebi2 (P < .001) and Cyp7b1 (P < .01). (C) Example of 2-P microscopy image of LCMV-infected PLN. Arrowheads depict CXCR5−/− B cells located at the edge or outside large and small B-cell clusters identified by CD35+ FDCs. Scale bar, 30 µm. (D) Percentage of microenvironmental track distribution as determined by 2-P microscopy. (E) Speeds of WT and CXCR5−/− B cells inside CD35+ clusters. Each dot represents an individual track. The red bar represents the mean. Data in D and E are pooled from 4 mice, 7 image sequences, and 1049 WT and 176 CXCR5 −/− B-cell tracks. ***P < .001.
Residual CXCL13 expression suffices for naive B cell screening of FDCs in virus-challenged PLNs. (A) Example of optical projection tomography images of WT (control, left) and -infected (right) PLN on day 8 post infection. The MECA-79+ HEV network is in red, and B220+ B follicles are green. Scale bar, 1 mm. (B) CXCL12, CXCL13, Cyb7b1, CH25H, and Ebi2 mRNA levels determined by quantitative polymerase chain reaction on day 8 post infection. Each dot represents an individual PLN. The red bar represents the mean. Levels of CXCL12, CXCL13, and CH25H mRNA are significantly reduced as compared with day 0 (P < .0001), as well as with mRNA levels of Ebi2 (P < .001) and Cyp7b1 (P < .01). (C) Example of 2-P microscopy image of LCMV-infected PLN. Arrowheads depict CXCR5−/− B cells located at the edge or outside large and small B-cell clusters identified by CD35+ FDCs. Scale bar, 30 µm. (D) Percentage of microenvironmental track distribution as determined by 2-P microscopy. (E) Speeds of WT and CXCR5−/− B cells inside CD35+ clusters. Each dot represents an individual track. The red bar represents the mean. Data in D and E are pooled from 4 mice, 7 image sequences, and 1049 WT and 176 CXCR5 −/− B-cell tracks. ***P < .001.
Discussion
B cells express GPCRs for chemokines presented on the HEV lumen, the T-cell area, and B-cell follicles and are able to efficiently induce directed migration in controlled in vitro experiments. It is not known how motile B cells compute various overlapping, divergent chemokine sources in vivo because chemokine availability and gradients are intrinsically difficult to detect. We used naive WT and mutant B cells as surrogate “biosensors” to deduce from their dynamic migratory behavior the shape and availability of chemoattractant gradients in lymphoid tissue. Using 2-P microscopy imaging and a combined pharmacological and genetic inhibition approach, our image analysis data dissect the contributions of the prototypical chemokine receptors CXCR4, CXCR5, and CCR7 for B-cell migration inside lymphoid tissue to uncover the factors that migrating B cells are able to compute during immunosurveillance. Our data provide a “chemokine” landscape, as seen by naive B cells, and uncover an integrin-independent guidance function for FRC and FDC stromal networks (supplemental Figure 6).
CXCR4 and CCR7 ligands are highly expressed in lymphoid tissue, and B-cell adhesion in HEV is efficiently mediated by CCL21 and CXCL12.1 In contrast, our 2-P microscopy analysis showed that CCR7 and CXCR4 signaling did not alter motility parameters or distribution of B cells after transmigration into PLN parenchyma, whereas CCR7 increased T-cell migration by approximately 30%.25,27,-29 The compartmentalized response of naive B cells to HEV- presented, but not FRC-presented, CCL21 is likely due to increased CCL21 deposition on the vasculature as compared with parenchyma. Since nonactivated B cells express lower CCR7 levels than do T cells, our data suggest that outside HEV, B cells are unable to detect the physiologically available levels of T-cell area-expressed chemokines. As chemokines are in part synthesized by lymphoid stromal cells including FRCs, CCL21 detected in tissue sections could be preferentially localized inside FRC conduits for transport to the HEV network, where it may contribute to lymphocyte recruitment.30,,,-34 Thus, 2-P microscopy imaging helps to uncouple in vitro chemoattractant responsiveness from in vivo chemoattractant responsiveness, which depends on the “usable” chemokine levels available to trafficking lymphocytes. At the same time, these data highlight the importance of chemokine receptor levels in responding to presumably limited amounts of stromal chemokine.
In contrast to CXCR4 and CCR7, CXCR5 increased the migration speed of WT B cells localized in the T-cell area as well as in B-cell follicles. Although it is intuitive to assume that B cells would follow a chemotactic gradient from their site of entry in the T-cell zone toward adjacent B-cell follicles, as recently observed during dendritic cell migration to lymphatic vessels,35,36 we did not find evidence for directed motility inside lymphoid tissue. While we cannot exclude a subtle follicle-directed B-cell taxis that is undetectable due to the confined observation volume and duration,37 B cells in close proximity to follicles typically turned back into the T-cell area. This is similar to observations made by Park and colleagues.5 This may be due to one or several of the following scenarios: subsets of stromal cells in the T-cell area express CXCL13,38 which may present low levels of CXCL13 in the T-cell area, thereby disrupting a chemotactic gradient. However, in immunofluorescent sections, virtually all detectable CXCL13 is found in B-cell follicles. As a second option, secreted CXCL13 may diffuse from follicles into the adjacent T-cell area in a process reminiscent of cytokine permeation throughout reactive PLNs.39 Since T cells in the adjacent T-cell area are highly motile and ignore the released CXCL13, a gradient may be unstable due to constant stirring of the extracellular fluid and could explain the chemokinetic effect observed here. A third possibility may be linked to the underlying stromal network anatomy, in particular, the cortical ridge that consists of dense ERTR7-positive reticular fibers surrounding B-cell follicles.40 In this scenario, B cells migrating close to follicles lack appropriate guidance structures to lead them into the B-cell area. Furthermore, the tightly packed environment of B-cell follicles may constitute a physical obstacle for randomly migrating lymphocytes. Thus, successful entry into follicles would require stochastic encounters with stromal elements leading to the FDC network as well as CXCL13 signaling to provide the attractive energy that allows entry into the dense B-cell population. Future studies are required to clarify the mechanisms underlying the remarkable separation of T cells and B cells and explain why cells lacking CXCR5 expression do not randomly enter B-cell follicles, even in the absence of presumed T-cell area retention signals. Additional molecules, presumably ligands for GPCRs due to the dependence of B-cell migration on Gαi2,41 or novel adhesion molecules likely contribute to B-cell migration in lymphoid tissue and retention of CXCR5−/− B cells in the T-cell area. From our in vivo analysis, we can exclude CCR7, CXCR4, ICAM-1, LFA-1, and α4 integrins from participating in B-cell retention in the T-cell area. A potential candidate is B-cell–expressed CLEC-2, which binds podoplanin expressed on FRC.42 Future studies are required to address these issues.
The startling high sensitivity of naive B cells to low levels of CXCL13 in the T-cell area is reflected under inflammatory conditions. Using a virus infection model, our data showed that CXCR5 was required to enable naive B-cell screening of antigen-loaded FDCs, despite strongly suppressed CXCL13 expression. A possible explanation for these observations is the decisive influence of chemokine receptor levels on chemokine detection in vivo, that is, only cells above a high chemokine receptor expression threshold are able to successfully sense or compete with other leukocytes for chemokines with low availability. In any event, the ability of naive B cells to respond to CXCL13 over a wide range of expression levels defines CXCR5 as a key player in the engagement of naive B cells in ongoing germinal centers, where they can compete with previously activated B cells for antigen deposited on FDCs.17
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank U.H. von Andrian and Sarah Henrickson for MatLab scripts; Bettina Stolp, Aleksandra Ozga, and Matthias Baumann for help with experiments; Britta Engelhardt for continuous support; and the Novartis colleagues Agnes Feige, Noemie Beluch, Inga Preuss, Thomas Suply, Isabelle Christen, and Juan Zhang for preparation and mass spectrometry analysis of tissue samples and Christian Beerli for analysis of Novartis Institutes for Biomedical Research levels.
This project was supported by grants from Sinergia to B.L., J.S., and J.V.S. (CRSII3-125447 and -141918), Swiss National Foundation to J.V.S. (31003A_135649), and the VIBRANT project to J.S. (228933/FP7-NMP).
Authorship
Contribution: F.M.C., D.N., S.F.S., M.H., J.S., J.M., R.D., E.S., M.P., H.-G.Z., and J.V.S. performed experiments and analyzed the data; E.S., T.J., and A.W.S. provided vital material; M.T.F. performed the single cell tracking analysis; B.L., J.S., and J.V.S. supervised the work; and F.C.M., D.N., S.F.S., and J.V.S. wrote the manuscript with feedback from all authors.
Conflict-of-interest disclosure: H.-G.Z., A.W.S., and T.J. are employees of Novartis Pharma AG. The remaining authors declare no competing financial interests.
Correspondence: Jens V. Stein, Theodor Kocher Institute, University of Bern, Freiestr. 1, 3012 Bern, Switzerland; e-mail: jstein@tki.unibe.ch.
References
Author notes
F.M.C., D.N., and S.F.S. contributed equally to this work.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal