Key Points
In AML1-ETO–positive AML cells, HDAC inhibitors induce autophagy, which acts as a prosurvival signal to limit HDAC-induced cell death.
In contrast to the fusion oncoproteins PML-RARA and breakpoint cluster region–abelson, AML1-ETO is not degraded by either basal- or drug-induced autophagy.
Abstract
The role of autophagy during leukemia treatment is unclear. On the one hand, autophagy might be induced as a prosurvival response to therapy, thereby reducing treatment efficiency. On the other hand, autophagy may contribute to degradation of fusion oncoproteins, as recently demonstrated for promyelocytic leukemia–retinoic acid receptor α and breakpoint cluster region–abelson, thereby facilitating leukemia treatment. Here, we investigated these opposing roles of autophagy in t(8;21) acute myeloid leukemia (AML) cells, which express the most frequently occurring AML fusion oncoprotein, AML1–eight-twenty-one (ETO). We demonstrate that autophagy is induced by AML1-ETO–targeting drugs, such as the histone deacetylase inhibitors (HDACis) valproic acid (VPA) and vorinostat. Furthermore, we show that autophagy does not mediate degradation of AML1-ETO but rather has a prosurvival role in AML cells, as inhibition of autophagy significantly reduced the viability and colony-forming ability of HDACi-treated AML cells. Combined treatment with HDACis and autophagy inhibitors such as chloroquine (CQ) led to a massive accumulation of ubiquitinated proteins that correlated with increased cell death. Finally, we show that VPA induced autophagy in t(8;21) AML patient cells, and combined treatment with CQ enhanced cell death. Because VPA and CQ are well-tolerated drugs, combinatorial therapy with VPA and CQ could represent an attractive treatment option for AML1-ETO–positive leukemia.
Introduction
Macroautophagy, hereafter referred to as autophagy, is a catabolic pathway that is upregulated during times of nutrient limitations or stress to maintain cellular metabolism and organelle integrity.1 Autophagy involves sequestration of cytoplasmic cargo, such as long-lived proteins, damaged organelles, and protein aggregates, into double-membrane vesicles termed autophagosomes, which fuse with lysosomes, leading to degradation of the contents by acidic hydrolases.1
There is currently a pressing need to understand in which settings autophagy should be inhibited and in which instances autophagy should be activated, to overcome drug resistance and optimize cancer treatment. Recent studies indicate that anticancer treatment may be hampered by the activation of autophagy as a prosurvival mechanism that prevents apoptosis and delays necrosis in the cancer cells.2,3 Thus, including autophagy inhibitors in cancer therapy could potentially overcome cancer drug resistance.4,5 However, autophagy has also been suggested to be a mediator of cell death in certain contexts,6 and it was recently demonstrated that autophagy facilitates basal and therapy-induced degradation of promyelocytic leukemia–retinoic acid receptor α (PML-RARA) and breakpoint cluster region–abelson, 2 frequently occurring fusion oncoproteins associated with acute promyelocytic leukemia and chronic myeloid leukemia (CML), respectively.7-10 Thus, in these instances, one would seek therapeutic options where autophagy is activated, rather than inhibited.
The most frequently occurring acute myeloid leukemia (AML) fusion oncoprotein, AML1–eight-twenty-one (ETO), is expressed in t(8;21) AML, and although this AML subtype is generally associated with a relatively favorable prognosis, more targeted and less toxic treatment than the current high-dose chemotherapy is warranted, particularly in treatment of relapsed or elderly patients.11 Histone deacetylase inhibitors (HDACis) have gained growing interest as anticancer agents because they potently induce cell cycle arrest, differentiation, and apoptosis of malignant cells,12 and interestingly, the HDACis valproic acid (VPA; Orfiril), a well-known anti-epileptic drug,13 and vorinostat (or SAHA; Zolinza), which is clinically approved for treatment of cutaneous T-cell lymphoma,14 have both been shown to induce partial differentiation and apoptosis in the t(8;21) AML model cell line Kasumi-1.15-20 Additionally, VPA was found to induce loss of AML1-ETO.18 Thus, VPA and other HDACis might be particularly relevant for therapy of AML1-ETO–expressing leukemia. Treatment with HDACis has been shown to affect autophagy in several types of cancer cells, including CML,21 Jurkat T-leukemia,22 colon cancer,23 hepatocellular carcinoma,24 nerve sheath tumor,25 breast cancer,26 and glioblastoma,27 with variable effects on cell viability.
In the current study, we demonstrate that the HDACis VPA and vorinostat activate autophagy in t(8;21) AML cells. However, in contrast to previous studies on PML-RARA and breakpoint cluster region–abelson, we show that the degradation of AML1-ETO is not mediated by autophagy, indicating that activation of autophagy is less likely to be beneficial in the treatment of t(8;21)-positive AML. Rather, we find that HDACis activate prosurvival autophagy, because inhibition of autophagy potentiated the apoptotic effect of HDACis in t(8;21) AML cells. These results indicate that inhibition of autophagy may be useful in the treatment of t(8;21) AML.
Methods
Materials
Oridonin, vorinostat, chloroquine (CQ), RNase, Hoechst 33342, valine, N-acetyl cysteine (NAC), and VPA were all from Sigma-Aldrich (St. Louis, MO). Orfiril (100 mg/mL VPA intravenous formulation) was from Desitin Arzneimittel (Hamburg, Germany). Bafilomycin A1 (Baf) was from Enzo Life Sciences (Farmingdale, NY). Propidium iodide (PI), poly-d-lysine, and zVAD-fmk were from EMD Millipore Corporation (Billerica, MA). [14C]Valine was from PerkinElmer (Waltham, MA).
AML cell lines
The 2 available human t(8;21)-positive AML cell lines, Kasumi-1 and SKNO-1, were used in addition to the t(8;21)-negative AML cell line HL60. The cells were maintained according to standard growth criteria as described in detail in the supplemental Methods on the Blood Web site. The cells were treated with VPA at 1.5 mM and vorinostat at 1 µM unless otherwise stated. The autophagy inhibitors Baf and CQ were routinely used at concentrations of 20 nM and 50 µM, respectively. Cells were pretreated with the inhibitors for 30 minutes before addition of VPA or vorinostat, and the incubation was continued for 16 hours in the presence of inhibitors.
Patient samples
t(8;21)-positive or -negative AML samples (supplemental Table 1) were collected after written informed consent from patients at the Aarhus University Hospital (Aarhus, Denmark), or at Haukeland University Hospital (Bergen, Norway). Mononuclear cells were obtained by Lymphoprep (Axis Shield, Oslo, Norway) density gradient centrifugation of peripheral blood or bone marrow at the time of collection. Patients provided informed consent in accordance with the Declaration of Helsinki. All patient materials were used according to protocols approved by the regional Ethics Committees for the Aarhus County (approval number M-2007-0171) and Regional Committees for Medical and Health Research Ethics West, respectively. Primary AML cells were cultured at 5 × 105 cells/mL in StemSpan SFEM (StemCell Technologies, Vancouver, Canada) supplemented with interleukin-3, Flt3 ligand, and stem cell factor (all at 20 ng/mL; R&D Systems, Minneapolis, MN).
Long-lived protein degradation assay
Cells were incubated for 24 hours with 0.25 μCi/mL l-[14C]valine–supplemented medium, followed by a 4-hour chase in fresh medium containing 10 mM nonradioactive l-valine to allow degradation of short-lived proteins. Next, the cells were washed and treated with VPA or vorinostat for 16 hours in the absence or presence of lysosomal inhibitors. Incubation in Hank’s balanced salt solution for 4 hours served as a positive control. Cellular protein was precipitated with trichloracetic acid, and percent degradation was assessed as the acid-soluble radioactivity divided by the total radioactivity.
Immunofluorescence
Staining of endogenous LC3 and quantification of spots were performed as described in detail in the supplemental Methods. Pictures were taken using an automated Cell Observer microscope (Carl Zeiss, Jena, Germany). Quantification of LC3 spots was performed by the spot detection protocol in the PhysiologyAnalyst module of the AxioVision ASSAYbuilder software.
Immunoblotting
Immunoblotting was performed as described in the supplemental Methods.
Flow cytometry
For determination of cell viability, treated cells were stained with PI (5 µg/mL) for 15 minutes at room temperature before analysis on a FACSCalibur flow cytometer (BD Biosciences, San Jose, CA). Sub-diploid DNA contents were determined by fixation of cells in 70% ethanol before treatment with PI (20 µg/mL) and RNase (40 µg/mL) for 45 minutes and fluorescence-activated cell sorter analysis.
Colony formation assay
Cells were treated with VPA or vorinostat alone or in combination with CQ for 16 hours. Subsequently, 800 cells were seeded per dish in MethoCult Express medium (StemCell Technologies). Colonies (>20 cells) were counted after 8 days from duplicate dishes by a blinded scorer.
Small interfering RNA transfection
Cells were transfected in a nucleofector device (Amaxa Biosciences, Basel, Switzerland) according to the manufacturer’s description as described in detail in the supplemental Methods.
Statistical analysis
Mean values ± standard error of the mean were calculated for each condition. The statistical significance of the differences was determined by paired Student t test: *P < .05; **P < .01; ***P < .001.
Results
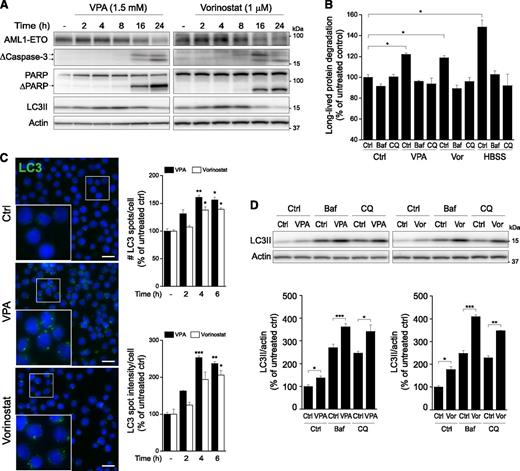
AML1-ETO–targeting HDACis VPA and vorinostat induce autophagy and apoptosis in Kasumi-1 cells
Treatment of the t(8;21) AML cell line Kasumi-1 with VPA has been reported to induce apoptosis and AML1-ETO catabolism,18,28,29 but it is not known whether autophagy plays a role in these processes. To study whether autophagy mediates degradation of AML1-ETO, Kasumi-1 cells were treated with VPA or the unrelated HDACi, vorinostat.14 As expected, VPA induced a gradual reduction in AML1-ETO protein levels with time, and a similar reduction was induced by vorinostat (Figure 1A; supplemental Figure 1A). The loss of AML1-ETO protein at 16 hours was not reflected by reduced transcription (supplemental Figure 1B). Concomitant with oncoprotein catabolism, apoptosis was induced by both drugs, as demonstrated by cleavage of pro-caspase-3 to its active forms and generation of the caspase-3–specific 89-kDa poly(ADP-ribose) polymerase (PARP) cleavage fragment (Figure 1A; supplemental Figure 1C). Moreover, induction of autophagy by the 2 HDACis was suggested by enhanced protein levels of the autophagosome marker LC3II (Figure 1A; supplemental Figure 1D). LC3II is generated by conjugation of LC3 to phosphatidylethanolamine in the autophagosome membrane during autophagy activation and is regarded as an indicator of autophagosome number.30 To assess whether the HDACis affected autophagic activity, we measured the degradation of long-lived proteins, which are bona fide autophagy substrates. Strikingly, both VPA and vorinostat significantly increased long-lived protein degradation (Figure 1B), increasing to ∼40% of the level induced by amino acid starvation, a potent inducer of autophagy. This increased protein degradation was completely reversed by 2 well-known inhibitors of autolysosomal degradation, Baf and CQ, confirming that the degradation was mediated by autophagy (Figure 1B).
