Key Points
The risk for venous thromboembolism in relatives with factor V Leiden or prothrombin G20210A differs according to the probands’ selection.
Relatives belonging to families with heterozygous probands with venous thromboembolism have the highest risk for venous thromboembolism.
Abstract
In family studies, the risk for venous thromboembolism (VTE) in relatives with factor V Leiden (FVL) or G20210A prothrombin (PT20210A) gene polymorphisms may differ according to genotype and clinical presentation of the proband. To address this hypothesis, a retrospective cohort family study was carried out on 192 kindreds with at least one member with homozygous FVL or PT20210A, for a total of 886 relatives. The proband of the family was heterozygous in 68 and homozygous or with both polymorphisms in 124 kindreds. Twenty-three probands were asymptomatic, 11 had had arterial thrombosis, 7 obstetrical complications, and 151 venous thrombosis (122 VTE and 29 superficial vein thrombosis). The incidence of VTE (per 1000 patient-years) in relatives was higher when the proband had heterozygous rather than homozygous polymorphism (1.25 [95% confidence interval (CI), 0.73-1.91] vs 0.44 [0.19-0.78]) and when the proband had had VTE instead of other or no clinical manifestations (0.95 [0.57-1.42] vs 0.50 [0.19-0.96]). Compared with relatives belonging to kindreds with homozygous probands without VTE, the adjusted hazard ratio of VTE for relatives selected from kindreds with heterozygous probands with VTE was 4.14 (95% CI, 1.17-14.71). The genotype and clinical presentation of the proband influence the risk for VTE in relatives with FVL or PT20210A.
Introduction
The 1691 guanine-to-adenine substitution in coagulation factor V gene (factor V rs6025 or factor V Leiden [FVL]) and the 20210 guanine-to-adenine substitution in the 3′-untranslated region of the prothrombin gene (PT20210A) are 2 common gain-of-function polymorphisms (with a prevalence about 3% and 4% in the Italian population, respectively) and are well-established risk factors for venous thromboembolism (VTE).1-4 Carriers of FVL or PT20210A show different VTE risk throughout life. Some of them suffer from VTE early in life, others develop VTE when they are elderly (and perhaps only under triggering conditions) or remain asymptomatic.5,6 This variation may have several explanations. The cosegregation of FVL or PT20210A with antithrombin, protein C, or protein S deficiency,7-9 or even with low borderline levels of these naturally occurring anticoagulant proteins10 ; the frequency of triggering risk factors (such as surgery, immobilization, pregnancy/puerperium, or oral contraceptive intake); and the coinheritance of other unknown genetic risk factors can modulate the thrombotic risk.11,12 In addition, the risk for VTE in family members with FVL or PT20210A might differ according either to genotype (heterozygous or homozygous) or clinical presentation (previous VTE, superficial vein thrombosis, arterial thrombosis, obstetrical complication, or no thrombosis) of the proband, who is the first family member who has been investigated. The latter hypothesis has been recently confirmed by a family study that showed a higher risk for VTE in relatives of probands with VTE than other clinical presentations.13
We hypothesized that the risk for VTE in relatives heterozygous or homozygous for FVL or PT20210A can be influenced by either the genotype or the clinical presentation of the proband. Although a lower risk is associated with heterozygosity than with homozygosity,14 family members of probands with heterozygous polymorphisms and VTE are expected to share the highest risk for VTE because their probands had developed thrombosis. We carried out a retrospective cohort family study of a large number of kindreds with at least one member with homozygous FVL or PT20210A. This selection criterion allowed us also to analyze a consistent number of relatives with homozygous polymorphisms and to assess the effect of family selection on their risk for VTE, according both to genotype (homozygous vs heterozygous) and clinical presentation (VTE vs other or no manifestations) of the proband.
Methods
Study population
First- and second-degree relatives of probands with FVL or PT20210A referred from 1991 to 2010 for a thrombophilia work-up to 5 Italian Thrombosis Centers (Milan, Rome, Bologna, Padua, and Vicenza) were included in the study if at least one member of the kindred had homozygous FVL or PT20210A. All probands were asked to bring to the centers as many family members as possible for FVL and PT20210A genotyping. Before knowing the results of the genotyping, clinical and demographic data of probands and relatives were collected by an interview, during which information on previous episodes of thrombosis also was collected via a validated questionnaire.15,16 Only objectively documented episodes of VTE (ie, deep vein thrombosis of lower or upper limbs and/or pulmonary embolism, or thrombosis of the cerebral or splanchnic veins) occurred before the referral to the thrombosis centers was recorded. Diagnosis of deep vein thrombosis of the lower or upper limbs was made by compression ultrasound or venography, and that of pulmonary embolism was made by ventilation/perfusion lung scan, computed tomography scan, or pulmonary angiography. Cerebral or splanchnic vein thromboses were diagnosed by a cerebral/abdominal angio-computed tomography scan or magnetic resonance. In the case of superficial vein thrombosis, the diagnosis was also accepted if it was made only on clinical grounds, but this type of venous thrombosis was only described and was not included in the analysis of thrombotic risk. Episodes of venous thrombosis were considered unprovoked when they occurred in the absence of transient risk factors (surgery, fractures, trauma, complete immobilization in bed for at least 7 days in the month preceding the event, pregnancy/puerperium, and oral contraceptive intake).
In all relatives, blood was collected into vacuum tubes containing 3.2% sodium citrate. Genotyping for FVL and PT20210A was carried out as previously described.1,2 The study was approved by the Institutional Review Board of the 5 hospitals, and all family members gave written informed consent to participate in the study in accordance with the Declaration of Helsinki.
Statistical analysis
Probands were excluded from the analyses to avoid selection bias. Continuous variables were described as median and interquartile range (IQR), and categorical variables were described as count and percentage. For each relative, the follow-up started at the date of birth and ended at either the date of the first VTE event or the date of the visit to the centers (administrative censoring). According to the genotype and clinical presentation of probands, relatives were divided into 4 groups; that is, belonging to kindreds with a homozygous proband without VTE (reference group), a homozygous proband with at least a single episode of VTE, a heterozygous proband without VTE, or a heterozygous proband with at least a single episode of VTE. Relatives belonging to kindreds with probands carrying both polymorphisms were included in the group of relatives selected from homozygous probands. For each group, the annual incidence of VTE was calculated by dividing the number of events by the sum of patient-years of observation, and 95% confidence intervals (CIs) were calculated under the Poisson distribution assumption. The cumulative VTE-free survival was calculated using the Kaplan-Meier method. The hazard ratio (and 95% CI) for VTE in each group compared with the reference group was estimated using a multivariable Cox proportional hazard model, which allowed for adjustment for such possible confounders as age, sex, type of genetic defect, and genotype of the relatives. The incidence rates of the 4 groups of relatives were standardized to those of the general population according to age and sex17 through the indirect method. The person-years each individual of the study population contributed to the follow-up were split in the different age categories, separately for men and women, and the expected number of VTE in each category was calculated by multiplying the person-years at risk by the corresponding sex- and age-specific incidence rate of the general population.17 Because in the reference study the first age category was set at 20 to 24 years, and in the study population all VTE events occurred from age 21 years onward, the first age category for standardization was set at 20 to 24 years. The resulting standardized incidence ratio (SIR), together with its 95% CI, is the ratio between observed and expected VTE and represents a measure of the magnitude of the VTE risk in the study population compared with that in the general population of same age and sex (ie, an SIR >1 means that the incidence of VTE in the study population is higher than that expected in a population with the age-year–specific rates of the general population and the person-year distribution observed in the study population). P < .05 was taken as cutoff for statistical significance. All analyses were performed with the statistical software SPSS (release 19.0; IBM SPSS Statistics for Windows).
Results
Eight hundred eighty-six relatives (380 men and 506 women; median age, 38 years [IQR, 25-54 years]; 551 first-degree and 335 second-degree) from 192 kindreds were included in the study. Of these participants, 378 were heterozygous for FVL, 129 were heterozygous for PT20210A, 101 were homozygous for FVL, 36 were homozygous for PT20210A, 38 had combined polymorphisms, and 204 were wild-type. The median number of relatives per family was 3 (IQR, 2-6 relatives; range, 1-27 relatives). The proband of the family was heterozygous for FVL or PT20210A in 68 kindreds (50 FVL and 18 PT20210A) and homozygous or with both polymorphisms in 124 kindreds (76 FVL, 35 PT20210A, and 13 with both polymorphisms). Twenty-three probands were asymptomatic (genetic defect discovered by chance), 11 had had arterial thrombosis, 7 had had obstetrical complications, and 151 had had venous thrombosis (122 VTE and 29 superficial vein thrombosis). The characteristics of relatives according to their type of polymorphism and to the proband’s genotype and clinical presentation are shown in Table 1.
Characteristics of the study population of relatives according to the genotype and clinical presentation of the proband
| Proband characteristics (phenotype and genotype) . | Relatives . | |||||
|---|---|---|---|---|---|---|
| Wild-type . | Heterozygous PT20210A . | Heterozygous FVL . | Homozygous PT20210A . | Homozygous FVL . | Combined polymorphisms* . | |
| Asymptomatic, obstetrical complications, arterial thrombosis | ||||||
| Homozygous (24 kindreds) | ||||||
| n (M/F) | 23 (13/10) | 38 (16/22) | 32 (15/17) | 2 (0/2) | 6 (4/2) | 9 (2/7) |
| Age at visit, y† | 38 (26-53) | 51 (26-60) | 44 (22-62) | 49 (29-62) | 33 (27-39) | 31 (14-53) |
| VTE, n (%) | 0 | 1 (3) | 0 | 1 (50) | 1 (17) | 0 |
| Age at VTE, y† | –– | 52 (––) | –– | 29 (––) | 34 (––) | –– |
| Heterozygous (17 kindreds) | ||||||
| n (M/F) | 31 (7/24) | 10 (6/4) | 27 (18/9) | 3 (0/3) | 18 (7/11) | 0 |
| Age at visit, y† | 41 (32-57) | 55 (29-69) | 46 (31-61) | 45 (36-56) | 30 (18-50) | –– |
| VTE, n (%) | 0 | 0 | 1 (4) | 0 | 2 (11) | –– |
| Age at VTE, y† | –– | –– | 69 (––) | –– | 51 (48-55) | –– |
| Superficial vein thrombosis | ||||||
| Homozygous (24 kindreds) | ||||||
| n (M/F) | 22 (9/13) | 3 (1/2) | 74 (34/40) | 2 (2/0) | 14 (5/9) | 1 (1/0) |
| Age at visit, y | 29 (14-56) | 20 (16-37) | 38 (25-56) | 29 (13-45) | 35 (21-47) | 3 (––) |
| VTE, n (%) | 0 | 0 | 0 | 0 | 0 | 0 |
| Age at VTE, y† | –– | –– | –– | –– | –– | –– |
| Heterozygous (5 kindreds) | ||||||
| n (M/F) | 14 (4/10) | 0 | 10 (2/8) | 0 | 6 (3/3) | 3 (1/2) |
| Age at visit, y† | 50 (37-64) | –– | 47 (25-65) | –– | 32 (24-59) | 25 (11-48) |
| VTE, n (%) | 0 | –– | 0 | –– | 0 | 1 (33) |
| Age at VTE, y† | –– | –– | –– | –– | –– | 40 (––) |
| VTE | ||||||
| Homozygous (76 kindreds) | ||||||
| n (M/F) | 52 (17/35) | 47 (17/30) | 148 (57/91) | 12 (5/7) | 23 (16/7) | 23 (13/10) |
| Age at visit, y† | 34 (21-47) | 39 (25-53) | 39 (24-54) | 32 (24-42) | 38 (27-50) | 43 (29-56) |
| VTE, n (%) | 0 | 0 | 3 (2) | 0 | 2 (9) | 1 (5) |
| Age at VTE, y† | –– | –– | 47 (24-62) | –– | 26 (24-27) | 61 (––) |
| Heterozygous (46 kindreds) | ||||||
| n (M/F) | 62 (31/31) | 31 (15/16) | 87 (36/51) | 17 (9/8) | 34 (13/21) | 2 (1/1) |
| Age at visit, y† | 38 (30-48) | 39 (26-55) | 43 (26-61) | 32 (21-43) | 36 (25-47) | 67 (59-75) |
| VTE, n (%) | 0 | 2 (6) | 6 (7) | 0 | 6 (18) | 0 |
| Age at VTE, y† | –– | 44 (35-53) | 61 (27-64) | –– | 33 (24-46) | –– |
| Proband characteristics (phenotype and genotype) . | Relatives . | |||||
|---|---|---|---|---|---|---|
| Wild-type . | Heterozygous PT20210A . | Heterozygous FVL . | Homozygous PT20210A . | Homozygous FVL . | Combined polymorphisms* . | |
| Asymptomatic, obstetrical complications, arterial thrombosis | ||||||
| Homozygous (24 kindreds) | ||||||
| n (M/F) | 23 (13/10) | 38 (16/22) | 32 (15/17) | 2 (0/2) | 6 (4/2) | 9 (2/7) |
| Age at visit, y† | 38 (26-53) | 51 (26-60) | 44 (22-62) | 49 (29-62) | 33 (27-39) | 31 (14-53) |
| VTE, n (%) | 0 | 1 (3) | 0 | 1 (50) | 1 (17) | 0 |
| Age at VTE, y† | –– | 52 (––) | –– | 29 (––) | 34 (––) | –– |
| Heterozygous (17 kindreds) | ||||||
| n (M/F) | 31 (7/24) | 10 (6/4) | 27 (18/9) | 3 (0/3) | 18 (7/11) | 0 |
| Age at visit, y† | 41 (32-57) | 55 (29-69) | 46 (31-61) | 45 (36-56) | 30 (18-50) | –– |
| VTE, n (%) | 0 | 0 | 1 (4) | 0 | 2 (11) | –– |
| Age at VTE, y† | –– | –– | 69 (––) | –– | 51 (48-55) | –– |
| Superficial vein thrombosis | ||||||
| Homozygous (24 kindreds) | ||||||
| n (M/F) | 22 (9/13) | 3 (1/2) | 74 (34/40) | 2 (2/0) | 14 (5/9) | 1 (1/0) |
| Age at visit, y | 29 (14-56) | 20 (16-37) | 38 (25-56) | 29 (13-45) | 35 (21-47) | 3 (––) |
| VTE, n (%) | 0 | 0 | 0 | 0 | 0 | 0 |
| Age at VTE, y† | –– | –– | –– | –– | –– | –– |
| Heterozygous (5 kindreds) | ||||||
| n (M/F) | 14 (4/10) | 0 | 10 (2/8) | 0 | 6 (3/3) | 3 (1/2) |
| Age at visit, y† | 50 (37-64) | –– | 47 (25-65) | –– | 32 (24-59) | 25 (11-48) |
| VTE, n (%) | 0 | –– | 0 | –– | 0 | 1 (33) |
| Age at VTE, y† | –– | –– | –– | –– | –– | 40 (––) |
| VTE | ||||||
| Homozygous (76 kindreds) | ||||||
| n (M/F) | 52 (17/35) | 47 (17/30) | 148 (57/91) | 12 (5/7) | 23 (16/7) | 23 (13/10) |
| Age at visit, y† | 34 (21-47) | 39 (25-53) | 39 (24-54) | 32 (24-42) | 38 (27-50) | 43 (29-56) |
| VTE, n (%) | 0 | 0 | 3 (2) | 0 | 2 (9) | 1 (5) |
| Age at VTE, y† | –– | –– | 47 (24-62) | –– | 26 (24-27) | 61 (––) |
| Heterozygous (46 kindreds) | ||||||
| n (M/F) | 62 (31/31) | 31 (15/16) | 87 (36/51) | 17 (9/8) | 34 (13/21) | 2 (1/1) |
| Age at visit, y† | 38 (30-48) | 39 (26-55) | 43 (26-61) | 32 (21-43) | 36 (25-47) | 67 (59-75) |
| VTE, n (%) | 0 | 2 (6) | 6 (7) | 0 | 6 (18) | 0 |
| Age at VTE, y† | –– | 44 (35-53) | 61 (27-64) | –– | 33 (24-46) | –– |
Thirty-two compound heterozygous, 5 homozygous for FVL and heterozygous for PT20210A, 1 heterozygous for FVL and homozygous for PT20210A.
Age is expressed as median and interquartile range (or minimum and maximum values in case of ≤3 observations).
Table 2 shows the type of symptom in relatives according to the genotype and the clinical presentation of the probands. Of the 116 relatives (89 of whom with FVL) belonging to kindreds with proband homozygous for FVL or PT20210A and superficial vein thrombosis only, 11 (9%; 7 heterozygous FVL, 2 homozygous FVL, and 2 wild-type) had superficial vein thrombosis, and none of them had VTE. Moreover, of the 33 relatives (19 with FVL) belonging to 5 kindreds whose proband was heterozygous for FVL or PT20210A and had had only superficial vein thrombosis, only 1 (3%) suffered from VTE (a 48-year-old man with homozygous FVL and heterozygous PT20210A who had an unprovoked VTE at the age of 40 years), whereas the other 9 symptomatic relatives (5 heterozygous FVL, 2 homozygous FVL, and 2 wild-type) had superficial vein thrombosis.
Type of symptom in the study population of relatives according to the genotype and clinical presentation of the proband
| Proband characteristics (phenotype and genotype) . | Relatives, n . | Symptomatic relatives, n (%) . | Type of symptom, n (%)* . | |||
|---|---|---|---|---|---|---|
| VTE . | Superficial vein thrombosis . | Arterial thrombosis . | Obstetric complications . | |||
| Asymptomatic, obstetric complications, arterial thrombosis | ||||||
| Homozygous (24 kindreds) | 110 | 11 (10) | 3 (27) | 5 (45) | 2 (18)† | 1 (9) |
| Heterozygous (17 kindreds) | 89 | 9 (10) | 3 (33) | 2 (22) | 4 (44) | 0 (—) |
| Superficial vein thrombosis | ||||||
| Homozygous (24 kindreds) | 116 | 13 (11) | 0 (—) | 11 (85)‡ | 2 (15) | 1 (8) |
| Heterozygous (5 kindreds) | 33 | 10 (30) | 1 (10) | 9 (90) | 0 (—) | 0 (—) |
| VTE | ||||||
| Homozygous (76 kindreds) | 305 | 27 (9) | 6 (22)¶ | 15 (56) | 6 (22) | 1 (4) |
| Heterozygous (46 kindreds) | 233 | 42 (18) | 14 (33)§ | 22 (52) | 6 (14) | 2 (5)‖ |
| Proband characteristics (phenotype and genotype) . | Relatives, n . | Symptomatic relatives, n (%) . | Type of symptom, n (%)* . | |||
|---|---|---|---|---|---|---|
| VTE . | Superficial vein thrombosis . | Arterial thrombosis . | Obstetric complications . | |||
| Asymptomatic, obstetric complications, arterial thrombosis | ||||||
| Homozygous (24 kindreds) | 110 | 11 (10) | 3 (27) | 5 (45) | 2 (18)† | 1 (9) |
| Heterozygous (17 kindreds) | 89 | 9 (10) | 3 (33) | 2 (22) | 4 (44) | 0 (—) |
| Superficial vein thrombosis | ||||||
| Homozygous (24 kindreds) | 116 | 13 (11) | 0 (—) | 11 (85)‡ | 2 (15) | 1 (8) |
| Heterozygous (5 kindreds) | 33 | 10 (30) | 1 (10) | 9 (90) | 0 (—) | 0 (—) |
| VTE | ||||||
| Homozygous (76 kindreds) | 305 | 27 (9) | 6 (22)¶ | 15 (56) | 6 (22) | 1 (4) |
| Heterozygous (46 kindreds) | 233 | 42 (18) | 14 (33)§ | 22 (52) | 6 (14) | 2 (5)‖ |
Percentage calculated on the number of symptomatic relatives.
One retinal thrombosis.
One relative had superficial vein thrombosis 12 years after myocardial infarction.
One relative had VTE soon after an obstetrical complication.
One relative had VTE 8 years after SVT
One relative had an obstetrical complication 2 years after VTE
A total of 27 episodes of VTE (21 isolated lower limbs deep vein thromboses, 4 lower limbs deep vein thromboses with pulmonary embolism, 1 upper limb deep vein thrombosis, and 1 portal vein thrombosis) during the 34 966 patient-years of follow-up were recorded, for an overall incidence rate of 0.77 per 1000 patient-years (95% CI, 0.48-1.06). The median age at VTE was 40 years (IQR, 28-61 years). Twelve episodes (44%) of VTE were unprovoked and 15 (56%) were secondary to transient risk factors. Ten relatives with heterozygous FVL (3%), 3 with heterozygous PT20210A (2%), 11 with homozygous FVL (11%), 1 with homozygous PT20210A (3%), 2 with both polymorphisms (5%), and none with wild-type genotype developed VTE. Nearly 50% of the VTE episodes occurred in relatives with homozygous or combined polymorphisms, and at a younger age (median, 35 years; IQR, 27-50 years) than VTE episodes in heterozygous carriers (median, 53 years; IQR, 32-63 years) (Table 1). Most of the transient risk factors reported in the 15 of the 27 episodes of VTE were pregnancy/puerperium and oral contraceptive intake. The type and prevalence of transient risk factors for VTE according to type of polymorphism are listed in Table 3.
Distribution of risk factors in the 27 relatives with VTE
| . | Wild-type (n = 0) . | Homozygous PT20210 (n = 3) . | Heterozygous FVL (n = 10) . | Homozygous PT20210 (n = 1) . | Homozygous FVL (n = 11) . | Combined polymorphisms (n = 2) . |
|---|---|---|---|---|---|---|
| No risk factor, n (%) | –– | 1 (33) | 5 (50) | 1 (100) | 3 (27) | 2 (100) |
| M/F | –– | 0/1 | 2/3 | 0/1 | 2/1 | 2/0 |
| Surgery, trauma or immobilization, n (%) | –– | 1 (33) | 2 (20) | –– | 1 (9) | –– |
| M/F | –– | 1/0 | 1/1 | –– | 0/1 | –– |
| Pregnancy/puerperium, n (%)* | –– | 1 (50) | –– | –– | 2 (25) | –– |
| Oral contraceptive use, n (%)* | –– | –– | 3 (43) | –– | 5 (63) | –– |
| . | Wild-type (n = 0) . | Homozygous PT20210 (n = 3) . | Heterozygous FVL (n = 10) . | Homozygous PT20210 (n = 1) . | Homozygous FVL (n = 11) . | Combined polymorphisms (n = 2) . |
|---|---|---|---|---|---|---|
| No risk factor, n (%) | –– | 1 (33) | 5 (50) | 1 (100) | 3 (27) | 2 (100) |
| M/F | –– | 0/1 | 2/3 | 0/1 | 2/1 | 2/0 |
| Surgery, trauma or immobilization, n (%) | –– | 1 (33) | 2 (20) | –– | 1 (9) | –– |
| M/F | –– | 1/0 | 1/1 | –– | 0/1 | –– |
| Pregnancy/puerperium, n (%)* | –– | 1 (50) | –– | –– | 2 (25) | –– |
| Oral contraceptive use, n (%)* | –– | –– | 3 (43) | –– | 5 (63) | –– |
Percentage calculated on the number of women.
The incidence of VTE (per 1000 patient-years) in relatives was higher when the proband had heterozygous vs homozygous polymorphism (1.25 [95% CI, 0.73-1.91; n = 355 with 18 VTE] vs 0.44 [95 CI, 0.19-0.78; n = 531 with 9 VTE]; relative risk, 2.84 [95% CI, 1.28-6.32]) and when the proband had VTE instead of other clinical presentations (0.95 [95% CI, 0.57-1.42; n = 537 with 20 VTE] vs 0.50 [95% CI, 0.19-0.96; n = 349 with 7 VTE]; relative risk, 1.90 [95% CI, 0.80-4.48]). Limiting the analysis to the largest group of heterozygous FVL relatives, these figures were 1.30 (95% CI, 0.50-2.48) vs 0.30 (95% CI, 0.05-0.73; relative risk, 4.33 [95% CI, 1.12-16.75]) and 0.94 (95% CI, 0.42-1.67) vs 0.17 (95% CI, 0-0.67; relative risk, 5.53 [95% CI, 0.70-43.64]), respectively.
The incidence and hazard ratios of VTE in the 4 groups of relatives formed according to the genotype and the clinical presentation of the proband are shown in Table 4. Compared with relatives belonging to kindreds with homozygous probands without VTE, the highest risk for VTE was found in those whose proband was heterozygous for FVL or PT20210A and had a VTE event (adjusted hazard ratio, 4.14; 95% CI, 1.17-14.71). Limiting the analysis to FVL relatives only, this figure was 9.85 (95% CI, 1.26-76.93). The incidence of VTE in heterozygous FVL relatives was 1.63 per 1000 patient-years (95% CI, 0.57-3.22) when they were selected from kindreds whose proband was heterozygous for FVL and had had VTE, whereas no VTE event was recorded if they belonged to families with homozygous FVL probands without VTE.
Risk for VTE in relatives according to the genotype and clinical presentation of the proband
| Proband characteristics . | Risk for VTE in relatives . | ||||||
|---|---|---|---|---|---|---|---|
| n (M/F) . | Age, y . | Patient-years . | VTE, n (%) . | VTE Incidence (95% CI)* . | Hazard ratio (95% CI) . | adjHazard ratio (95% CI)† . | |
| Homozygous and VTE – | 226 (102/124) | 36 (23-56) | 8670 | 3 (1) | 0.35 (0.06-0.86) | 1‡ | 1‡ |
| Homozygous and VTE + | 305 (125/180) | 37 (25-53) | 11884 | 6 (2) | 0.50 (0.18-1.00) | 1.53 (0.38-6.12) | 1.32 (0.32-5.35) |
| Heterozygous and VTE – | 122 (48/74) | 41 (30-58) | 5243 | 4 (3) | 0.76 (0.19-1.70) | 2.07 (0.46-9.26) | 2.31 (0.51-10.55) |
| Heterozygous and VTE + | 233 (105/128) | 39 (27-55) | 9169 | 14 (6) | 1.53 (0.82-2.46) | 4.46 (1.28-15.55) | 4.14 (1.17-14.71) |
| Proband characteristics . | Risk for VTE in relatives . | ||||||
|---|---|---|---|---|---|---|---|
| n (M/F) . | Age, y . | Patient-years . | VTE, n (%) . | VTE Incidence (95% CI)* . | Hazard ratio (95% CI) . | adjHazard ratio (95% CI)† . | |
| Homozygous and VTE – | 226 (102/124) | 36 (23-56) | 8670 | 3 (1) | 0.35 (0.06-0.86) | 1‡ | 1‡ |
| Homozygous and VTE + | 305 (125/180) | 37 (25-53) | 11884 | 6 (2) | 0.50 (0.18-1.00) | 1.53 (0.38-6.12) | 1.32 (0.32-5.35) |
| Heterozygous and VTE – | 122 (48/74) | 41 (30-58) | 5243 | 4 (3) | 0.76 (0.19-1.70) | 2.07 (0.46-9.26) | 2.31 (0.51-10.55) |
| Heterozygous and VTE + | 233 (105/128) | 39 (27-55) | 9169 | 14 (6) | 1.53 (0.82-2.46) | 4.46 (1.28-15.55) | 4.14 (1.17-14.71) |
Age is expressed as median and interquartile range.
Per 1000 patient-years.
Hazard ratio adjusted for age, sex, type of defect, and genotype of relatives.
Reference group.
Considering only unprovoked VTE, the incidence rates (per 1000 patient-years) in the 4 groups of relatives were 0.12 (95% CI, 0-0.46; 1 VTE), 0.25 (95% CI, 0.05-0.63; 3 VTE), 0.38 (95% CI, 0.03-1.10; 2 VTE), and 0.66 (95% CI, 0.23-1.30; 6 VTE), respectively. Compared with the reference group, the adjusted hazard ratio for unprovoked VTE in relatives selected from kindreds with heterozygous symptomatic probands was 4.79 (95% CI, 0.55-41.44).
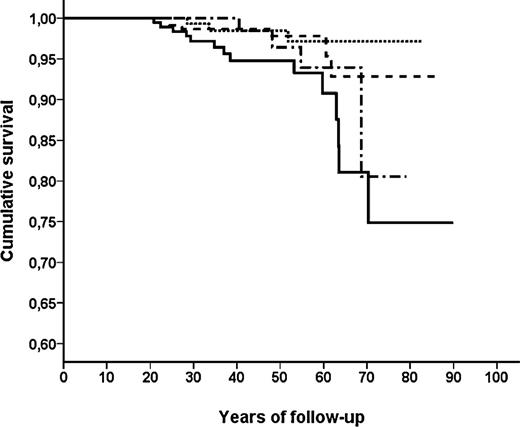
Figure 1 shows the cumulative probability of remaining free from VTE in the 4 groups of relatives. At the age of 65 years, this probability was 0.97 (95% CI, 0.94-1.00) when probands were homozygous without VTE, 0.95 (95% CI, 0.90-1.00) when homozygous with VTE, 0.94 (95% CI, 0.87-1.00) when heterozygous without VTE, and 0.81 (95% CI, 0.69-0.93) when heterozygous with VTE (log-rank test χ2, 9.82; P = .020).
Thrombosis-free survival (Kaplan-Meier estimates) in the 4 subgroups of relatives divided according to the proband’s characteristics. Homozygous without VTE is designated by a dotted line, homozygous with VTE is designated by a dashed line, heterozygous without VTE is designated by a dash-dot line, and heterozygous with VTE is designated by a solid line.
Thrombosis-free survival (Kaplan-Meier estimates) in the 4 subgroups of relatives divided according to the proband’s characteristics. Homozygous without VTE is designated by a dotted line, homozygous with VTE is designated by a dashed line, heterozygous without VTE is designated by a dash-dot line, and heterozygous with VTE is designated by a solid line.
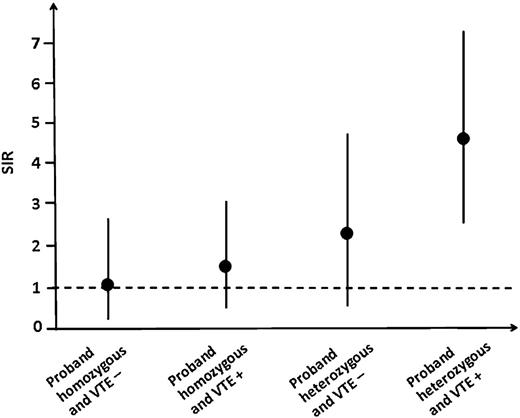
The standardization of incidence rates in the 4 groups of relatives with rates of sex- and age-specific strata of the general population is reported in Table 5, and the corresponding SIRs are shown in Figure 2. When relatives were selected from kindreds with homozygous probands without VTE, the incidence rate of VTE was similar to that of the general population (SIR, 1.05; 95% CI, 0.19-2.61), whereas it was 1.5-fold higher when they were selected from kindreds with homozygous probands with VTE (SIR, 1.55; 95% CI, 0.54-3.07), twofold higher when the probands were heterozygous without VTE (SIR, 2.21; 95% CI, 0.55-4.97), and 4.5-fold higher when the probands were heterozygous with VTE (SIR, 4.61; 95% CI, 2.47-7.40).
Standardization of VTE incidence rates of the study population of relatives according to sex and age, considering the general population as reference
| Proband characteristics and relatives’ sex and age, y . | Incidence rate, general population* . | Study population (patient-years) . | Observed VTE . | Expected VTE . |
|---|---|---|---|---|
| Homozygous and VTE – | ||||
| Men | ||||
| 20-24 | 0.13 | 392 | 0 | 0.05 |
| 25-39 | 0.16 | 809 | 0 | 0.13 |
| 40-54 | 0.65 | 494 | 1 | 0.32 |
| 55-69 | 1.80 | 222 | 0 | 0.40 |
| 70+ | 4.71 | 22 | 0 | 0.10 |
| Women | ||||
| 15-24 | 0.36 | 490 | 0 | 0.18 |
| 25-39 | 0.40 | 1112 | 2 | 0.44 |
| 40-54 | 0.79 | 801 | 0 | 0.63 |
| 55-69 | 1.56 | 295 | 0 | 0.46 |
| 70+ | 4.67 | 33 | 0 | 0.15 |
| Overall | 3 | 2.86 | ||
| Homozygous and VTE + | ||||
| Men | ||||
| 20-24 | 0.13 | 502 | 1 | 0.07 |
| 25-39 | 0.16 | 1069 | 0 | 0.17 |
| 40-54 | 0.65 | 661 | 0 | 0.43 |
| 55-69 | 1.80 | 227 | 2 | 0.41 |
| 70+ | 4.71 | 46 | 0 | 0.22 |
| Women | ||||
| 20-24 | 0.36 | 734 | 1 | 0.26 |
| 25-39 | 0.40 | 1611 | 1 | 0.64 |
| 40-54 | 0.79 | 1014 | 1 | 0.80 |
| 55-69 | 1.56 | 376 | 0 | 0.59 |
| 70+ | 4.67 | 61 | 0 | 0.28 |
| Overall | 6 | 3.87 | ||
| Heterozygous and VTE – | ||||
| Men | ||||
| 20-24 | 0.13 | 221 | 0 | 0.03 |
| 25-39 | 0.16 | 540 | 0 | 0.09 |
| 40-54 | 0.65 | 344 | 1 | 0.22 |
| 55-69 | 1.80 | 167 | 2 | 0.30 |
| 70+ | 4.71 | 25 | 0 | 0.12 |
| Women | ||||
| 20-24 | 0.36 | 310 | 0 | 0.11 |
| 25-39 | 0.40 | 722 | 0 | 0.29 |
| 40-54 | 0.79 | 435 | 1 | 0.34 |
| 55-69 | 1.56 | 171 | 0 | 0.27 |
| 70+ | 4.67 | 9 | 0 | 0.04 |
| Overall | 4 | 1.81 | ||
| Heterozygous and VTE + | ||||
| Men | ||||
| 20-24 | 0.13 | 420 | 0 | 0.05 |
| 25-39 | 0.16 | 930 | 1 | 0.15 |
| 40-54 | 0.65 | 498 | 0 | 0.32 |
| 55-69 | 1.80 | 203 | 1 | 0.37 |
| 70+ | 4.71 | 37 | 0 | 0.17 |
| Women | ||||
| 20-24 | 0.36 | 538 | 2 | 0.19 |
| 25-39 | 0.40 | 1225 | 5 | 0.49 |
| 40-54 | 0.79 | 728 | 1 | 0.58 |
| 55-69 | 1.56 | 286 | 3 | 0.45 |
| 70+ | 4.67 | 57 | 1 | 0.27 |
| Overall | 14 | 3.04 |
| Proband characteristics and relatives’ sex and age, y . | Incidence rate, general population* . | Study population (patient-years) . | Observed VTE . | Expected VTE . |
|---|---|---|---|---|
| Homozygous and VTE – | ||||
| Men | ||||
| 20-24 | 0.13 | 392 | 0 | 0.05 |
| 25-39 | 0.16 | 809 | 0 | 0.13 |
| 40-54 | 0.65 | 494 | 1 | 0.32 |
| 55-69 | 1.80 | 222 | 0 | 0.40 |
| 70+ | 4.71 | 22 | 0 | 0.10 |
| Women | ||||
| 15-24 | 0.36 | 490 | 0 | 0.18 |
| 25-39 | 0.40 | 1112 | 2 | 0.44 |
| 40-54 | 0.79 | 801 | 0 | 0.63 |
| 55-69 | 1.56 | 295 | 0 | 0.46 |
| 70+ | 4.67 | 33 | 0 | 0.15 |
| Overall | 3 | 2.86 | ||
| Homozygous and VTE + | ||||
| Men | ||||
| 20-24 | 0.13 | 502 | 1 | 0.07 |
| 25-39 | 0.16 | 1069 | 0 | 0.17 |
| 40-54 | 0.65 | 661 | 0 | 0.43 |
| 55-69 | 1.80 | 227 | 2 | 0.41 |
| 70+ | 4.71 | 46 | 0 | 0.22 |
| Women | ||||
| 20-24 | 0.36 | 734 | 1 | 0.26 |
| 25-39 | 0.40 | 1611 | 1 | 0.64 |
| 40-54 | 0.79 | 1014 | 1 | 0.80 |
| 55-69 | 1.56 | 376 | 0 | 0.59 |
| 70+ | 4.67 | 61 | 0 | 0.28 |
| Overall | 6 | 3.87 | ||
| Heterozygous and VTE – | ||||
| Men | ||||
| 20-24 | 0.13 | 221 | 0 | 0.03 |
| 25-39 | 0.16 | 540 | 0 | 0.09 |
| 40-54 | 0.65 | 344 | 1 | 0.22 |
| 55-69 | 1.80 | 167 | 2 | 0.30 |
| 70+ | 4.71 | 25 | 0 | 0.12 |
| Women | ||||
| 20-24 | 0.36 | 310 | 0 | 0.11 |
| 25-39 | 0.40 | 722 | 0 | 0.29 |
| 40-54 | 0.79 | 435 | 1 | 0.34 |
| 55-69 | 1.56 | 171 | 0 | 0.27 |
| 70+ | 4.67 | 9 | 0 | 0.04 |
| Overall | 4 | 1.81 | ||
| Heterozygous and VTE + | ||||
| Men | ||||
| 20-24 | 0.13 | 420 | 0 | 0.05 |
| 25-39 | 0.16 | 930 | 1 | 0.15 |
| 40-54 | 0.65 | 498 | 0 | 0.32 |
| 55-69 | 1.80 | 203 | 1 | 0.37 |
| 70+ | 4.71 | 37 | 0 | 0.17 |
| Women | ||||
| 20-24 | 0.36 | 538 | 2 | 0.19 |
| 25-39 | 0.40 | 1225 | 5 | 0.49 |
| 40-54 | 0.79 | 728 | 1 | 0.58 |
| 55-69 | 1.56 | 286 | 3 | 0.45 |
| 70+ | 4.67 | 57 | 1 | 0.27 |
| Overall | 14 | 3.04 |
Per 1000 patient-years. Data obtained from Naess et al.17
SIR for the 4 groups of relatives selected on the basis of genotype and clinical presentation of the proband (reported on the x-axis). Vertical bars represent 95% CI. The horizontal dashed line set at SIR = 1 represents the line of equal incidence of VTE in the study population and in the general population of same age and sex.
SIR for the 4 groups of relatives selected on the basis of genotype and clinical presentation of the proband (reported on the x-axis). Vertical bars represent 95% CI. The horizontal dashed line set at SIR = 1 represents the line of equal incidence of VTE in the study population and in the general population of same age and sex.
Discussion
This study shows that the selection of families with either FVL or PT20210A according to the genotype and clinical presentation of the proband (ie, the family member who was first referred for thrombophilia work-up) influences the risk for VTE in relatives. The highest risk was found in kindreds with probands heterozygous for FVL or PT20210A and symptomatic for VTE. Indeed, relatives belonging to these kindreds had a fourfold higher risk for VTE than those with homozygous probands without VTE. These results did not substantially change when we considered homozygous probands only, excluding probands with combined polymorphisms (data not shown). The index event bias highlighted in this study is a type of selection bias in which the contribution to the disease of some specific causes (in this case FVL or PT20210A) may vary according to the presence of other (yet unknown) causes for the disease.18 This bias has been claimed as a possible explanation for the paradox of the absence of increased risk for disease recurrence in the presence of the same risk factors at the first event of the same disease,19-21 and it can be applied in this context to explain the different risk for VTE in family members carrying the same genetic polymorphism.
Our study confirms a recent observation of an increased risk for VTE in relatives with thrombophilia only when their probands were symptomatic for VTE.13 However, in that study, only a minority of probands were homozygous or compound heterozygous for FVL or PT20210A, and therefore the effect of the combination of proband’s genotype and clinical manifestations on the risk for VTE in relatives could not be evaluated. In comparison with a previous multicenter family study12 in which most of the FVL or PT20210A families were selected from heterozygous probands with a history of VTE, the overall absolute risk for VTE found in this study is lower (0.77 vs 1.41 per 1000 patient-years, respectively). However, when in this study the subgroup of relatives belonging to kindreds with heterozygous and symptomatic probands was selected, the incidence of VTE was very similar (1.53 per 1000 patient-years). Similar figures were also obtained in the largest group of heterozygous FVL relatives selected in the same way (1.63 vs 1.90 per 1000 patient-years, respectively). This further supports the influence of selection criteria based on genotype and clinical presentation of the proband on the VTE risk estimates in family studies. In 2 previous family studies (one carried out in Italy and the other in The Netherlands), the annual incidence of VTE in FVL relatives selected from kindreds with probands symptomatic for VTE and mostly heterozygous for the polymorphism was 2.80 and 4.50 per 1000 patient-years, respectively.22,23 However, in both studies, the follow-up started at age 15 years because VTE rarely occurs in children. Using the same criterion in our study, the annual incidence of VTE in heterozygous FVL relatives belonging to families with heterozygous symptomatic probands became 2.40 per 1000 patient-years, thus approaching the figures of those studies.
The effect of selection criteria on the risk for VTE was already postulated in the past for carriers of inherited deficiencies of the naturally occurring anticoagulants. In 1987, among a large group of healthy blood donors, Miletich et al identified 79 individuals with low protein C levels, none of whom had a personal or family history of VTE.24 This contrasted with the results of previous studies on protein C–deficient families, in which the risk for VTE was very high.25,26 Both findings were clearly related to a selection bias: the risk for thrombosis was underestimated when individuals were recruited among healthy blood donors and overestimated when they were recruited among thrombophilic families, as demonstrated by studies on unselected outpatients27 or by those comparing different patients’ selection criteria.28
Interestingly, we observed in this study that symptomatic relatives of homozygous or heterozygous probands (mostly with FVL) who had only superficial vein thrombosis also suffered from superficial vein thrombosis, and only 1 of them had VTE. Whether these families represent a particular subset of FVL carriers with a peculiar predisposition to superficial vein thrombosis can only be speculated.
When incidence rates of our study population of relatives were standardized to those of sex- and age-specific strata of the general population, only relatives belonging to kindreds with heterozygous probands symptomatic for VTE had a 4.5-fold significantly higher incidence of VTE, whereas those belonging to families with homozygous probands asymptomatic for VTE had a rate similar to that of the general population. This finding suggests that family members should be tested only if the proband is symptomatic for VTE, and in particular, when heterozygous for FVL or PT20210A. In these relatives, a high penetrance of the genetic defect can be hypothesized as likely because of the coexistence of other unknown genetic defects. In contrast, testing relatives of probands with homozygous FVL or PT20210A or combined polymorphisms and no VTE is not warranted, as previously observed.13,29,30
Among the limitations of this study is its retrospective design. However, the criteria used to select the study population should have minimized the negative effects of the retrospective design. First, probands were excluded from the analysis. Second, all the VTE episodes among relatives were objectively documented. Third, the personal and family histories of thrombosis were obtained through a validated questionnaire before obtaining the results of thrombophilia screening, and therefore the effects of the ascertainment bias were limited. Finally, the follow-up ended at the date of visit to the centers, excluding the possibility of an underestimation of the VTE risk related to antithrombotic prophylaxis during high-risk situations or particular behaviors after the result of genotyping was available (eg, avoidance of oral contraceptives or postsurgical antithrombotic prophylaxis in carriers of FVL or PT20210A).
The possibility that asymptomatic relatives were less motivated to reach the center for genotyping (thus leading to an overestimation of the true VTE risk) cannot be ruled out, but it is unlikely to have affected the different VTE risk in relatives selected according to the proband’s characteristics. Another limitation of this study is that the relatively small number of VTE events among relatives may have affected the precision of the risk estimates. This is true for all categories of relatives selected on the basis of the genotype and clinical presentation of the proband, except for those belonging to families with heterozygous probands with VTE, for whom a clear 4.5-fold higher risk for VTE was found compared with the general population of same age and sex. The possibility that pooling together relatives homozygous and heterozygous for FVL or PT20210A has affected VTE risk estimates is unlikely because of the adjustment of the risk estimates for the type of polymorphism and genotype of relatives in the multivariable Cox model.
In conclusion, our study underlines the influence of patients’ selection on the risk for VTE in family members with FVL or PT20210A. This example of index event bias can in part explain the different risk for VTE in families sharing the same genetic defect. Further studies are required to confirm these results.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
There is an Inside Blood commentary on this article in this issue.
Authorship
Contribution: P.B. designed the study, collected data, performed statistical analysis, and wrote the initial draft of the manuscript; V.D.S. collected data, contributed to the interpretation of results, and revised the manuscript; S.M.P., D.T., C.L., and P.S. collected data and revised the manuscript; E.R. collected data; G.C. collected data, contributed to the interpretation of results, and revised the manuscript; M.C. collected data; I.M. designed the study, collected data, contributed to the interpretation of results, and revised the manuscript; and all authors were responsible for approval of the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Paolo Bucciarelli, A. Bianchi Bonomi Hemophilia and Thrombosis Center, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Via Pace, 9-20122 Milan, Italy; e-mail: bucciarelli@policlinico.mi.it.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal