Key Points
In β-thalassemia major, hepcidin levels are simultaneously associated with erythropoiesis and iron loading pre- and posttransfusion.
Transfusion improves anemia, suppressing erythropoiesis and in turn increasing hepcidin in patients with β-thalassemia major.
Abstract
β-thalassemia major causes ineffective erythropoiesis and chronic anemia and is associated with iron overload due to both transfused iron and increased iron absorption, the latter mediated by suppression of the iron-regulatory hormone hepcidin. We sought to determine whether, in β-thalassemia major, transfusion-mediated inhibition of erythropoiesis dynamically affects hepcidin. We recruited 31 chronically transfused patients with β-thalassemia major and collected samples immediately before and 4 to 8 days after transfusion. Pretransfusion hepcidin was positively correlated with hemoglobin and ferritin and inversely with erythropoiesis. The hepcidin-ferritin ratio indicated hepcidin was relatively suppressed given the degree of iron loading. Posttransfusion, hemoglobin and hepcidin increased, and erythropoietin and growth differentiation factor-15 decreased. By multiple regression, pre- and posttransfusion hepcidin concentrations were both associated positively with hemoglobin, inversely with erythropoiesis, and positively with ferritin. Although men and women had similar pretransfusion hemoglobin, men had significantly increased erythropoiesis and lower hepcidin, received a lower transfusion volume per liter blood volume, and experienced a smaller posttransfusion reduction in erythropoiesis and hepcidin rise. Age of blood was not associated with posttransfusion hemoglobin or ferritin change. Hepcidin levels in patients with β-thalassemia major dynamically reflect competing influences from erythropoiesis, anemia, and iron overload. Measurement of these indices could assist clinical monitoring.
Introduction
The mainstay of therapy for β-thalassemia major is lifelong red cell transfusion to improve anemia and suppress ineffective expanded erythropoiesis.1 Ineffective erythropoiesis causes iron overload due to suppression of the liver-derived hormone hepcidin that regulates iron absorption and recycling via its effects on ferroportin, the cellular iron export protein.2 Low hepcidin preserves ferroportin and permits increased intestinal iron absorption and enhanced macrophage iron release (and hence iron recycling), whereas elevated hepcidin causes degradation of ferroportin, thus decreasing iron absorption and recycling.3 Hepcidin is suppressed by hypoxia4 and iron deficiency5 and is elevated by iron loading and inflammation.6 Erythropoiesis is perhaps the most potent suppressor of hepcidin,7 although the mechanism remains uncertain. The existence of a secreted factor from the erythroid marrow that suppresses hepcidin synthesis has been hypothesized.7 One candidate, growth differentiation factor-15 (GDF-15), is elevated in ineffective erythropoiesis (especially in thalassemia) and suppresses hepcidin expression in vitro.8
Ineffective erythropoiesis in thalassemia is suppressed by transfusion.9 Cross-sectional studies suggest that transfused patients with β-thalassemia major have higher hepcidin than non–transfusion-dependent patients with β-thalassemia intermedia.10,11 Transfusion increases urinary hepcidin in patients with β-thalassemia major.12 If erythropoiesis measurably fluctuates over the intertransfusion interval, thalassemia could be a valuable model to study the dynamic regulation of hepcidin in the face of competing influences of coexistent anemia, expanded erythropoiesis, and iron loading. Although hemoglobin (Hb) concentrations in nonthalassemic men are generally higher than those for women,13 current transfusion dosing guidelines do not account for these potential differences.
In a cohort of chronically transfused patients with β-thalassemia major, we hypothesized that (1) pre- and posttransfusion hepcidin concentrations are simultaneously influenced by anemia and erythropoiesis, iron loading, and inflammation; (2) transfusion-mediated increases in Hb suppress erythropoietic drive, which in turn desuppresses (raises) hepcidin; and (3) there are differences in men and women with regard to pretransfusion erythropoiesis and response to transfusion. We found that hepcidin levels in patients with β-thalassemia major are associated with anemia, erythropoiesis, and iron stores; that suppression of erythropoiesis by transfusion is associated with an increase in hepcidin; and that compared with women pre- and posttransfusion, men had increased erythropoiesis and lower hepcidin.
Methods
Patients
The Southern Health thalassemia service (Melbourne, Australia) is the state center for management of thalassemia. Patients receive red cell transfusions and iron chelators in accordance with international recommendations.14 Adults with transfusion-dependent β-thalassemia were eligible for this study. Blood was collected immediately prior to transfusion, and patients were asked to return 5 days after transfusion for posttest sampling, when erythroid suppression was expected to correlate with maximal suppression.15 Data on the transfused units were collected.
Laboratory analysis
Samples were tested for Hb and reticulocyte count (Beckman Coulter LH750), ferritin, soluble transferrin receptor (sTfR), and erythropoietin (EPO) by immunoassay (Beckman Coulter DXi 800), C-reactive protein (CRP; Beckman Coulter DXc 800), GDF-15 (enzyme-linked immunosorbent assay; R&D Systems), and hepcidin (Enzyme Immunoassay; Bachem).
Normal values and definitions
The reference range for the Beckman Coulter sTfR assay established by the manufacturer in 189 healthy adults is 0.90 to 2.01 mg/L (mean, 1.35 mg/L). For EPO, the manufacturer’s upper limit of normal is 18.5 mIU/mL. Tanno et al16 suggested GDF-15 levels in normal individuals fall between 200 and 1150 pg/mL. In a study investigating effects of altitude on erythropoiesis and hepcidin in healthy participants of similar mean age (40 years) to patients in our study, Piperno et al17 reported a baseline mean EPO of 11.5 mU/mL and, using the same assay, GDF-15 of 338.7 pg/mL. Thus, erythroid activity was evaluated by patient sTfR divided by 1.35 mg/L,18 patient EPO divided by 11.5 mIU/mL, and patient GDF-15 divided by 338.7 pg/mL. Absolute hepcidin values vary between assays.19 Using the same assay (Bachem) used in our study, Talbot et al4 reported mean hepcidin concentrations of 14 ng/mL (standard deviation, 11 ng/mL) in healthy adults, and Choi et al20 identified a range of 3.2 to 66.9 ng/mL in non–iron-deficient Korean children. The hepcidin-ferritin ratio was calculated to normalize hepcidin relative to concomitant iron loading and should be ∼1 in normal controls.12,21 β-gene mutations were classified as β0 or β+ according to an international database.22 Blood volume was estimated using Nadler’s formula based on gender, weight, and height.23
Statistical considerations
Variables with a right-skewed distribution were log-transformed following addition of 1 to an approximate normal distribution, which is a standard procedure to enable parametric analysis of skewed data.17 Geometric means were calculated by exponentiation of the arithmetic mean of the log-variable, followed by subtraction of 1. Student t test was used to compare means between groups or pre- and posttransfusion. Pearson’s correlation was used to assess associations between indices. Change from pre to posttransfusion was evaluated by calculation of difference (posttransfusion minus pretransfusion) where variables were normally distributed and percentage change where variables were skewed. Univariate and then multiple linear regression was used to evaluate the independent relationship between included variables and hepcidin pre- and posttransfusion. Standardized (β) coefficients were calculated (where variables are standardized to have a variance of 1) to enable comparison between variables. The study had a power of 0.80 to detect a difference of 25% in normally distributed variables (assuming a standard deviation of 30% of the value of the mean of the variable) by t test and a power of 0.80 to be able to detect correlations between variables with r exceeding 0.5.
Ethics approval
The Southern Health Human Research Ethics Committee approved the study. All patients provided written consent in accordance with the Declaration of Helsinki.
Results
Pretransfusion
Thirty-one (male, n = 16; female, n = 15) patients with β-thalassemia major (β0/β0 = 3, β0/β+ = 14, β+/β+ = 11, Eβ-thalassemia = 1, unknown = 2) provided pretransfusion samples (Table 1). The mean duration since previous transfusion was 22 days (range, 13-36 days). Twenty-seven patients were receiving chelation with deferasirox (daily or twice daily) and 4 with desferrioxamine (4-6 nights per week).
Summary of patients included in the study
| Variable . | Overall . | Males . | Females . | P difference between genders . |
|---|---|---|---|---|
| N | 31 | 16 | 15 | |
| Age (years) | 40.5 [37.1, 43.8] | 42.3 [37.0, 47.5] | 38.5 [34.1, 43.0] | .2585 |
| Weight (kg) | 62.3 [56.9, 67.6] | 67.3 [61.6, 72.9] | 56.9 [47.8, 66.1] | .0462 |
| Height (cm) | 159.6 [155.4, 163.9] | 166.3 [161.1, 171.4] | 153.0 [147.7, 158.4] | .0006 |
| Days since previous transfusion | 22 [20, 24] | 22 [18,25] | 23 [20, 25] | .5701 |
| Number of red cell units transfused | 2.8 [2.6, 3.1] | 2.9 [2.5, 3.2] | 2.8 [2.4, 3.2] | .7835 |
| Transfusion volume (mL/kg)* | 11.9 [10.7, 13.2] | 11.0 [9.3, 12.7] | 12.9 [11.0, 14.8] | .1273 |
| Estimated patient blood volume (L)† | 3.91 [3.59, 4.22] | 4.46 [4.14, 4.78] | 3.36 [2.97, 3.74] | .0001 |
| Estimated milliliters transfused per liter blood volume† | 196.5 [175.2, 217.9] | 171.3 [143.4, 197.2] | 221.0 [190.9, 251.2] | .0122 |
| Mean age of transfused unit (days) | 16.1 [14.2, 18.0] | 15.7 [13.0, 18.4] | 16.5 [13.4, 19.6] | .6865 |
| Variable . | Overall . | Males . | Females . | P difference between genders . |
|---|---|---|---|---|
| N | 31 | 16 | 15 | |
| Age (years) | 40.5 [37.1, 43.8] | 42.3 [37.0, 47.5] | 38.5 [34.1, 43.0] | .2585 |
| Weight (kg) | 62.3 [56.9, 67.6] | 67.3 [61.6, 72.9] | 56.9 [47.8, 66.1] | .0462 |
| Height (cm) | 159.6 [155.4, 163.9] | 166.3 [161.1, 171.4] | 153.0 [147.7, 158.4] | .0006 |
| Days since previous transfusion | 22 [20, 24] | 22 [18,25] | 23 [20, 25] | .5701 |
| Number of red cell units transfused | 2.8 [2.6, 3.1] | 2.9 [2.5, 3.2] | 2.8 [2.4, 3.2] | .7835 |
| Transfusion volume (mL/kg)* | 11.9 [10.7, 13.2] | 11.0 [9.3, 12.7] | 12.9 [11.0, 14.8] | .1273 |
| Estimated patient blood volume (L)† | 3.91 [3.59, 4.22] | 4.46 [4.14, 4.78] | 3.36 [2.97, 3.74] | .0001 |
| Estimated milliliters transfused per liter blood volume† | 196.5 [175.2, 217.9] | 171.3 [143.4, 197.2] | 221.0 [190.9, 251.2] | .0122 |
| Mean age of transfused unit (days) | 16.1 [14.2, 18.0] | 15.7 [13.0, 18.4] | 16.5 [13.4, 19.6] | .6865 |
Arithmetic mean [95% confidence interval]; P calculated from 2-sample t test.
Assuming each bag contains 260 mL red cells (Australian Red Cross Blood Service red cell unit mean volume = 259 ± 23 mL).50
Nadler’s formula for total blood volume (TBV): men, TBV (mL) = 604 + (367 × height3 [m3]) + (32.2 × weight [kg]); women, TBV (mL) = 183 + (356 × height3 [m3]) + (33.1 × weight [kg]).
Figure 1 summarizes pretransfusion Hb together with indices of erythropoiesis and iron and shows the posttransfusion change. Pretransfusion, mean Hb was 101.9 g/L, and Hb for 29 of 31 patients exceeded 90 g/L, including 18 for whom it exceeded 100 g/L. Mean reticulocyte count was 83.5 × 109/L (within the normal range). Based on the sTfR, mean relative erythroid activity was 2.1. EPO (4.8 × mean), and GDF-15 (22.3 × mean) levels were also increased. Pretransfusion hepcidin concentrations were within the range reported in normal adults and children; however, the hepcidin-ferritin ratio was markedly <1 in all patients (mean, 0.018), indicating suppression of hepcidin out of proportion with the degree of iron loading.12,24
Pre- and posttransfusion indices of hematology, erythropoiesis, and iron physiology. There were 31 patients before transfusion and 26 after transfusion. Following transfusion, mean (A) Hb increased (mean pretransfusion 101.9 g/L [98.1, 105.7], posttransfusion 122.2 g/L [117.0, 127.4], P < .0001; change 20.5 g/L [16.1, 24.8]), (B) EPO decreased (pretransfusion 54.7 mIU/mL [41.3, 72.4], posttransfusion 25.6 mIU/mL [20.0, 32.8], P < .0001, percentage change −49.4% [−58.4, −40.5]), (C) GDF-15 decreased (pretransfusion 7556.2 pg/mL [6016.5, 9490.8], posttransfusion 4979.6 pg/mL [3910.8, 6340.5], P < .0001, percentage change −35.6% [−41.3, −29.9]), (D) sTfR did not significantly vary (pretransfusion 2.95 mg/L [2.43, 3.54], posttransfusion 2.79 mg/L [2.30, 3.35], P = .0937, percentage change −2.0% [-5.3, 1.3]), (E) ferritin increased (pretransfusion 987.7 ng/mL [726.2, 1343.2], posttransfusion 1086.3 ng/mL [806.2, 1463.6], P = .0021, percentage change 18.7% [8.3, 29.1]); (F) CRP did not vary significantly (pretransfusion 1.78 mg/L [1.11, 2.68], posttransfusion 1.88 mg/L [1.06, 3.02], P = .7423, percentage change 22.9% [−8.8, 54.6]); (G) hepcidin increased (pretransfusion 19.2 ng/mL [12.7, 29.8], posttransfusion 41.3 ng/mL [26.3, 64.5], P < .0001, percentage change 154.6% [108.9, 200.2]); and (H) hepcidin-ferritin ratio increased (pretransfusion 0.027 [0.019, 0.036], posttransfusion 0.054 [0.036, 0.072], P = .0001, percentage change 129.7% [75.0, 184.5]). Reticulocyte count (not shown) did not change (pretransfusion 83.6 × 109/L [60.6, 106.6], posttransfusion 80.8 × 109/L [53.4, 108.3], P = .8252).
Pre- and posttransfusion indices of hematology, erythropoiesis, and iron physiology. There were 31 patients before transfusion and 26 after transfusion. Following transfusion, mean (A) Hb increased (mean pretransfusion 101.9 g/L [98.1, 105.7], posttransfusion 122.2 g/L [117.0, 127.4], P < .0001; change 20.5 g/L [16.1, 24.8]), (B) EPO decreased (pretransfusion 54.7 mIU/mL [41.3, 72.4], posttransfusion 25.6 mIU/mL [20.0, 32.8], P < .0001, percentage change −49.4% [−58.4, −40.5]), (C) GDF-15 decreased (pretransfusion 7556.2 pg/mL [6016.5, 9490.8], posttransfusion 4979.6 pg/mL [3910.8, 6340.5], P < .0001, percentage change −35.6% [−41.3, −29.9]), (D) sTfR did not significantly vary (pretransfusion 2.95 mg/L [2.43, 3.54], posttransfusion 2.79 mg/L [2.30, 3.35], P = .0937, percentage change −2.0% [-5.3, 1.3]), (E) ferritin increased (pretransfusion 987.7 ng/mL [726.2, 1343.2], posttransfusion 1086.3 ng/mL [806.2, 1463.6], P = .0021, percentage change 18.7% [8.3, 29.1]); (F) CRP did not vary significantly (pretransfusion 1.78 mg/L [1.11, 2.68], posttransfusion 1.88 mg/L [1.06, 3.02], P = .7423, percentage change 22.9% [−8.8, 54.6]); (G) hepcidin increased (pretransfusion 19.2 ng/mL [12.7, 29.8], posttransfusion 41.3 ng/mL [26.3, 64.5], P < .0001, percentage change 154.6% [108.9, 200.2]); and (H) hepcidin-ferritin ratio increased (pretransfusion 0.027 [0.019, 0.036], posttransfusion 0.054 [0.036, 0.072], P = .0001, percentage change 129.7% [75.0, 184.5]). Reticulocyte count (not shown) did not change (pretransfusion 83.6 × 109/L [60.6, 106.6], posttransfusion 80.8 × 109/L [53.4, 108.3], P = .8252).
There were no associations between duration since previous transfusion and any pretransfusion index. The 4 patients (3 women and 1 man) receiving desferrioxamine had lower pretransfusion Hb (mean, 88.9 vs 103.9 g/L; P < .005, t test) compared with those taking deferasirox, but there were no differences in age or pretransfusion ferritin, EPO, sTfR, GDF-15, or hepcidin. Age was inversely associated with ferritin (r = −0.47, P = .0085) but not with hepcidin or any other index. By analysis of variance, severity of the β-globin genotype was not associated with Hb, erythropoiesis, or hepcidin.
Associations between pretransfusion indices and hepcidin
Figure 2 presents associations between pretransfusion Hb, indices of erythropoiesis, and hepcidin. Pretransfusion Hb was inversely associated with indices of erythropoiesis (EPO and GDF-15 but not sTfR). Table 2 presents results of univariate and multiple linear regression for associations with pretransfusion hepcidin. Hepcidin was positively associated with Hb and ferritin and inversely associated with EPO, sTfR, and GDF-15. Women had higher hepcidin levels.
Associations between Hb and indices of erythropoiesis and hepcidin pretransfusion and posttransfusion. Associations between Hb, erythropoiesis, iron stores, and hepcidin were evaluated in both the pretransfusion and posttransfusion state. (A) Pretransfusion Hb concentration was associated with indices of erythropoiesis GDF-15 (r = −0.54, P = .0019) and EPO (r = −0.61, P = .0004), but not sTfR (not shown, r = −0.14, P = .4682), and also with hepcidin (r = 0.47, P = .0094). (B) Pretransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.57, P = .0011); EPO (r = −0.48, P = .0101); and sTfR (r = −0.43, P = .0199). (C) Pretransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.56, P = .0015) but not with inflammation (CRP, r = 0.01, P = .9627). (D) Posttransfusion Hb was associated with erythropoiesis (GDF-15 [r = −0.58, P = .0018), EPO [r = −0.58, P = .0026]) and hepcidin (r = 0.60, P = .0011), but not sTfR (not shown, r = −0.29, P = .1563). (E) Posttransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.65, P = .0004); EPO (r = −0.71, P = .0001); and sTfR (r = −0.50, P = .0101). (F) Posttransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.44, P = .0258) but not with inflammation (CRP, r = 0.17, P = .4045).
Associations between Hb and indices of erythropoiesis and hepcidin pretransfusion and posttransfusion. Associations between Hb, erythropoiesis, iron stores, and hepcidin were evaluated in both the pretransfusion and posttransfusion state. (A) Pretransfusion Hb concentration was associated with indices of erythropoiesis GDF-15 (r = −0.54, P = .0019) and EPO (r = −0.61, P = .0004), but not sTfR (not shown, r = −0.14, P = .4682), and also with hepcidin (r = 0.47, P = .0094). (B) Pretransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.57, P = .0011); EPO (r = −0.48, P = .0101); and sTfR (r = −0.43, P = .0199). (C) Pretransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.56, P = .0015) but not with inflammation (CRP, r = 0.01, P = .9627). (D) Posttransfusion Hb was associated with erythropoiesis (GDF-15 [r = −0.58, P = .0018), EPO [r = −0.58, P = .0026]) and hepcidin (r = 0.60, P = .0011), but not sTfR (not shown, r = −0.29, P = .1563). (E) Posttransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.65, P = .0004); EPO (r = −0.71, P = .0001); and sTfR (r = −0.50, P = .0101). (F) Posttransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.44, P = .0258) but not with inflammation (CRP, r = 0.17, P = .4045).
Associations with hepcidin pre- and posttransfusion
| Variable . | Pretransfusion . | Posttransfusion . | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient [95% CI] . | β coefficient . | P . | R2 . | Coefficient [95% CI] . | β Coefficient . | P . | R2 . | |
| Univariate regression | ||||||||
| Age | −0.02 [−0.07, 0.03] | −0.14 | .461 | 0.02 | −0.01 [−0.06, 0.04] | −0.09 | .654 | 0.01 |
| Gender | −0.99 [−1.69, −0.30] | −0.48 | .007 | 0.23 | −1.30 [−2.01, −0.59] | −0.61 | .001 | 0.37 |
| Hb | 0.05 [0.01, 0.08] | 0.47 | .009 | 0.21 | 0.05 [0.02, 0.08] | 0.60 | .001 | 0.36 |
| Ferritin | 0.70 [0.30, 1.11] | 0.56 | .001 | 0.32 | 0.64 [0.08, 1.20] | 0.44 | .026 | 0.19 |
| CRP | 0.01 [−0.53, 0.56] | 0.01 | .963 | 0.00 | 0.22 [−0.32, 0.77] | 0.17 | .404 | 0.03 |
| EPO | −0.67 [−1.17, −0.17] | −0.48 | .010 | 0.23 | −1.35 [−1.93, −0.78] | −0.71 | <.001 | 0.51 |
| GDF-15 | −0.97 [−1.51, −0.42] | −0.56 | .001 | 0.32 | −1.17 [−1.75, −0.59] | −0.65 | <.001 | 0.42 |
| sTfR | −1.18 [−2.16, −0.20] | −0.43 | .020 | 0.18 | −1.58 [−2.75, −0.42] | −0.50 | .010 | 0.25 |
| Multiple regression | ||||||||
| Model 1 | ||||||||
| Gender | −0.66 [−1.26, −0.07] | −0.32 | .031 | 0.57 | −0.75 [−1.47, −0.03] | −0.35 | .041 | 0.57 |
| Ferritin | 0.49 [0.13, 0.86] | 0.40 | .010 | 0.34 [−0.12, 0.80] | 0.23 | .144 | ||
| Hb | 0.04 [0.02, 0.07] | 0.43 | .003 | 0.04 [0.01, 0.06] | 0.43 | .010 | ||
| Model 2 | ||||||||
| Gender | −0.46 [−1.09, 0.17] | −0.23 | .146 | 0.53 | −0.66 [−1.31, −0.02] | −0.31 | .045 | 0.68 |
| Ferritin | 0.58 [0.17, 0.98] | 0.43 | .007 | 0.36 [−0.08, 0.79] | 0.23 | .102 | ||
| EPO | −0.59 [−1.00, −0.18] | −0.42 | .007 | −1.01 [−1.53, −0.49] | 0.56 | .001 | ||
| Model 3 | ||||||||
| Gender | −0.12 [−0.82, 0.58] | −0.06 | .731 | 0.54 | −0.31 [−1.19, 0.57] | −0.15 | .475 | 0.58 |
| Ferritin | 0.58 [0.21, 0.96] | 0.47 | .004 | 0.50 [0.02, 0.97] | 0.34 | .041 | ||
| GDF-15 | −0.76 [−1.30, −0.21] | −0.45 | .008 | −0.96 [−1.65, −0.27] | −0.53 | .009 | ||
| Model 4 | ||||||||
| Gender | −0.28 [−1.01, 0.45] | −0.14 | .437 | 0.47 | −0.75 [−1.55, 0.05] | −0.35 | .066 | 0.51 |
| Ferritin | 0.60 [0.19, 1.00] | 0.48 | .006 | 0.43 [−0.07, 0.93] | 0.29 | .089 | ||
| sTfR | −0.89 [−1.80, 0.03] | −0.32 | .057 | −1.11 [−2.21, −0.01] | −0.35 | .049 | ||
| Variable . | Pretransfusion . | Posttransfusion . | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient [95% CI] . | β coefficient . | P . | R2 . | Coefficient [95% CI] . | β Coefficient . | P . | R2 . | |
| Univariate regression | ||||||||
| Age | −0.02 [−0.07, 0.03] | −0.14 | .461 | 0.02 | −0.01 [−0.06, 0.04] | −0.09 | .654 | 0.01 |
| Gender | −0.99 [−1.69, −0.30] | −0.48 | .007 | 0.23 | −1.30 [−2.01, −0.59] | −0.61 | .001 | 0.37 |
| Hb | 0.05 [0.01, 0.08] | 0.47 | .009 | 0.21 | 0.05 [0.02, 0.08] | 0.60 | .001 | 0.36 |
| Ferritin | 0.70 [0.30, 1.11] | 0.56 | .001 | 0.32 | 0.64 [0.08, 1.20] | 0.44 | .026 | 0.19 |
| CRP | 0.01 [−0.53, 0.56] | 0.01 | .963 | 0.00 | 0.22 [−0.32, 0.77] | 0.17 | .404 | 0.03 |
| EPO | −0.67 [−1.17, −0.17] | −0.48 | .010 | 0.23 | −1.35 [−1.93, −0.78] | −0.71 | <.001 | 0.51 |
| GDF-15 | −0.97 [−1.51, −0.42] | −0.56 | .001 | 0.32 | −1.17 [−1.75, −0.59] | −0.65 | <.001 | 0.42 |
| sTfR | −1.18 [−2.16, −0.20] | −0.43 | .020 | 0.18 | −1.58 [−2.75, −0.42] | −0.50 | .010 | 0.25 |
| Multiple regression | ||||||||
| Model 1 | ||||||||
| Gender | −0.66 [−1.26, −0.07] | −0.32 | .031 | 0.57 | −0.75 [−1.47, −0.03] | −0.35 | .041 | 0.57 |
| Ferritin | 0.49 [0.13, 0.86] | 0.40 | .010 | 0.34 [−0.12, 0.80] | 0.23 | .144 | ||
| Hb | 0.04 [0.02, 0.07] | 0.43 | .003 | 0.04 [0.01, 0.06] | 0.43 | .010 | ||
| Model 2 | ||||||||
| Gender | −0.46 [−1.09, 0.17] | −0.23 | .146 | 0.53 | −0.66 [−1.31, −0.02] | −0.31 | .045 | 0.68 |
| Ferritin | 0.58 [0.17, 0.98] | 0.43 | .007 | 0.36 [−0.08, 0.79] | 0.23 | .102 | ||
| EPO | −0.59 [−1.00, −0.18] | −0.42 | .007 | −1.01 [−1.53, −0.49] | 0.56 | .001 | ||
| Model 3 | ||||||||
| Gender | −0.12 [−0.82, 0.58] | −0.06 | .731 | 0.54 | −0.31 [−1.19, 0.57] | −0.15 | .475 | 0.58 |
| Ferritin | 0.58 [0.21, 0.96] | 0.47 | .004 | 0.50 [0.02, 0.97] | 0.34 | .041 | ||
| GDF-15 | −0.76 [−1.30, −0.21] | −0.45 | .008 | −0.96 [−1.65, −0.27] | −0.53 | .009 | ||
| Model 4 | ||||||||
| Gender | −0.28 [−1.01, 0.45] | −0.14 | .437 | 0.47 | −0.75 [−1.55, 0.05] | −0.35 | .066 | 0.51 |
| Ferritin | 0.60 [0.19, 1.00] | 0.48 | .006 | 0.43 [−0.07, 0.93] | 0.29 | .089 | ||
| sTfR | −0.89 [−1.80, 0.03] | −0.32 | .057 | −1.11 [−2.21, −0.01] | −0.35 | .049 | ||
Hepcidin, sTfR, ferritin, EPO, and CRP all log-transformed following addition of 1. Gender coded: female = 0; male = 1. β-coefficient, coefficient using variables standardized to have variance of 1.
Four multiple linear regression models adjusted for gender were developed to evaluate simultaneous coregulation of hepcidin by iron loading (ferritin) and anemia/erythropoiesis (measured by Hb, EPO, GDF-15, and sTfR respectively; Table 2). One index of erythropoiesis or anemia was included per model. Because CRP was not associated with hepcidin, it was not considered further. The models show that controlling for gender, iron stores, and erythropoiesis simultaneously influence hepcidin, with these factors explaining about half the variance in hepcidin (as indicated by the R2).
Posttransfusion
Twenty-six patients returned after a mean of 6 days for posttransfusion sampling. There were no differences in age, gender, or pretransfusion iron loading, Hb, indices of erythropoiesis, and hepcidin between patients who did and did not return. Change in Hb and indices of erythropoiesis, ferritin, CRP, and hepcidin are presented in Figure 1. In every patient, Hb and hepcidin increased (other than one in whom hepcidin remained undetectable) and EPO and GDF-15 fell. Change in sTfR was heterogeneous, with a reduction in 15 of 26 patients, whereas mean sTfR did not change (2.1 × mean). EPO was 2.2 × mean, whereas GDF-15, although reduced, remained ∼14.7 × mean. Mean hepcidin rose to 45.6 ng/mL, >2 standard deviations above the mean reported in normal individuals by Talbot et al,4 although within the range reported in healthy children.20 The hepcidin-ferritin ratio rose following transfusion but remained <1 (mean = 0.054).
Associations between posttransfusion indices and hepcidin
Reflecting the pretransfusion situation, posttransfusion Hb was inversely associated with indices of erythropoiesis (EPO and GDF-15 but not sTfR; Figure 2). Posttransfusion hepcidin was positively associated with Hb and ferritin and inversely associated with EPO, sTfR, and GDF-15 (Table 2). Again, women had higher hepcidin concentrations. Multiple linear regression showed that, controlling for gender, erythropoiesis continued to influence hepcidin posttransfusion, whereas ferritin was only associated when GDF-15 was used to indicate erythropoiesis. The R2 for each model was similar, indicating a similar effect for each measure of anemia/erythropoiesis on hepcidin. The effect of ferritin on hepcidin appeared weaker posttransfusion.
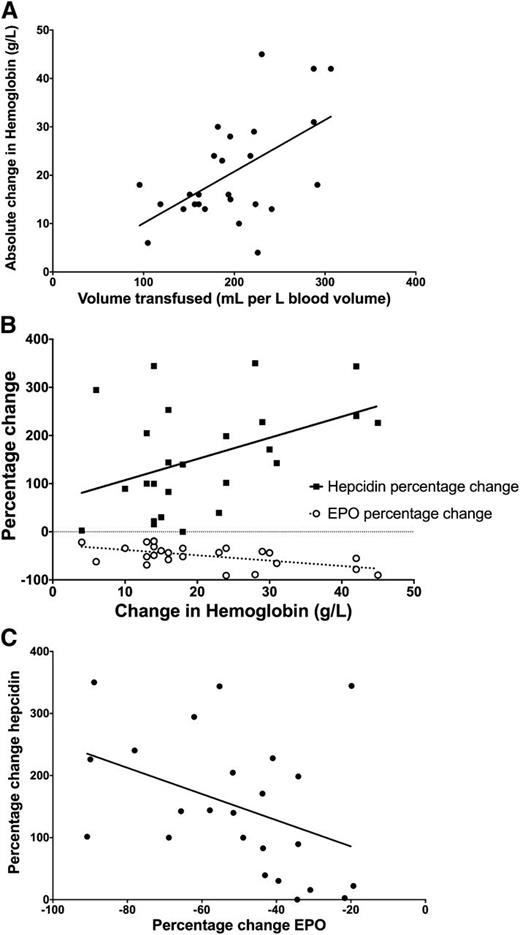
Associations between change in Hb, erythropoiesis, and hepcidin
Associations between changes pre- to posttransfusion were examined for variables that changed significantly posttransfusion (ie, Hb, EPO, GDF-15, ferritin, and hepcidin; Figure 3). The volume (mL) of red cells transfused per liter blood volume (and the volume [mL] per kilogram body weight [r = 0.53, P = .006], but not the absolute number of units transfused [P = .5598]) was associated with the posttransfusion increase in Hb. In turn, the change in Hb was associated with the reduction in EPO and increase in hepcidin. EPO and hepcidin changes were inversely correlated. Associations between changes in GDF-15 and hepcidin were not evident, nor was there an associated change in ferritin and hepcidin.
Associations between change from pre- to posttransfusion. Associations between indices that changed significantly from pre- to posttransfusion were evaluated (ie, Hb, ferritin, EPO, GDF-15, and hepcidin). (A) Transfused volume of red cells normalized for patient blood volume was positively associated with posttransfusion change in Hb (r = 0.56, P = .0033). (B) Posttransfusion change in Hb was inversely associated with change in EPO (r = −0.56, P = .0034) and positively with change in hepcidin (r = 0.44, P = .0300). (C) Percentage change in EPO was inversely associated with change in hepcidin (r = −0.41, P = .0489). Changes in GDF-15 and sTfR were not associated with change in hepcidin, nor was change in ferritin associated with change in hepcidin (not shown).
Associations between change from pre- to posttransfusion. Associations between indices that changed significantly from pre- to posttransfusion were evaluated (ie, Hb, ferritin, EPO, GDF-15, and hepcidin). (A) Transfused volume of red cells normalized for patient blood volume was positively associated with posttransfusion change in Hb (r = 0.56, P = .0033). (B) Posttransfusion change in Hb was inversely associated with change in EPO (r = −0.56, P = .0034) and positively with change in hepcidin (r = 0.44, P = .0300). (C) Percentage change in EPO was inversely associated with change in hepcidin (r = −0.41, P = .0489). Changes in GDF-15 and sTfR were not associated with change in hepcidin, nor was change in ferritin associated with change in hepcidin (not shown).
Comparisons between men and women
Male and female patients were of similar age, duration since previous transfusion, time to return posttransfusion, and pretransfusion Hb and reticulocyte count. Male patients were heavier, taller, and had higher blood volumes than women (Table 1). Although male patients were transfused a similar number of units (absolute and milligrams per kilogram) compared with women, male patients received a lower transfusion volume per liter blood volume compared with their female counterparts.
Comparisons of Hb and indices of erythropoiesis, ferritin, and hepcidin between the genders are presented in Table 3. Pretransfusion, male patients had higher sTfR and GDF-15 (indicating higher relative erythropoiesis), lower ferritin, and lower hepcidin compared with women. Posttransfusion, men had significantly lower Hb, higher reticulocyte count, lower ferritin, higher sTfR and GDF-15 (with EPO approaching significance, P = .053), and lower hepcidin compared with women.
Differences between men and women in pre- and posttransfusion indices of hematology, erythropoiesis, and iron physiology
| Variable . | Pretransfusion . | Posttransfusion . | ||||
|---|---|---|---|---|---|---|
| Men . | Women . | P difference between genders . | Men . | Women . | P difference between genders . | |
| N | 16 | 15 | 12 | 14 | ||
| Hb (g/L)* | 102.0 [95.6, 108.4] | 101.8 [97.0, 106.6] | .9583 | 116.9 [108.6, 125.3] | 126.8 [120.4, 133.2] | .0486 |
| Reticulocytes: absolute (109/L)* | 97.4 [64.9, 129.8] | 69.7 [34.6, 104.9] | .2255 | 110.7 [65.7, 155.7] | 55.3 [23.2, 87.4] | .0349 |
| Ferritin (ng/mL)† | 716.1 [481.8, 1064.0] | 1362.2 [866.1, 2145.5] | .0298 | 796.3 [549.6, 1154.7] | 1420.4 [912.0, 2215.2] | .0435 |
| CRP (mg/L)† | 1.53 [0.90, 2.36] | 2.06 [0.83, 4.13] | .4896 | 1.53 [0.66, 2.87] | 2.22 [0.86, 4.56] | .4725 |
| sTfR (mg/L)† | 3.66 [2.80, 4.72] | 2.35 [1.82, 2.97] | .0127 | 3.40 [2.55, 4.45] | 2.33 [1.81, 2.95] | .0351 |
| EPO (mIU/mL)† | 60.7 [38.8, 97.1] | 49.6 [34.2, 71.8] | .4737 | 33.2 [22.3, 49.0] | 20.9 [15.2, 28.7] | .0548 |
| Hepcidin (ng/mL)† | 11.3 [5.6, 22.0] | 32.2 [22.0, 47.0] | .0067 | 19.9 [10.1, 43.3] | 76.1 [55.0, 105.3] | .0009 |
| GDF-15 (pg/mL)† | 10267.0 [7007.9, 15041.9] | 5561.0 [4691.5, 6591.6] | .0039 | 7406.0 [5039.0, 10885.6] | 3543.4 [2933.1, 4280.6] | .0006 |
| Hepcidin-ferritin ratio† | 0.025 [0.014, 0.037] | 0.030 [0.015, 0.044] | .6116 | 0.038 [0.020, 0.057] | 0.068 [0.039, 0.098] | .0838 |
| Variable . | Pretransfusion . | Posttransfusion . | ||||
|---|---|---|---|---|---|---|
| Men . | Women . | P difference between genders . | Men . | Women . | P difference between genders . | |
| N | 16 | 15 | 12 | 14 | ||
| Hb (g/L)* | 102.0 [95.6, 108.4] | 101.8 [97.0, 106.6] | .9583 | 116.9 [108.6, 125.3] | 126.8 [120.4, 133.2] | .0486 |
| Reticulocytes: absolute (109/L)* | 97.4 [64.9, 129.8] | 69.7 [34.6, 104.9] | .2255 | 110.7 [65.7, 155.7] | 55.3 [23.2, 87.4] | .0349 |
| Ferritin (ng/mL)† | 716.1 [481.8, 1064.0] | 1362.2 [866.1, 2145.5] | .0298 | 796.3 [549.6, 1154.7] | 1420.4 [912.0, 2215.2] | .0435 |
| CRP (mg/L)† | 1.53 [0.90, 2.36] | 2.06 [0.83, 4.13] | .4896 | 1.53 [0.66, 2.87] | 2.22 [0.86, 4.56] | .4725 |
| sTfR (mg/L)† | 3.66 [2.80, 4.72] | 2.35 [1.82, 2.97] | .0127 | 3.40 [2.55, 4.45] | 2.33 [1.81, 2.95] | .0351 |
| EPO (mIU/mL)† | 60.7 [38.8, 97.1] | 49.6 [34.2, 71.8] | .4737 | 33.2 [22.3, 49.0] | 20.9 [15.2, 28.7] | .0548 |
| Hepcidin (ng/mL)† | 11.3 [5.6, 22.0] | 32.2 [22.0, 47.0] | .0067 | 19.9 [10.1, 43.3] | 76.1 [55.0, 105.3] | .0009 |
| GDF-15 (pg/mL)† | 10267.0 [7007.9, 15041.9] | 5561.0 [4691.5, 6591.6] | .0039 | 7406.0 [5039.0, 10885.6] | 3543.4 [2933.1, 4280.6] | .0006 |
| Hepcidin-ferritin ratio† | 0.025 [0.014, 0.037] | 0.030 [0.015, 0.044] | .6116 | 0.038 [0.020, 0.057] | 0.068 [0.039, 0.098] | .0838 |
Arithmetic mean [95% confidence interval]; P calculated from t test.
Geometric mean [95% confidence interval]; P calculated from t test of log-transformed data.
Age of blood
Finally, post hoc analysis was performed to study associations between age of the red cell units (defined as duration between collection date and transfusion date) and changes in Hb, erythropoiesis, and ferritin. The mean age of units transfused was 16.1 days. In 1 patient, all transfused units were ≤7 days; in a further 6 patients, all units were ≤14 days. There were no associations between mean unit age and change in Hb, ferritin, CRP, EPO, sTfR, GDF-15, or hepcidin, nor did patients who exclusively received units ≤14 days experience different changes in these parameters.
Discussion
Our study is the first to examine the effect of transfusion on erythropoiesis and, in turn, the effect of modulation of erythropoiesis on serum hepcidin in patients with β-thalassemia major. We found that hepcidin concentrations reflect competing influences from erythropoiesis, anemia, and iron overload and are dynamic over the intertransfusion interval, with changes reflecting suppression of erythropoiesis by transfusion-related increases in Hb. Furthermore, despite similar pretransfusion Hb levels, men have increased erythropoiesis compared with women, compounded by smaller posttransfusion Hb increments due to smaller transfusate volumes per liter blood volume.
Hepcidin has been previously measured in patients with β-thalassemia. In the only previous longitudinal study, Kearney et al12 reported that transfusion increased urinary hepcidin in patients with β-thalassemia major, reflecting our findings. Cross-sectional studies10,11 have shown that hepcidin in non–transfusion-dependent β-thalassemia is lower, and erythropoiesis higher, than in transfused β-thalassemia major, with inverse associations between indices of erythropoiesis and hepcidin. Studies in patients with β-thalassemia major have reported that posttransfusion hepcidin is relatively normal25,26 but that hepatic hepcidin expression and urinary hepcidin were suppressed for the degree of iron loading and chiefly influenced by erythropoiesis,27 reflecting our findings.
Observed differences in patterns of pretransfusion levels and posttransfusion changes of EPO, sTfR, and GDF-15 may reflect the different physiology and clinical significance of these indices. EPO closely correlated (inversely) with Hb pre- and posttransfusion, and EPO percentage change inversely correlated with Hb change. EPO rapidly rises in anemia as a result of anemia-induced hypoxia and falls as Hb is corrected.28 EPO levels are highest when anemia is due to marrow hypoplasia and are lower when anemia is due to dyserythropoiesis (ie, in thalassemia), perhaps because of erythroblast uptake of EPO.29 sTfR and GDF-15 both reflect erythropoiesis, but we observed different behavior between them. Transferrin receptors are chiefly expressed by erythroblasts,30 increasing from early to intermediate stages and decreasing with maturation. Thus, transferrin receptor mass reflects numbers of immature erythroid cells.31 We did not observe a significant pre- to posttransfusion change in sTfR in the group as a whole, and we did not identify associations between Hb and sTfR either pre- or posttransfusion. In our cohort, pretransfusion Hb exceeded 100 g/L in 18 patients, potentially considerably suppressing erythropoiesis (indicated by sTfR) both pretransfusion and over the intertransfusion interval. Relative stability of erythroid activity over the transfusion cycle in chronically transfused adult patients has been observed previously.9 Conversely, although GDF-15 fell following transfusion, it was markedly elevated pretransfusion and remained so posttransfusion. Expression of GDF-15 peaks in late erythroblasts and is also associated with erythroblast apoptosis,16 a feature of ineffective erythropoiesis in β-thalassemia.32 Ineffective erythropoiesis with tissue hypoxia and erythroblast apoptosis may induce the high levels of GDF-15 seen in thalassemia. Reflecting our data, GDF-15 has been found to be markedly elevated in β-thalassemia syndromes (eg, 11 512-127 254 pg/mL)8 and moderately elevated in other dyserythropoietic conditions, including congenital dyserythropoietic anemia33 and pyruvate kinase deficiency.34 Conversely, as discussed below, GDF-15 does not appear to increase as dramatically where erythropoiesis is physiologically increased (eg, altitude or following administration of EPO).35 Thus, the divergent patterns of EPO, sTfR, and GDF-15 may reflect differing physiologies of these parameters and provide insights into transfusion effects on erythropoiesis in thalassemia. EPO closely reflects anemia but may also reflect erythroid suppression. sTfR reflects overall erythropoietic activity but not necessarily ineffective erythropoiesis/dyserythropoiesis with apoptosis, which appears best reflected by GDF-15. Differential expression of these parameters may indicate that even adequately transfused patients with β-thalassemia, despite stable overall erythroid suppression, have ongoing ineffective erythropoiesis with apoptosis that fluctuates with transfusion.
In all patients, the hepcidin-ferritin ratio was markedly <1 both pre- and posttransfusion, indicating suppression of hepcidin that is out of proportion to the degree of iron loading and implying a suppressive effect from erythropoiesis.12 Although ferritin rose posttransfusion, it is unlikely that increasing iron stores caused the rise in hepcidin, because percentage changes in hepcidin and ferritin were not correlated. Furthermore, the rise in the hepcidin-ferritin ratio following transfusion despite the increase in ferritin indicates that hepcidin increased out of proportion to the increase in ferritin.
The mechanism for suppression of hepcidin in patients with thalassemia and other conditions with increased erythropoiesis remains uncertain, but several lines of evidence suggest an erythropoiesis-derived signal that inhibits hepcidin production. Sera from thalassemic patients suppresses Hamp expression in hepatoma cell lines,8,36 indicating the presence of the signal in serum and activity in vitro. The suppressive signal appears to override iron loading–induced BMP6-mediated signaling.37 Suppression of hepcidin by anemia and hypoxia is contingent on erythroid activity. For example, mice with induced anemia require an active erythroid compartment to suppress hepatic hepcidin expression.38 Hypoxia does not induce suppression of hepcidin if EPO-mediated erythropoiesis is inhibited.39 Our study has emulated these animal data by using transfusion to physiologically correct anemia, suppress erythropoiesis, and increase hepcidin.
Two molecules, GDF-15 and Twisted gastrulation protein homolog 1, have been identified through transcriptome analysis as putative erythroblast-derived factors that modulate hepcidin.8 Tanno et al8 showed that recombinant GDF-15 inhibited expression of hepcidin in hepatic cell lines, whereas depletion of GDF-15 in thalassemic serum reverses the suppressive effect on hepcidin expression. However, the relationship between GDF-15 and hepcidin regulation remains equivocal. For example, Gdf-15−/− mice subjected to phlebotomy appropriately suppress hepcidin, and Hbb th3/+ mice (a thalassemia model) do not express increased bone marrow Gdf-15.40 Hepcidin suppression in pregnancy is not associated with increased GDF-15, even though expanding maternal erythroid mass is one of the reasons for the increased iron requirement.41 Following stem cell transplantation, recovery of erythropoiesis is associated with suppression of hepcidin, which is not associated with rising GDF-15.42 Finally, when serum from thalassemic patients immunodepleted of GDF-15 was applied to hepatoma cells, the suppressive effect of serum on hepcidin expression was only partially reversed.8 GDF-15 may play a particular role in hepcidin suppression in ineffective erythropoiesis but appears to be only one of the factors involved. In vitro, Twisted gastrulation protein homolog 1 interferes with BMP-mediated hepcidin expression in human hepatocytes through inhibition of BMP-dependent sons of mothers against decapentaplegic homologues phosphorylation, and expression is increased in thalassemic mice.43 Human correlative studies are not yet available. Our findings do not provide evidence that hepcidin is regulated directly by GDF-15 or any other specific factor. Rather, our data confirm that erythroid activity is closely and dynamically associated with hepcidin, consistent with a potential secreted erythroid factor that suppresses hepcidin.
Guidelines for the management of β-thalassemia major advise transfusion to maintain a pretransfusion Hb at 90 to 105 g/L,14 based on studies indicating that, compared with hypertransfusion regimes, patients maintained in this range balance satisfactory suppression of erythropoiesis with manageable transfusional iron loading and reduced transfusion requirements.44 Cazzola et al18 reported that erythroid proliferation (measured by sTfR) was 1 to 2 times normal in patients with a pretransfusion Hb of 100 to 110 g/L, which is 1 to 4 times normal for Hb 90 to 100 g/L and 2 to 6 times normal in patients with Hb 85 to 90 g/L. The authors concluded that maintaining Hb concentrations >90 g/L should sufficiently balance the need to suppress erythropoiesis with transfused iron. Adoption of these pretransfusion Hb targets reduced transfusion requirements and eased iron loading.44 In our study, patients were receiving an individualized, stable, regular transfusion regimen based on their tolerable transfusion volume and a clinically and logistically acceptable intertransfusion interval. Pretransfusion erythroid activity (defined by sTfR) was 1 to 4 times normal in 24 of 28 patients with Hb >90 g/L; thus, our data support current recommendations.
Previous studies reporting erythropoiesis and hepcidin in thalassemia did not present comparisons between men and women. Multiple regression indicated that pre- and posttransfusion gender differences in hepcidin levels are partially mediated by differences in erythropoiesis. We observed evidence of increased erythropoiesis in men compared with women. We hypothesize that 2 mechanisms contribute to this difference. First, in nonthalassemic populations, despite similar EPO concentrations,45 Hb levels in men are generally higher than women, presumably due to androgen effects on erythropoiesis.28 Men may thus require higher Hb concentrations to suppress erythropoietic drive. Second, posttransfusion, smaller increments in Hb in men appear to perpetuate differences in erythropoiesis and hepcidin. The smaller rise in Hb in men may be explained by male patients receiving a lower transfusion dose per unit blood volume. Current guidelines do not account for gender differences in blood volume, which may result in men receiving a relatively smaller transfusion volume. We also noted that male patients had lower ferritin concentrations compared with womens. Although relatively lower transfusion volumes could be one explanation, differences in dosing and adherence to iron chelators also need to be considered. Although weight and height were inversely associated with hepcidin and positively associated with sTfR and GDF-15 (data not shown), these associations were no longer seen when controlling for gender. As the number of subjects in our study was relatively small, studies in other thalassemia patient groups are needed to establish whether gender differences observed here are present more generally.
Earlier studies in transfused children with β-thalassemia major showed that when children were anemic and transfusions delayed, iron absorption from ferrous sulfate and food is increased, whereas absorption is normal when measured shortly following transfusion when Hb is raised, predicting an interaction between erythropoiesis and hepcidin many years before hepcidin was discovered.46,47 Hepcidin regulates intestinal iron absorption, and its levels can predict erythrocyte incorporation of dietary iron.48 However, correlations between hepcidin and iron utilization in patients with β-thalassemia have not been evaluated, and thus, specific predictions of iron absorption based on hepcidin cannot be made. In chronically transfused patients with thalassemia, hepcidin levels resemble those in nonthalassemic individuals, potentially implying relatively normal dietary iron absorption, especially posttransfusion. Interestingly, the coefficient between hepcidin and Hb remained constant pre- and posttransfusion, indicating stability in the relationship between these indices.
Compared with transfusion of fresh blood, aged (40-42 days old) blood has been found to produce greater increases in serum ferritin, transferrin saturation, and non–transferrin-bound iron in healthy volunteers.49 We did not find evidence of an effect of blood storage age on changes in ferritin. However, only a few patients received exclusively fresh units, and further studies are needed to evaluate the effects of blood storage in β-thalassemia.
Unlike mouse models of thalassemia,2 age was not associated with hepcidin levels. This association may be mediated by iron loading and may be modified by chelator adherence. One patient appeared an outlier in our dataset: a 40-year-old man with pretransfusion Hb = 66 g/L; EPO = 244.7 IU/mL, sTfR = 4.1 mg/mL, GDF-15 = 33 464 pg/mL, hepcidin undetectable; posttransfusion Hb = 84 g/L, EPO = 160.5 IU/mL, GDF-15 = 21 931 pg/mL, hepcidin remained undetectable. The patient was retained in the analysis because he fulfilled inclusion criteria and recorded data were accurate. If this patient was excluded from the analysis, pretransfusion multiple regression models 2 and 4 and posttransfusion model 4 remained significant; associations between transfusion volume and change in Hb and between change in Hb and change in EPO and hepcidin remained significant, and differences between men and women in pretransfusion sTfR, GDF-15, and hepcidin and posttransfusion reticulocyte count, GDF-15 (with sTfR approaching significance, P = .055), and hepcidin persisted, indicating our findings are robust.
Our data may have clinical implications. Erythropoiesis varies over the transfusion cycle; thus, timing of measurement of indices for clinical and research purposes must be standardized (eg, immediately pretransfusion) or at least documented. Second, monitoring of EPO, sTfR, and GDF-15 could have a potentially valuable clinical role in the future in quantitatively and qualitatively evaluating erythropoiesis and thus optimizing transfusion dosing. Further studies that identify trends in these indices over time in patients, and correlate these indices with clinical implications of expanded erythropoiesis (eg, extramedullary hematopoiesis, osteoporosis, growth) may clarify the clinical role of these parameters. As hepcidin appears to integrate erythropoietic and iron-loading signals, clinical measurement of hepcidin (together with the hepcidin-ferritin ratio) may become a useful indicator of erythropoiesis and iron kinetics in complex patients. Our data also suggest that, reflecting the situation in nonthalassemic individuals, optimal pretransfusion Hb levels in men with β-thalassemia may be higher than for female patients, although corroboration in other cohorts is necessary. In all patients, the Hb increment is related to the transfusion volume relative to patient blood volume, and thus incorporation of the recipient blood volume into transfusion dosage calculations may be useful.
There is an Inside Blood commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are grateful for the kind assistance from the staff of the Medical Therapy Unit, Southern Health, in particular the study coordinator Ms Yoke Wong, the nurse unit manager Ms Joanne Shaw, the medical resident Dr Claire Sheeran, and the blood bank scientist Ms Kylie Rushford. Associate Professor Erica Wood and Dr Zoe McQuilten provided guidance with the development of the project. The authors thank the patients who participated in this research.
The work was supported by internal department funds. S.-R.P. is supported by a CJ Martin Early Career Fellowship from the National Health and Medical Research Council of Australia and a Haematology Society of Australia and New Zealand New Investigator Fellowship. D.M.F. is the recipient of a fellowship from the Australian Liver Foundation. G.J.A. is supported by a Senior Research Fellowship from the National Health and Medical Research Council of Australia.
Authorship
Contribution: S.-R.P. designed the research, collected, analyzed, and interpreted the data, performed statistical analysis, and wrote the manuscript; D.M.F. performed the hepcidin and GDF-15 assays and wrote the manuscript; D.K.B. designed the research and wrote the manuscript; G.J.A. designed the research, performed the hepcidin and GDF-15 assays, and wrote the manuscript; and all authors approved the final manuscript.
Conflict-of-interest disclosure: S.-R.P. has received an unrestricted research grant as a co-investigator from Vifor Pharma Ltd. The remaining authors declare no competing financial interests.
Present address for S.-R.P.: Molecular Immunology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, John Radcliffe Hospital, Oxford OX3 9DS, United Kingdom.
Correspondence: Sant-Rayn Pasricha, Nossal Institute for Global Health, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Carlton, Victoria 3010, Australia; e-mail: sant-rayn.pasricha@unimelb.edu.au.

![Figure 1. Pre- and posttransfusion indices of hematology, erythropoiesis, and iron physiology. There were 31 patients before transfusion and 26 after transfusion. Following transfusion, mean (A) Hb increased (mean pretransfusion 101.9 g/L [98.1, 105.7], posttransfusion 122.2 g/L [117.0, 127.4], P < .0001; change 20.5 g/L [16.1, 24.8]), (B) EPO decreased (pretransfusion 54.7 mIU/mL [41.3, 72.4], posttransfusion 25.6 mIU/mL [20.0, 32.8], P < .0001, percentage change −49.4% [−58.4, −40.5]), (C) GDF-15 decreased (pretransfusion 7556.2 pg/mL [6016.5, 9490.8], posttransfusion 4979.6 pg/mL [3910.8, 6340.5], P < .0001, percentage change −35.6% [−41.3, −29.9]), (D) sTfR did not significantly vary (pretransfusion 2.95 mg/L [2.43, 3.54], posttransfusion 2.79 mg/L [2.30, 3.35], P = .0937, percentage change −2.0% [-5.3, 1.3]), (E) ferritin increased (pretransfusion 987.7 ng/mL [726.2, 1343.2], posttransfusion 1086.3 ng/mL [806.2, 1463.6], P = .0021, percentage change 18.7% [8.3, 29.1]); (F) CRP did not vary significantly (pretransfusion 1.78 mg/L [1.11, 2.68], posttransfusion 1.88 mg/L [1.06, 3.02], P = .7423, percentage change 22.9% [−8.8, 54.6]); (G) hepcidin increased (pretransfusion 19.2 ng/mL [12.7, 29.8], posttransfusion 41.3 ng/mL [26.3, 64.5], P < .0001, percentage change 154.6% [108.9, 200.2]); and (H) hepcidin-ferritin ratio increased (pretransfusion 0.027 [0.019, 0.036], posttransfusion 0.054 [0.036, 0.072], P = .0001, percentage change 129.7% [75.0, 184.5]). Reticulocyte count (not shown) did not change (pretransfusion 83.6 × 109/L [60.6, 106.6], posttransfusion 80.8 × 109/L [53.4, 108.3], P = .8252).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/1/10.1182_blood-2012-12-471441/4/m_124f1.jpeg?Expires=1769083154&Signature=UhbiY9T6J1yYHT~Rv~X9EVjNi8fCD4lZ78Yt93GHIY4o0CEyGPOgT45Z7JEIrpen60MZgVSuY5kb0S3d-rzSkP59WvLiKnxKv9MEb~Agkt62kDCkdLJvdi1F5bEA0HSq6d90WsKMFlqDTLrffKVIdrVVi4cs83odImSR6uEHf0e0iWiEBnSkXA01NLnNB-YvZStZ67CUzmBwOVtpn9vYhiIbNvbjtNDuPpPrh2q-asriJrSVcpn7WVyru~SR-0Ua58tm-NcqYSB6KuAqkecEs7B0XQ4mDZNNupErhhZil5OYfHspNaQQcCeo-HtlS-gs346pfn5KjOkS34PA1cTtrg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 2. Associations between Hb and indices of erythropoiesis and hepcidin pretransfusion and posttransfusion. Associations between Hb, erythropoiesis, iron stores, and hepcidin were evaluated in both the pretransfusion and posttransfusion state. (A) Pretransfusion Hb concentration was associated with indices of erythropoiesis GDF-15 (r = −0.54, P = .0019) and EPO (r = −0.61, P = .0004), but not sTfR (not shown, r = −0.14, P = .4682), and also with hepcidin (r = 0.47, P = .0094). (B) Pretransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.57, P = .0011); EPO (r = −0.48, P = .0101); and sTfR (r = −0.43, P = .0199). (C) Pretransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.56, P = .0015) but not with inflammation (CRP, r = 0.01, P = .9627). (D) Posttransfusion Hb was associated with erythropoiesis (GDF-15 [r = −0.58, P = .0018), EPO [r = −0.58, P = .0026]) and hepcidin (r = 0.60, P = .0011), but not sTfR (not shown, r = −0.29, P = .1563). (E) Posttransfusion hepcidin was inversely associated with erythropoiesis: GDF-15 (r = −0.65, P = .0004); EPO (r = −0.71, P = .0001); and sTfR (r = −0.50, P = .0101). (F) Posttransfusion hepcidin was positively associated with iron loading (ferritin, r = 0.44, P = .0258) but not with inflammation (CRP, r = 0.17, P = .4045).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/122/1/10.1182_blood-2012-12-471441/4/m_124f2.jpeg?Expires=1769083154&Signature=4W9CaRUHhM0eZ9dPX4xJ3XYDByHW3hl~I1-ixpYfaXIza5SDpBwhG-9i7isqfJjpvvB4miGz69TJEJmve89v4qupX3AQwhFKSV1lDPplz9Q4ay4Z9E6SCBGkHRPD86Zuof6SDdL45kCaR5rru7~TYE4Rx5uSLYL~qGJR9zQUw6IDxryoV-dOISwx5Q7-9j~bovJcN8WMiy23WDJHxj7llm9lR3Zg8OxNreF6DXYizkrML1eBlBkQlFsezpGmEdRijQunUhYeEEiHWpS4ZKm~zhkOabpnJA4FByUeyqj5IrD2-cD0FxiH9xnP3qjDbZS7Kf9MrkHe6VNwXbzj02jfFQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)