VPA or vorinostat activates autophagy in Kasumi-1 cells. (A) Kasumi-1 cells were treated with VPA or vorinostat for the indicated hours, and total cell lysates were prepared for immunoblotting. The blots were probed with the indicated antibodies. Blots from 1 representative experiment are shown. Similar results were obtained by probing for AML1-ETO using an AML1-reactive antibody (data not shown). AML1-ETO migrates more or less as a doublet.47 (B) Kasumi-1 cells were treated with VPA or vorinostat (Vor) for 16 hours in the presence or absence of autolysosomal inhibitors, and autophagic activity was measured as degradation of long-lived proteins. Starvation in Hank’s balanced salt solution was used as a positive control. (C) Kasumi-1 cells were treated with VPA or vorinostat for 2 to 6 hours and then fixed and prepared for immunofluorescence staining of endogenous LC3 (green) and Hoechst staining of nuclei (blue). (Left) Representative images from the 4-hour time point are shown. Scale bar, 20 µm. (Right) Mean number of LC3 spots per cell and the mean intensity of LC3 spot pixels per cell were quantified from 1000 to 3000 cells per condition per experiment. The asterisks denote the statistical significances compared with the untreated control. (D) Autophagic flux was determined in Kasumi-1 cells by treatment with VPA or vorinostat for 4 hours in the presence or absence of Baf or CQ for the final 2 hours. Total cell lysates were prepared for immunoblotting, and the blots were probed with antibodies against LC3 and actin. Blots from 1 representative experiment are shown. The relative levels of LC3II were normalized to actin. All bars show mean values ± standard error of the mean (SEM) quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
VPA or vorinostat activates autophagy in Kasumi-1 cells. (A) Kasumi-1 cells were treated with VPA or vorinostat for the indicated hours, and total cell lysates were prepared for immunoblotting. The blots were probed with the indicated antibodies. Blots from 1 representative experiment are shown. Similar results were obtained by probing for AML1-ETO using an AML1-reactive antibody (data not shown). AML1-ETO migrates more or less as a doublet.47 (B) Kasumi-1 cells were treated with VPA or vorinostat (Vor) for 16 hours in the presence or absence of autolysosomal inhibitors, and autophagic activity was measured as degradation of long-lived proteins. Starvation in Hank’s balanced salt solution was used as a positive control. (C) Kasumi-1 cells were treated with VPA or vorinostat for 2 to 6 hours and then fixed and prepared for immunofluorescence staining of endogenous LC3 (green) and Hoechst staining of nuclei (blue). (Left) Representative images from the 4-hour time point are shown. Scale bar, 20 µm. (Right) Mean number of LC3 spots per cell and the mean intensity of LC3 spot pixels per cell were quantified from 1000 to 3000 cells per condition per experiment. The asterisks denote the statistical significances compared with the untreated control. (D) Autophagic flux was determined in Kasumi-1 cells by treatment with VPA or vorinostat for 4 hours in the presence or absence of Baf or CQ for the final 2 hours. Total cell lysates were prepared for immunoblotting, and the blots were probed with antibodies against LC3 and actin. Blots from 1 representative experiment are shown. The relative levels of LC3II were normalized to actin. All bars show mean values ± standard error of the mean (SEM) quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
In agreement with the observed increase in autophagic activity, VPA and vorinostat significantly increased the number of autophagosomes, as indicated by the typical punctuate staining pattern observed by immunofluorescence staining of endogenous LC3 (Figure 1C). Moreover, both HDACis appeared to enhance de novo autophagosome formation in Kasumi-1 cells, as the levels of LC3II were significantly higher in cells treated with VPA or vorinostat in combination with Baf and CQ than in cells treated with the lysosomal inhibitors alone (Figure 1D). Interestingly, the increase in LC3II protein levels correlated with increased LC3B mRNA levels (supplemental Figure 1D-E), indicating that VPA and vorinostat regulate autophagy at the transcriptional level. In summary, these data clearly demonstrate that the AML1-ETO–targeting drugs VPA and vorinostat induce autophagy in addition to apoptosis in the AML1-ETO–positive cell line Kasumi-1.
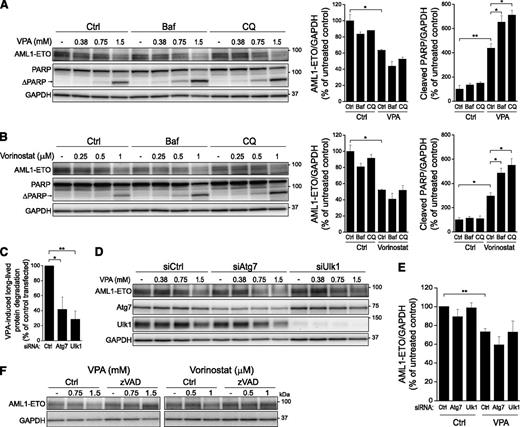
AML1-ETO is not degraded by autophagy
Having observed that VPA and vorinostat induce autophagy concomitant with loss of AML1-ETO, we next investigated whether autophagy is responsible for AML1-ETO degradation. To this end, AML1-ETO protein levels were quantified in Kasumi-1 cells treated with increasing concentrations of VPA or vorinostat in the absence or presence of the autophagy inhibitors Baf or CQ. AML1-ETO did not accumulate by inhibition of basal autophagy, and neither Baf nor CQ reversed VPA- or vorinostat-induced catabolism of this fusion protein (Figure 2A-B). The same was observed when using an unrelated AML1-ETO–targeting drug, the plant diterpenoid oridonin. Although oridonin induced autophagy concomitantly with loss of AML1-ETO, the reduction in AML1-ETO was not reversed in the presence of autolysosomal inhibitors (supplemental Figure 2). These results indicate that neither basal- nor drug-induced turnover of the fusion oncoprotein is mediated by autophagy. This was further confirmed by small interfering RNA (siRNA)-mediated knockdown of the core autophagic components Atg7 and Ulk1 (supplemental Figure 3A). Whereas depletion of these proteins strongly inhibited VPA-induced autophagy as assessed by long-lived protein degradation (Figure 2C), HDACi-induced loss of AML1-ETO was not reversed (Figure 2D-E; supplemental Figure 3B).
AML1-ETO is not degraded by autophagy. Kasumi-1 cells were treated with the indicated concentrations of (A) VPA or (B) vorinostat for 16 hours in the presence or absence of Baf or CQ. Cell lysates were prepared for immunoblotting, and the blots were probed with the indicated antibodies. Representative blots are shown. (Right) The relative band intensities of AML1-ETO and cleaved PARP at 1.5 mM VPA and 1 μM vorinostat were normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). (C) Kasumi-1 cells transfected with siRNA oligoes against Atg7 and Ulk1 were treated with VPA for 16 hours, and degradation of long-lived proteins was quantified. The VPA-induced degradation of long-lived proteins in cells transfected with siAtg7 or siUlk1 was compared with the VPA-induced protein degradation in siCtrl-transfected cells to demonstrate inhibition of autophagy. (D-E) Cells transfected as in C were treated with VPA at the indicated concentrations for the last 16 hours, and total cell lysates were prepared for immunoblotting. AML1-ETO was detected by an ETO-specific antibody. (E) The relative band intensities of AML1-ETO at 1.5 mM VPA were normalized to GAPDH. (F) VPA- or vorinostat-induced degradation of AML1-ETO is inhibited by caspase-inhibitor. Kasumi-1 cells were treated with zVAD-fmk (20 µM) for 30 minutes before addition of the indicated concentrations of VPA or vorinostat, and the incubation was continued for 16 hours. Total cell lysates were prepared for immunoblotting, and the blots were probed with antibodies against ETO and GAPDH. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01.
AML1-ETO is not degraded by autophagy. Kasumi-1 cells were treated with the indicated concentrations of (A) VPA or (B) vorinostat for 16 hours in the presence or absence of Baf or CQ. Cell lysates were prepared for immunoblotting, and the blots were probed with the indicated antibodies. Representative blots are shown. (Right) The relative band intensities of AML1-ETO and cleaved PARP at 1.5 mM VPA and 1 μM vorinostat were normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). (C) Kasumi-1 cells transfected with siRNA oligoes against Atg7 and Ulk1 were treated with VPA for 16 hours, and degradation of long-lived proteins was quantified. The VPA-induced degradation of long-lived proteins in cells transfected with siAtg7 or siUlk1 was compared with the VPA-induced protein degradation in siCtrl-transfected cells to demonstrate inhibition of autophagy. (D-E) Cells transfected as in C were treated with VPA at the indicated concentrations for the last 16 hours, and total cell lysates were prepared for immunoblotting. AML1-ETO was detected by an ETO-specific antibody. (E) The relative band intensities of AML1-ETO at 1.5 mM VPA were normalized to GAPDH. (F) VPA- or vorinostat-induced degradation of AML1-ETO is inhibited by caspase-inhibitor. Kasumi-1 cells were treated with zVAD-fmk (20 µM) for 30 minutes before addition of the indicated concentrations of VPA or vorinostat, and the incubation was continued for 16 hours. Total cell lysates were prepared for immunoblotting, and the blots were probed with antibodies against ETO and GAPDH. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01.
Caspase-3 has been reported to mediate AML1-ETO cleavage.28,31 Because both VPA and vorinostat induced cleavage of pro-caspase-3 and PARP, concomitant with the loss of AML1-ETO (Figures 1A and 2A-B), we next tested whether caspases were involved in drug-induced AML1-ETO catabolism. Indeed, blocking caspase activity with the pan-caspase inhibitor zVAD-fmk efficiently reversed drug-induced loss of AML1-ETO (Figure 2F; supplemental Figure 4). Thus, we conclude that, although autophagy is induced by the AML1-ETO–targeting drugs VPA and vorinostat, caspases appear to be the major effectors of AML1-ETO loss. Notably, recent data showed that the caspase-3 cleavage fragment of AML1-ETO, ΔAML1-ETO, was stabilized by oridonin and responsible for oridonin toxicity,29,32 and we could indeed detect this fragment in oridonin-treated cells (supplemental Figure 4). However, as this fragment was hardly visible in cells treated with VPA or vorinostat, it is less likely that it mediates the apoptotic effect of these HDACis and is rather subject to further catabolism (supplemental Figure 4; data not shown).
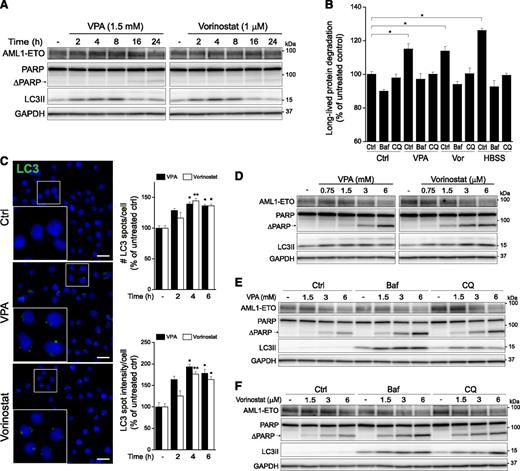
The results obtained in Kasumi-1 cells were corroborated by parallel experiments in another t(8;21) positive cell line, SKNO-1. Treatment of SKNO-1 cells with VPA- or vorinostat at the concentrations used in Kasumi-1 cells (1.5 mM and 1 μM, respectively) clearly induced autophagy, as measured by LC3II accumulation, increased degradation of long-lived proteins, and LC3 puncta formation (Figure 3A-C), but had little or no effect on AML1-ETO levels and PARP cleavage (Figure 3A). At higher concentrations of VPA and vorinostat (3-6 mM and 3-6 μM, respectively), AML1-ETO was reduced concomitant with potent cleavage of PARP (Figure 3D). However, and in line with the data obtained in Kasumi-1 cells, cotreatment with Baf or CQ did not reverse HDACi-induced loss of AML1-ETO in SKNO-1 cells (Figure 3E-F). Together, these data further support the conclusion that autophagy is not responsible for the degradation of AML1-ETO.
VPA and vorinostat induce autophagy without reducing the AML1-ETO levels in SKNO-1 cells. (A) SKNO-1 cells were treated with VPA or vorinostat for the indicated hours, and total cell lysates were prepared for immunoblotting. The blots were probed with the indicated antibodies, and GAPDH was used as a loading control. Blots from 1 representative experiment are shown. (B) SKNO-1 cells were treated with VPA or vorinostat (Vor) for 16 hours in the presence or absence of autolysosomal inhibitors, and autophagic activity was measured as degradation of long-lived proteins. Starvation in Hank’s balanced salt solution was used as a positive control. (C) SKNO-1 cells were treated with VPA or vorinostat for 2 to 6 hours and then fixed and prepared for immunofluorescence staining of endogenous LC3 (green) and Hoechst staining of nuclei (blue). Representative images from the 4-hour time point are shown. Scale bar, 20 µm. (Right) The mean number of LC3 spots per cell and the mean intensity of LC3 spot pixels per cell were quantified from 1000 to 2000 cells per condition per experiment. The asterisks denote the statistical significances compared with the untreated control. (D-F) SKNO-1 cells were treated with the indicated concentrations of VPA and vorinostat for 16 hours in the absence or presence of autolysosomal inhibitors. Total cell lysates were prepared for immunoblotting with the indicated antibodies, and representative blots are shown. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01.
VPA and vorinostat induce autophagy without reducing the AML1-ETO levels in SKNO-1 cells. (A) SKNO-1 cells were treated with VPA or vorinostat for the indicated hours, and total cell lysates were prepared for immunoblotting. The blots were probed with the indicated antibodies, and GAPDH was used as a loading control. Blots from 1 representative experiment are shown. (B) SKNO-1 cells were treated with VPA or vorinostat (Vor) for 16 hours in the presence or absence of autolysosomal inhibitors, and autophagic activity was measured as degradation of long-lived proteins. Starvation in Hank’s balanced salt solution was used as a positive control. (C) SKNO-1 cells were treated with VPA or vorinostat for 2 to 6 hours and then fixed and prepared for immunofluorescence staining of endogenous LC3 (green) and Hoechst staining of nuclei (blue). Representative images from the 4-hour time point are shown. Scale bar, 20 µm. (Right) The mean number of LC3 spots per cell and the mean intensity of LC3 spot pixels per cell were quantified from 1000 to 2000 cells per condition per experiment. The asterisks denote the statistical significances compared with the untreated control. (D-F) SKNO-1 cells were treated with the indicated concentrations of VPA and vorinostat for 16 hours in the absence or presence of autolysosomal inhibitors. Total cell lysates were prepared for immunoblotting with the indicated antibodies, and representative blots are shown. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01.
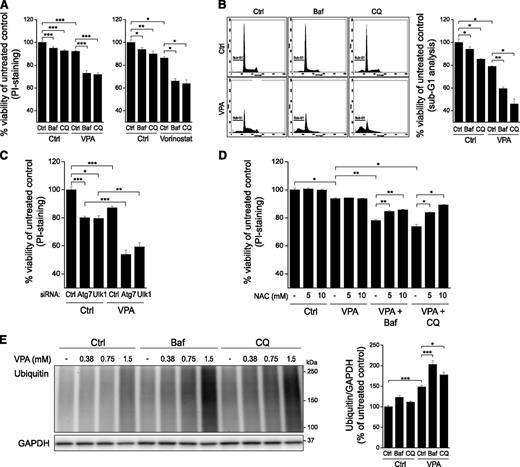
Autophagy promotes survival of Kasumi-1 cells by limiting drug-induced accumulation of ubiquitinated proteins
Having ruled out autophagy as a mediator of AML1-ETO degradation, we next investigated the effect of drug-induced autophagy on the viability of t(8;21) AML cells. HDACi treatment alone induced a modest reduction in cell viability, as assessed by PI exclusion, but most importantly, the combination with autolysosomal inhibitors significantly potentiated the toxic effect of VPA and vorinostat in a supra-additive manner (Figure 4A). Cotreatment with VPA or vorinostat and autophagy inhibitors also significantly increased the cleavage of PARP (Figure 2A-B), indicating enhanced caspase activity and apoptosis. Indeed, similar results were obtained when determining sub-diploid DNA contents of fixed and PI-stained cells treated with VPA and autophagy inhibitors (Figure 4B), further indicating the apoptotic nature of the cell death induced by combined drug treatments. The prosurvival role of VPA-induced autophagy in Kasumi-1 cells was further and more specifically demonstrated by siRNA-mediated knockdown of Atg7 and Ulk1; inhibition of autophagy by depletion of these core autophagy components significantly potentiated the toxicity of VPA (Figure 4C). Notably, Baf and CQ had minor effects on cell viability in Ulk1 knockdown cells (supplemental Figure 5), indicating that the toxic effect of these autolysosomal inhibitors was mainly caused by inhibition of autophagy in drug-treated AML cells.
Cell death induced by combined treatment with VPA/vorinostat and autophagy inhibitors depends on ROS and correlates with accumulation of ubiquitinated proteins. (A) Kasumi-1 cells were treated with VPA or vorinostat in the absence or presence of Baf or CQ for 16 hours. Cell viability was determined by fluorescence-activated cell sorter (FACS) analysis of PI-stained cells. (B) Kasumi-1 cells were treated with VPA for 16 hours in the absence or presence of Baf or CQ before fixation and PI staining for sub-G1 analysis. The figure shows representative histograms and presentation of cell viability as the fraction of non–sub-G1 cells. (C) Kasumi-1 cells transfected with siRNA oligoes against Atg7 and Ulk1 were treated with VPA for the last 16 hours. Cell viability was determined by FACS analysis of PI-stained cells. (D) Kasumi-1 cells were pretreated with NAC (5 or 10 mM) for 1 hour before addition of Baf or CQ. Then after 30 minutes, VPA was added, and the incubation was continued for 16 hours. Cell viability was determined by FACS analysis of PI-stained cells. (E) Cells were treated with the indicated concentrations of VPA for 16 hours in the absence or presence of Baf or CQ, and total cell lysates were prepared for immunoblotting. The blots were probed with antibodies against ubiquitin and GAPDH. Blots from 1 representative experiment are shown. (Right) Relative band intensities of ubiquitin at 1.5 mM VPA were normalized to GAPDH. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
Cell death induced by combined treatment with VPA/vorinostat and autophagy inhibitors depends on ROS and correlates with accumulation of ubiquitinated proteins. (A) Kasumi-1 cells were treated with VPA or vorinostat in the absence or presence of Baf or CQ for 16 hours. Cell viability was determined by fluorescence-activated cell sorter (FACS) analysis of PI-stained cells. (B) Kasumi-1 cells were treated with VPA for 16 hours in the absence or presence of Baf or CQ before fixation and PI staining for sub-G1 analysis. The figure shows representative histograms and presentation of cell viability as the fraction of non–sub-G1 cells. (C) Kasumi-1 cells transfected with siRNA oligoes against Atg7 and Ulk1 were treated with VPA for the last 16 hours. Cell viability was determined by FACS analysis of PI-stained cells. (D) Kasumi-1 cells were pretreated with NAC (5 or 10 mM) for 1 hour before addition of Baf or CQ. Then after 30 minutes, VPA was added, and the incubation was continued for 16 hours. Cell viability was determined by FACS analysis of PI-stained cells. (E) Cells were treated with the indicated concentrations of VPA for 16 hours in the absence or presence of Baf or CQ, and total cell lysates were prepared for immunoblotting. The blots were probed with antibodies against ubiquitin and GAPDH. Blots from 1 representative experiment are shown. (Right) Relative band intensities of ubiquitin at 1.5 mM VPA were normalized to GAPDH. All bars show mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
Reactive oxygen species (ROS) are induced by several types of cellular stress and have been implicated as mediators of both autophagy and apoptosis.33 To investigate whether the observed effects of HDACis in AML cells were mediated via ROS, Kasumi-1 cells were pretreated with the ROS scavenger NAC before addition of VPA. Cell death induced by VPA in combination with Baf or CQ was indeed reversed by NAC treatment (Figure 4D), indicating a dependency on ROS for the mediation of cell death by VPA/autophagy inhibitor cotreatment. Elevation of cellular ROS is often associated with an accumulation of ubiquitinated proteins.34 In line with this, cotreatment with VPA and autolysosomal inhibitors led to a significant accumulation of ubiquitinated proteins in Kasumi-1 cells (Figure 4E). Similar results were obtained by vorinostat treatment (supplemental Figure 6). Interestingly, also treatment with HDACis alone enhanced the levels of ubiquitinated proteins (Figure 4E; supplemental Figure 6), and this was not caused by inhibition of proteasomal activity (data not shown). In summary, our data indicate that VPA and vorinostat trigger cell stress leading to accumulation of ubiquitinated proteins, which subsequently become targeted for degradation by autophagy. Thus, HDACi-induced autophagy appears to counteract cell death by preventing a massive buildup of ubiquitinated proteins.
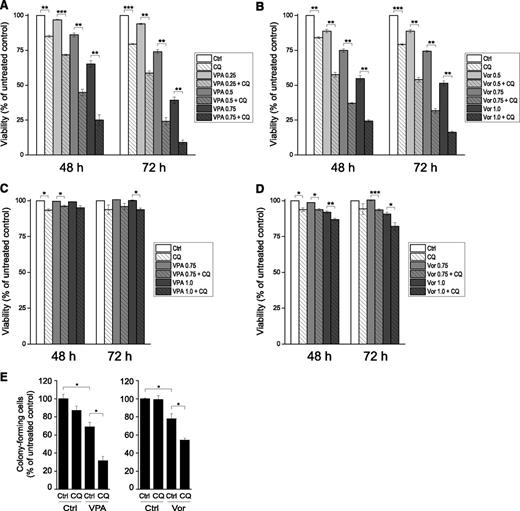
CQ potentiates the toxic effect of VPA and vorinostat during long-term treatment
We next examined whether CQ would potentiate the toxic effect of VPA during prolonged exposure. Moreover, to more closely mimic the clinical conditions, the VPA intravenous formulation (Orfiril) was used in the following experiments, and concentrations of VPA that represent the therapeutic VPA serum concentrations obtained during controlled long-term treatment of epilepsy35 (in the range of 0.25-1 mM) were chosen. Whereas the reduction in cell viability was modest when CQ or low concentrations of VPA (up to 0.5 mM) were administered separately, cotreatment with CQ significantly potentiated VPA-induced toxicity at all concentrations tested (Figure 5A; supplemental Figure 7A). Very similar results were obtained with the combination of vorinostat and CQ (Figure 5B), and supra-additive effects of the HDACis and CQ were also observed in SKNO-1 cells (supplemental Figure 7B-C). In contrast, HL60, an AML1-ETO–negative cell line, was considerably less sensitive to these drug combinations (Figure 5C-D). This indicates a persistent supra-additive effect on cell death in t(8;21)-positive cell lines treated with HDACis and CQ.
CQ potentiates the effect of VPA and vorinostat in long-term experiments and colony-formation assay. (A-B) Kasumi-1 cells were treated with the indicated concentrations of (A) VPA (mM) or (B) vorinostat (Vor, μM) with or without CQ for the indicated times, and cell viability was determined by FACS analysis of PI-stained cells. (C-D) HL60 cells were treated as in A and B, and cell viability was determined by FACS analysis of PI-stained cells. (E) Kasumi-1 cells were treated with VPA (0.75 mM) or vorinostat (0.5 μM) in the absence or presence of CQ for 16 hours, 800 cells were seeded in Methocult medium in the absence of drugs, and colonies were scored 8 days later. All bars represent mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
CQ potentiates the effect of VPA and vorinostat in long-term experiments and colony-formation assay. (A-B) Kasumi-1 cells were treated with the indicated concentrations of (A) VPA (mM) or (B) vorinostat (Vor, μM) with or without CQ for the indicated times, and cell viability was determined by FACS analysis of PI-stained cells. (C-D) HL60 cells were treated as in A and B, and cell viability was determined by FACS analysis of PI-stained cells. (E) Kasumi-1 cells were treated with VPA (0.75 mM) or vorinostat (0.5 μM) in the absence or presence of CQ for 16 hours, 800 cells were seeded in Methocult medium in the absence of drugs, and colonies were scored 8 days later. All bars represent mean values ± SEM quantified from ≥3 independent experiments. *P < .05; **P < .01; ***P < .001.
To investigate whether HDACis and CQ affected the clonogenic ability of Kasumi-1 cells, a colony formation assay was performed. After 16 hours of treatment, the cells were seeded out in semisolid medium in the absence of drugs, and colonies were scored 8 days later. As shown in Figure 5E, CQ potentiated the ability of both VPA and vorinostat to inhibit colony formation, the effect being most pronounced with VPA.
Together, these data demonstrate that HDACi/CQ cotreatment has a long-term detrimental effect on both the viability and the clonogenic ability of t(8;21)-positive cells.
VPA induces autophagy and potentiates the toxic effect of CQ in primary t(8;21) AML cells
Given the potential clinical implications of our findings, we next investigated whether the effects observed in the t(8;21)-positive cell lines were reflected also in primary AML cells obtained from t(8;21)-positive patients. In line with our findings in the t(8;21) cell lines, VPA treatment significantly increased the degradation of long-lived proteins in the patient samples (Figure 6A) (mean value: 107.2% of untreated control ± 2.08, P < .05), suggesting that VPA induces autophagy also in primary AML cells. Although VPA showed no toxicity by itself, treatment with CQ alone was more toxic to the primary cells than to the AML cell lines (Figure 6B). Most importantly, however, cotreatment with VPA and CQ reduced cell viability to a level significantly lower than CQ treatment alone (Figure 6B). In contrast, the same concentrations of VPA and CQ that were observed to be toxic to AML cells did not show the same toxicity in peripheral blood mononuclear cells from a healthy individual (supplemental Figure 8). AML cells negative for t(8;21) were, like the t(8;21)-negative cell line HL60, less sensitive than t(8;21)-positive cells to treatment with CQ and also less sensitive to cotreatment with VPA and CQ (supplemental Figure 9), although a tendency of VPA inducing autophagy (supplemental Figure 9A) and a tendency of additive toxic effects by combination of VPA and CQ were observed (supplemental Figure 9B). In conclusion, these data indicate that VPA induces prosurvival autophagy in primary AML cells, further strengthening the potential clinical relevance of autophagy as a drug target in AML. Moreover, compared with t(8;21)-negative AML cells and normal peripheral blood mononuclear cells, CQ and the combination of VPA and CQ appears to be particularly toxic to t(8;21)-positive AML.
VPA induces autophagy and potentiates the effect of CQ in primary t(8;21) AML cells. (A) Primary t(8;21) AML samples were treated or not with VPA (1 mM) for 16 hours, and degradation of long-lived proteins was measured. (B) The AML samples were treated with VPA (1 mM), CQ (12.5 µM), or both for 48 hours. Cell viability was determined by FACS analysis of PI-stained cells and presented as (left) raw data or (right) normalized to the untreated control. **P < .01.
VPA induces autophagy and potentiates the effect of CQ in primary t(8;21) AML cells. (A) Primary t(8;21) AML samples were treated or not with VPA (1 mM) for 16 hours, and degradation of long-lived proteins was measured. (B) The AML samples were treated with VPA (1 mM), CQ (12.5 µM), or both for 48 hours. Cell viability was determined by FACS analysis of PI-stained cells and presented as (left) raw data or (right) normalized to the untreated control. **P < .01.
Discussion
In this study, we demonstrate that the apoptosis-inducing HDACis VPA and vorinostat induce autophagy in t(8;21) AML cells. In addition our data set indicates that the induction of autophagy precedes apoptosis induction and acts to limit the latter, as inhibition of autophagy enhanced caspase activity and apoptotic cell death in VPA- and vorinostat-treated cells. This potentiating effect on HDAC inhibitor-induced cell death was observed both with lysosomal inhibitors and by siRNA-mediated knockdown of core autophagic components, strongly indicating that the effect was specifically caused by inhibition of the prosurvival function of autophagy in drug-treated AML cells.
Interestingly, our data and those reported in previous publications indicate a variable role of autophagy in the 2 most frequent subtypes of fusion oncoprotein-associated AMLs. In PML-RARA–expressing cells, drug-induced degradation of the fusion oncoprotein is partly dependent on autophagy,7,8 and thus autophagy inducers may be beneficial in therapeutic treatment. In t(8;21)-positive AML, however, we show that the AML1-ETO fusion oncoprotein is not degraded by autophagy. Combined with our finding that autophagy has a prosurvival role in these cells, we suggest that inhibition of autophagy can be used as an efficient treatment strategy in this AML subtype. Together, these studies point to the importance of elucidating the role of autophagy in different AML subtypes when aiming to optimize cancer treatment via modulation of autophagy.
We found that both VPA and vorinostat enhanced the levels of ubiquitinated proteins, which appeared to be substrates for autophagy, as they further accumulated by autophagy inhibition. The buildup of ubiquitinated proteins correlated with increased cell death, indicating that the increase in apoptosis observed by combined treatment with HDAC and autophagy inhibitors was due to toxic accumulation of ubiquitinated proteins. The increased cell death induced by VPA/autophagy inhibitor cotreatment was reversed by the ROS scavenger NAC, indicating an involvement of ROS. Interestingly, ROS and accumulation of ubiquitinated proteins have similarly been implicated in cell death induced by vorinostat and CQ in colon cancer and CML cells,21,23 indicating that this phenomenon is not confined to the AML cells used in the current study.
HDACis have been reported to induce autophagy in a number of cell types21-27 ; however, the exact mechanism(s) involved are yet to be defined. Because HDACs have both histone and nonhistone targets, the effects of HDACis might be caused by chromatin remodeling and changes in gene expression and/or by altered functions of nonhistone proteins due to their increased acetylation.36 Interestingly, we found that both VPA and vorinostat enhanced the transcript levels of LC3B in Kasumi-1 cells. This has also been observed in glioblastoma cells.27 Moreover, in patients with chronic obstructive pulmonary disease, inhibition of HDAC activity was shown to increase the binding of early growth response-1 and E2F transcription factors to the LC3B promoter region, activating LC3B expression in patient lung tissues.37 Thus, induction of LC3B transcription may be a common denominator explaining the autophagy-induction by HDACis. However, because enhanced transcription of LC3B is not necessarily sufficient to enhance autophagic activity,38 it is likely that HDACis must also bring about other molecular changes to activate autophagy. Interestingly, HDACi-induced hyperacetylation of nonhistone proteins, such as Ku, signal transducer and activator of transcription 3, heat shock protein (Hsp)90, p53, and several transcription factors, have been shown to affect cell proliferation, cell survival, and apoptosis in various cell types.36,39 Hsp90 is deactivated by hyperacetylation, leading to degradation of its client proteins. The Hsp90 client proteins Akt and c-Kit, involved in autophagy regulation and prosurvival signaling, respectively, might be relevant in t(8;21) AML because ∼50% of AML patients show constitutive activation of the phosphatidylinositol 3-kinase/Akt pathway,40 and activating c-Kit mutations mediating cellular survival are predominantly found in t(8;21) and inv(16) AML subtypes.41,42 The regulation of autophagy and survival may be tightly linked, as loss of survival signals, which would mimic growth factor starvation, is known to induce autophagy.43 It will be interesting in future studies to elucidate whether nonhistone targets of HDACs influence the viability of t(8;21) AML cells during HDACi treatment.
AML subtypes expressing AML1-ETO, PML-RARA, or PLZF-RARA have been reported to be particularly responsive to HDACi treatment.19,44 A common oncogenic feature of these fusion proteins is assembly of HDAC-containing repressor complexes that block transcription of prodifferentiation genes,45 and the sensitivity toward HDACis could be explained by a release of the transcriptional block with subsequent restoration of differentiation and loss of apoptosis evation.15 Moreover, HDACis are known to induce DNA damage, and the abovementioned fusion oncoproteins were reported to mediate downregulation of DNA repair machinery components, making these AML subtypes particularly sensitive to further HDACi-induced DNA damage.44 Thus, it seems probable that AML subtypes that express fusion oncoproteins with similar abilities as AML1-ETO, eg, inv(16)-positive AML expressing the fusion oncoprotein core-binding factor β–smooth muscle myosin heavy chain, will also respond to HDAC inhibitor treatment.45 Our results indicate that HDACis induce prosurvival autophagy in t(8;21)-positive AML and that HDACis therefore are more efficient death inducers in combination with autophagy inhibitors like CQ. Furthermore, our initial studies suggest that the same may, although to a lesser extent, also be the case for t(8;21)-negative AML. To which degree a combination strategy with autophagy inhibitors may increase the proapoptotic effect of HDACis in various subtypes of AML cells with or without HDAC-associated fusion proteins will be of great interest and the topic of future studies. Beyond this, it will also be interesting to learn to which degree the HDACi/CQ combination strategy can target AML stem cells. Vorinostat was recently shown to reduce the self-renewal properties of AML stem cells,46 and it remains to be seen whether this effect is potentiated by autophagy inhibition.
In conclusion, we showed that inhibition of autophagy can significantly potentiate the apoptotic effect of HDACis in t(8;21) AML1-ETO–positive AML cells. Thus, a combinatorial treatment with autophagy inhibitors and AML1-ETO–targeting drugs, such as VPA or vorinostat, represents an attractive novel therapeutic option that warrants further investigation.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Øystein Bruserud (Haukeland University Hospital, Bergen) for an AML patient sample.
M.L.T., S.-O.B., and A.S. were supported by funding from the Research Council of Norway and the Norwegian Cancer Society. N.E. was supported by funding from the South-Eastern Norway Regional Health Authority, the University of Oslo, and the Research Council of Norway through the Centre for Molecular Medicine Norway. P.H. was supported by the Danish Medical Research Council, the Danish Cancer Society, and the Karen Elise Jensen Foundation.
Authorship
Contribution: M.L.T., N.E., S.-O.B., and A.S. designed the experiments; M.L.T., N.E., and S.-O.B. performed the research and data analysis; P.H. provided patient material; M.L.T., N.E., and A.S. prepared the manuscript; and M.L.T., N.E., S.-O.B., P.H., and A.S. added to and approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Anne Simonsen, Department of Biochemistry, Institute of Basic Medical Sciences, University of Oslo, Pb. 1112 Blindern, 0317 Oslo, Norway; e-mail: anne.simonsen@medisin.uio.no.