Abstract
Alloreactivity of donor lymphocytes leads to graft-versus-host disease (GVHD) contributing to significant morbidity and mortality following allogeneic hematopoietic cell transplantation (HCT). Within the past decade, significant progress has been made in elucidating the mechanisms underlying the immunologic dysregulation characteristic of GVHD. The recent discoveries of different cell subpopulations with immune regulatory function has led to a number of studies aimed at understanding their role in allogeneic HCT and possible application for the prevention and treatment of GVHD and a host of other immune-mediated diseases. Preclinical animal modeling has helped define the potential roles of distinct populations of regulatory cells that have progressed to clinical translation with promising early results.
Introduction
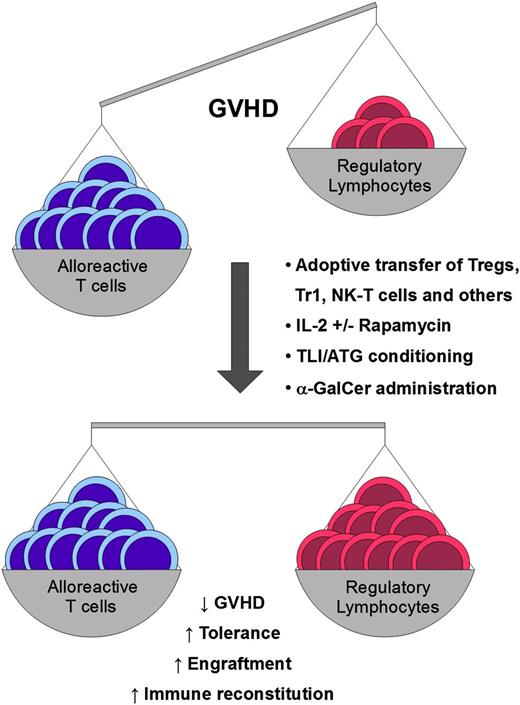
Immunologic reconstitution is a critical process following hematopoietic cell transplantation (HCT). Dysregulation may lead to immune-mediated destruction of host tissues resulting in graft-versus-host disease (GVHD) and opportunistic infections. Deeper understanding and manipulation of immune regulatory mechanisms to control dysregulated immune responses have enormous potential for improving outcomes following allogeneic HCT and in a number of other clinical situations. Recently, the discovery of different populations of regulatory cells led researchers to focus on the role of regulatory cells in allogeneic HCT. Several studies have explored the mechanisms underlying regulatory cell function, with the aim of extending knowledge on immunologic aspects of allogeneic HCT and translating these findings to the clinic. Regulatory T cells (Tregs) and, more recently, natural killer T (NK-T) cells have been studied extensively in the context of allogeneic HCT. Furthermore, there is increasing evidence that myeloid-derived suppressor cells, mesenchymal stem cells, and regulatory B cells can play a significant role in posttransplant immune regulation. In this review, we will focus on CD4+CD25+FoxP3+ Tregs, T regulatory type 1 (Tr1) cells, and NK-T cells because they have been widely studied in preclinical models and extended to the clinic (Figure 1). The aim of this review is to update the newest strategies to enhance the potential of Tregs for clinical benefit and highlight the results of their first clinical applications. In addition, we will discuss the immunoregulatory role of NK-T cells and their significance in the development of transplant tolerance.
Different clinical approaches can be applied to impact the immunologic balance between alloreactive donor T cells and regulatory lymphocytes. α-GalCer, α-galactosylceramide; ATG, antithymocyte globulin; IL, interleukin; TLI, total lymphoid irradiation.
Different clinical approaches can be applied to impact the immunologic balance between alloreactive donor T cells and regulatory lymphocytes. α-GalCer, α-galactosylceramide; ATG, antithymocyte globulin; IL, interleukin; TLI, total lymphoid irradiation.
Regulatory T cells
Tregs are a subset of CD4+ T cells that can suppress proliferation and effector functions of many different cells such as T cells, B cells, NK cells, and antigen-presenting cells.1 Tregs express the α chain of the IL-2 receptor (CD25) and a nuclear transcription factor termed forkhead box P3 (FoxP3)2-4 whose deficiency causes dramatic immunologic disease in both animal models and humans.5-7 In spite of a large number of studies, the exact mechanism through which Tregs control immune responses has not been fully elucidated. Treg function appears to be cytokine or contact mediated. Several studies showed that IL-10, transforming growth factor β (TGF-β), and IL-35 have been implicated in enhancing suppression8-12 ; whereas CTLA-4, LAG-3, CD39, and granzymes play an important role in the contact-dependent immune control.13-18
The ability of Tregs to suppress effector cell proliferation and function makes these cells extremely promising for cellular therapy of immune diseases. Many studies have been performed to translate the in vitro results to in vivo animal models. In the setting of allogeneic HCT, infusion of donor-derived conventional CD4+ and CD8+ T cells (Tcons) causes an immune-mediated destruction of host tissues leading to acute and chronic GVHD. In a number of different allogeneic HCT animal models, the addition of highly purified CD4+CD25+FoxP3+ Tregs resulted in suppression of GVHD.19-22
The paucity of Tregs in the peripheral blood is one of the major obstacles for the application of these models and eventual clinical translation. Following the finding that Tregs proliferate in vivo in the allogeneic setting, their infusion before Tcons allowed for the use of a smaller number of Tregs maintaining GVHD suppression.23 Another approach widely explored to obtain a larger number of functional Tregs is through ex vivo expansion. Different groups demonstrated that Tregs expand in vitro, usually after activation by CD3/CD28 and in the presence of TGF-β and antigen-presenting cells.22,24 With these conditions, after a 2- to 3-week culture period, it is possible to obtain a significant expansion of both mouse and human Tregs. The major limitation of this approach is the fact that Tcons expand preferentially in these cultures.25 To avoid the undesired Tcon expansion, different strategies are under investigation, such as the use of rapamycin, the exclusion of the Tcons from the Treg inoculum, and isolation of naïve CD4+CD25+CD45RA+ Tregs prior to expansion.26-28
Naïve conventional CD4+ T cells can rapidly express a regulatory phenotype (CD25+FoxP3+) following T-cell receptor (TCR) and TGF-β stimulation.29-31 These “induced” Tregs (iTregs) can exert suppressive activity but maintain the production of proinflammatory cytokines and show a different gene expression profile in comparison with naturally occurring thymus-derived Tregs.32,33 Recently, new insights regarding FoxP3 gene methylation status and expression of different markers such as Helios and neuropilin 1 have been contributing to better defining the differences between naturally occurring thymus-derived Tregs and iTregs.34-39 Many researchers are exploring the possibility of generating larger numbers of Tregs in vitro. Unfortunately, ex vivo human iTreg suppressive activity appears less stable in some preclinical models, suggesting that FoxP3 expression is not the only factor that naïve CD4+ T cells require to convert into functional suppressive cells.40 The lack of knowledge regarding in vivo iTreg phenotype stability, function, persistence, and impact on GVHD onset and severity is limiting the application of iTregs in clinical trials.
Several reports have shown that Tregs can play a key role in tumor progression contributing to immunologic escape41,42 ; therefore, an important concern in the application of Tregs in the allogeneic HCT setting is the possible suppression of immune-mediated graft-versus-tumor (GVT) responses. In HCT animal models, the adoptive transfer of freshly isolated Tregs preserved GVT reactions in some model systems.2,20,43 The mechanism underlying this concept has to do with Treg-mediated suppression of Tcon proliferation but not activation. In the setting where there is a relatively high T-cell precursor frequency for alloantigens (eg, following allogeneic HCT, especially across histocompatibility barriers), expansion of cytotoxic T cells is less important for the exertion of GVT effects. In the opposite setting (eg, following vaccination to a rare tumor antigen where the T-cell precursor frequency is low and T-cell expansion is required for a biological effect), Tregs appear to suppress these immune-mediated antitumor effects.44,45 Therefore, following allogeneic transplantation where there is immune activation, often relatively high T-cell precursor frequencies for alloantigens, both major and minor, and low tumor burden appears to be an ideal setting in which to test Treg function.
Recently, the first clinical studies have been published showing that the adoptive transfer of Tregs can control GVHD. The group from Perugia demonstrated that by introducing freshly isolated donor-type Tregs after myeloablative conditioning and before the infusion of a megadose of CD34+ cells and Tcons, haploidentical transplantation is possible without any immunosuppression and with a very low rate of acute and chronic GVHD.46 In the first protocol, transplant-related mortality was substantial and felt to be mainly due to early infections and toxicity of the conditioning regimen, suggesting the need for improvements in the preparative therapy. Nevertheless, the infusion of up to 2 × 106 CD25+-selected Tregs per kg showed no toxicity, permitted the infusion of up to 1 × 106 Tcons per kg, boosting immune recovery, and appeared to preserve GVT responses because the disease recurrence rate was extremely low despite the fact that all the transplanted patients were affected by high-risk leukemias. Prior studies have established that infusion of this number of Tcons without Tregs results in prohibitive GVHD following haploidentical transplantation without immune suppression, providing definitive evidence of Treg function. A second study from the University of Minnesota confirmed that the adoptive transfer of Tregs is without apparent toxicity and can reduce the risk of acute GVHD.47 This group demonstrated that umbilical cord third-party Tregs can be expanded ex vivo, and their application in the double cord transplant setting appeared to reduce GVHD risk in comparison with a historical control group. These preliminary studies demonstrate that cellular therapy with Tregs is safe and feasible and provides the first evidence of Treg efficacy in GVHD prevention and GVT persistence.
The importance of enhancing Treg function and numbers to reduce GVHD led to the development of several strategies to expand this cell population in vivo. Treatment with IL-2 and/or rapamycin allowed for the expansion of Tregs maintaining the suppression of Tcons in different animal models and in human studies.48-51 Recently, investigators from the Dana Farber Cancer Center explored the application of low-dose IL-2 treatment of refractory chronic GVHD with the hypothesis that such treatment would result in preferential expansion of Tregs, which are exquisitely sensitive to IL-2 yet do not produce this cytokine. They demonstrated that IL-2, at the daily dose of 1 × 106 units/m2, was reasonably well tolerated, produced in vivo Treg expansion, and induced clinical responses reducing chronic GVHD in 13 of 23 evaluable patients.52 An alternative approach to enhance Treg numbers is through the adoptive transfer of highly purified donor-derived Tregs, which is being applied in the setting of chronic GVHD by several groups (NCT01911039, NCT01903473). Trzonkowski et al reported 2 patients affected by GVHD that were treated with adoptive transfer of ex vivo–expanded donor-derived Tregs as adjuvant therapy. The treatment resulted in a significant clinical response that was more evident in the patient with chronic GVHD.53
Another possible approach to the clinical translation of Tregs comes from investigators at the University of Milan who described a population of CD4+ Tregs that produce high amounts of IL-10 yet do not constitutively express FoxP3.54-56 These cells, termed Tr1, showed the ability to suppress immune response and restore tolerance in ex vivo and in vivo models.56-58 Human Tr1 cells can also be generated from IL-10–enriched T-cell cultures and expanded in vitro.59-61 Recently, Gagliani et al more completely characterized mouse and human Tr1 cells by the constitutive and persistent expression of CD49b and LAG3.62 This finding allows for more effective selection of Tr1 cells for future clinical applications in GVHD suppression, tolerance induction, and immune recovery after HCT.
Despite the promising early pilot clinical trials of Tregs, there are still major issues to be solved regarding optimal cellular source, cell purity, numbers of cells required for biological effect, antigen specificity, activation status, phenotype stability, homing, survival, and impact on important biological functions such as immunity and GVT responses. New insights about the expression and the relevance of surface markers such as CD62L, LAG3, and major histocompatibility complex class II molecules can help refine Treg selection and function.17,63-66 Studies aimed at understanding the impact of Treg derived from different donor sources on GVHD prevention and treatment can extend the application of this cellular therapy. Furthermore, studies showed that in vitro–primed antigen-specific Tregs can be developed with specific suppressive activity,67-69 so particular effort is needed to identify common antigens that trigger GVHD and can be used for clinical translation. Major challenges include the individual variability between patients; however, the recent introduction of new techniques for the analysis of the TCR repertoire could represent an extremely useful tool to overcome such limitations.70 Many groups are also exploring the possibility that Tregs could induce transplant tolerance providing a promising tool for enhancing donor engraftment after nonmyeloablative conditioning or possibly for reducing or treating solid organ graft rejection. Therefore, the door for Treg clinical translation has opened encouraging additional trials in several clinical settings.
NK-T cells
Another subset of T lymphocytes that coexpress NK and T-cell markers has been shown to have potent immunomodulatory activities mainly through the rapid production of cytokines such as IL-4, IL-10, and IL-13.71 NK-T cells suppress different autoimmune and alloimmune reactions in both animal models and humans, setting the stage for clinical translation.72 Invariant NK-T (iNK-T) cells express the TCRα Vα24-Jα18 in humans and recognize the glycolipid α-GalCer through their TCR with high affinity.
Adoptive transfer of both donor and host NK-T cells has been investigated where it was found that these cells are capable of suppressing GVHD in mice.73-75 Compared with Tregs, even lower numbers of NK-T cells can prevent GVHD through inducing a T helper 2–biased immune response.75
Recent retrospective clinical data strongly support the beneficial immunologic effects of NK-T cells in the setting of allogeneic HCT in humans. Chaidos and others showed in a multivariate analysis that a higher graft CD4– iNK-T cell dose was associated with a significantly lower risk of acute GVHD.76 Similarly, Rubio and others found that low peripheral blood iNK-T/T-cell ratios posttransplant was an independent factor associated with the occurrence of acute GVHD.77
One clinical approach to the translation of these concepts came from the studies of Strober et al where they found that a preparative regimen for allogeneic HCT using TLI in combination with ATG resulted in alteration of conventional T cells and marked reduction in GVHD risk.78 NK-T cells are relatively radioresistant and express high levels of bcl-2. Following exposure to TLI, it was found in these studies that TLI/ATG-prepared animals had dramatically higher ratios of host NK-T cells/Tcons and could be transplanted with 1000 times the number of conventional T cells as compared with total body irradiation–conditioned animals, which would otherwise result in lethal GVHD. In this context, it has been shown that host NK-T cells and donor Tregs interact synergistically in a way that host NK-T cells lead to an expansion of donor Tregs in an IL-4–dependent manner.79
The results from these preclinical animal models have been successfully translated to patients with hematologic malignancies who underwent allogeneic HCT after conditioning with TLI/ATG where they experienced a very low risk of acute GVHD and transplant-related mortality.80 More recently, 2 larger clinical trials confirmed independently the protective nature of this conditioning regimen.81,82 In these studies, the incidence of acute GVHD was as low as 2% and 10% for patients receiving grafts from related and unrelated donors, respectively. Nonrelapse mortality was <4%, reflecting the safety of this approach using the reduced-intensity preparative regimen. Hence, conditioning with TLI/ATG might be considered an alternative treatment option for the elderly, comorbid, and heavily pretreated patient populations. In addition, these clinical studies provided evidence for sustained GVT effects. Currently, several clinical phase 2 trials are ongoing to evaluate the TLI/ATG-conditioning regimen for the treatment of myelodysplastic and myeloproliferative disorders (NCT00185796), as well as lymphoid malignancies (NCT00896493, NCT01566656). Another clinical phase 2 trial evaluating the impact of TLI/ATG conditioning followed by allogeneic HCT as consolidation to autologous HCT for the treatment of patients with poor-risk diffuse large B-cell lymphoma has been recently completed (NCT00482053).
The iNK-T cell–activating glycolipid α-GalCer can induce in vivo expansion of regulatory cells in mice that effectively prevented acute GVHD.83 This concept has been translated to the clinic in an ongoing multicenter phase 1/2 clinical trial (NCT01379209) investigating the liposomal formulation of α-GalCer (RGI-2001) in patients undergoing myeloablative allogeneic HCT for the treatment of hematologic malignancies.
Furthermore, it has been demonstrated in animal models that TLI/ATG conditioning and transplantation of donor hematopoietic cells can induce tolerance of solid organ allografts.84,85 A first patient was successfully treated with combined kidney and HCT at Stanford in 2005, allowing for the withdrawal of all immunosuppressive medications after 6 months without signs of allograft rejection, with persistent mixed chimerism, and without signs of GVHD.86 More recently, it has been shown by Scandling and others in a pilot clinical study that TLI/ATG conditioning promoted the induction of tolerance in a majority of patients after combined kidney and HCT, allowing for withdrawal of immunosuppressive medications.87,88 As shown in previous animal models, tolerance induction was associated with increased peripheral blood Treg/T-cell and NK-T/T-cell ratios, and lymphocytes from patients off immunosuppressive drugs showed a significantly reduced response to donor alloantigens in vitro.
The concept of immune regulation, suppression of alloreactivity, and induction of tolerance through manipulation of immune regulatory cells in the context of allogeneic HCT has been successfully transferred to the clinic. Further preclinical and clinical studies are necessary to elucidate the mechanisms underlying their potent immunoregulatory features to optimize these promising approaches for our patients. It is clear that the concepts initially developed in preclinical animal models are beginning to bear fruit in the clinic with broad potential applications.
Conclusion
Regulation of immune function following allogeneic HCT is a complex process involving a variety of important humoral and cellular mechanisms. The development of strategies to enhance immune regulatory cell numbers and function, as well as adoptive transfer of regulatory cell populations, holds significant promise for improving outcomes for patients undergoing allogeneic HCT and perhaps a myriad of other immune-mediated conditions. The complexity of the biology of immune regulation, the paucity of regulatory cell populations, and the lack of knowledge about functional mechanisms and optimal methodologies for manipulation are still to be overcome. However, the recent results deriving from the first clinical approaches adapted from animal modeling have demonstrated the biological impact of these cell populations and the feasibility of clinical translation. Further clinical trials are needed to definitively establish the potential of these cells in controlling immune dysregulation and their applicability in allogeneic HCT, as well as extension into other clinical settings.
Acknowledgments
This work was supported in part by the National Institutes of Health (CAP01 HL075462 and CAP01 CA80006) (R.S.N.), the Deutsche Krebshilfe (D.S.), and the Fondazione Italiana per la Ricerca sul Cancro (A.P.).
Authorship
Contribution: D.S., A.P., and R.S.N. researched and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Robert S. Negrin, Professor of Medicine, Center for Clinical Sciences Research Building, Room 2205, 269 Campus Dr, Stanford, CA 94305; e-mail: negrs@stanford.edu.
References
Author notes
D.S. and A.P. contributed equally to this study.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal